Abstract
Background
Iatrogenic cerebral arterial gas embolism (CAGE) is an uncommon but potentially a fatal condition. Hyperbaric oxygen (HBO2) therapy is the only definitive treatment for patients with CAGE presenting with acute neurologic deficits.
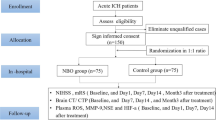
Methods
We reviewed medical records and neuroimaging of consecutive CAGE patients treated with HBO2 at a state referral hyperbaric facility over a 22-year period. We analyzed the effect of demographics, source of intra-arterial gas, signs and symptoms, results of imaging studies, time between event and HBO2 treatment, and response to HBO2 treatment in 36 consecutive patients. Favorable outcome was defined by complete resolution or improvement of CAGE signs and symptoms at 24 h after HBO2 treatment. Unfavorable outcome was defined by unchanged or worsened neurologic signs and symptoms or in hospital death.
Results
A total of 26 (72%) of the 36 patients had favorable outcome. Patients with favorable outcome were younger compared to those with unfavorable outcome (mean age [years, SD] 44.7 ± 17.8 vs. 58.1 ± 24.1, p = 0.08). Cardiopulmonary symptoms were significantly more common in CAGE related to venous source of gas compared to arterial source (p = 0.024) but did not influence the rate of favorable outcomes. Adjusted multivariate analysis demonstrated that time from event to HBO2 ≤6 h (positively) and the presence of infarct/edema on head computerized tomography (CT)/magnetic resonance imaging (MRI) before HBO2 (negatively) were independent predictors of favorable outcome at 24 h after HBO2 treatment [odds ratio (OR) 9.08 confidence interval (CI) (1.13–72.69), p = 0.0376, and (OR) 0.034 (CI) (0.002–0.58), p = 0.0200, respectively]. Two of the 36 patients were treated with thrombolytics because of acute focal deficits and suspected ischemia—one with intravenous and the second with intra-arterial thrombolysis. The latter patient developed fatal intracerebral hemorrhage.
Conclusions
A high proportion of CAGE patients treated with HBO2 had favorable outcomes. Time-to-HBO2 ≤6 h increased the odds of favorable outcome, whereas the presence of infarct/edema on CT/MRI scan before HBO2 reduced the odds of a favorable outcome. Timely diagnosis and differentiation from thrombo-embolic ischemic events appears to be an important determinant of successful HBO2 treatment.
Similar content being viewed by others
References
Thomas R, Thangakunam B, Cherian RA, Gupta R, Christopher DJ. Cerebral air embolism complicating CT-guided trans-thoracic needle biopsy of the lung. ClinRespir J. 2011;5(2):e1–3. doi:10.1111/j.1752-699X.2010.00229.x.
Heckmann JG, Lang CJ, Kindler K, Huk W, Erbguth FJ, Neundorfer B. Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med. 2000;28(5):1621–5.
Pandurangadu AV, Paul JA, Barawi M, Irvin CB. A Case Report of Cerebral Air Embolism after Esophagogastroduodenoscopy: Diagnosis and Management in the Emergency Department. J Emerg Med. 2011 [Epub ahead of print].
Müller MC, Lagarde SM, Germans MR, Juffermans NP. Cerebral air embolism after arthrography of the ankle. Med SciMonit. 2010;16(7):CS92–4.
Finsterer J, Stöllberger C, Bastovansky A. Cardiac and cerebral air embolism from endoscopic retrograde cholangio-pancreatography. Eur J Gastroenterol Hepatol. 2010;22(10):1157–62. Review.
Forsberg U, Jonsson P, Stegmayr C, Stegmayr B. Microemboli developed during haemodialysis pass the lung barrier and may cause ischaemic lesions in organs such as the brain. Nephrol Dial Transplant. 2010;25(8):2691–5. Epub 2010 Mar 19.
Gerriets T, Schwarz N, Sammer G, Baehr J, Stolz E, Kaps M, Kloevekorn WP, Bachmann G, Schönburg M. Protecting the brain from gaseous and solid micro-emboli during coronary artery bypass grafting: a randomized controlled trial. Eur Heart J. 2010;31(3):360–8.
Nishiyama T, Hanaoka K. Gas embolism during hysteroscopy. Can J Anaesth. 1999;46(4):379–81.
Gupta R, Vora N, Thomas A, Crammond D, Roth R, Jovin T, Horowitz M. Symptomatic cerebral air embolism during neuro-angiographic procedures: incidence and problem avoidance. Neurocrit Care. 2007;7(3):241–6.
Taylor SP, Hoffman GM. Gas embolus and cardiac arrest during laparoscopic pyloromyotomy in an infant. Can J Anaesth. 2010;57(8):774–8.
Gesell L. Hyperbaric oxygen therapy indications. 12th ed. Undersea and hyperbaric medical society: Durhan; 2008. p. 9–12.
Weiss KL, Macura KJ, Ahmed A. Cerebral air embolism: Acute imaging. J Stroke Cerebrovasc Dis. 1998;7(3):222–6.
Tanaka R, Shimada Y, Shimura H, Oizumi H, Hattori N, Tanaka S. Predominant Vasogenic Edema in a Patient with Fatal Cerebral Air Embolism. J Stroke Cerebrovasc Dis. 2010 [Epub ahead of print].
Hodgson M, Beran RG, Shirtley G. The role of computed tomography in the assessment of neurologic sequelae of decompression sickness. Arch Neurol. 1988;45(9):1033–5.
Muth CM, Shank ES. Gas embolism. New Engl J Med. 2000;342(7):476–82.
Jorens PG, Van Marck E, Snoeckx A, Parizel P. Nonthrombotic pulmonary embolism. Eur Resp J. 2009;34:452–72.
Boussuges A, Blanc P, Molenat F, Bergmann E, Sainty JM. Prognosis in iatrogenic gas embolism. Minerva Med. 1995;86(11):453–7.
Benson J, Adkinson C, Collier R. Hyperbaric oxygen therapy of iatrogenic cerebral arterial gas embolism. Undersea Hyperb Med. 2003;30(2):117–26.
U.S. Navy Diving Manual. Revision 5. SS521-AG-PRO-010, 0910-LP-103-8009. Published by Direction of the Commander, Naval Sea Systems Command, 15 August 2005. U.S. Government Printing Office, Washington DC 20402.
Blanc P, Boussuges A, Henriette K, Sainty JM, Deleflie M. Iatrogenic cerebral air embolism: importance of an early hyperbaric oxygenation. Intensive Care Med. 2002;28(5):559–63.
vanHulst RA, Drenthen J, Haitsma JJ, Lameris TW, Visser GH, Klein J, Lachmann B. Effects of hyperbaric treatment in cerebral air embolism on intracranial pressure, brain oxygenation, and brain glucose metabolism in the pig. Crit Care Med. 2005;33(4):841–6.
Bitterman H, Melamed Y. Delayed hyperbaric treatment of cerebral air embolism. Isr J Med Sci. 1993;29(1):22–6.
Mader JT, Hulet WH. Delayed hyperbaric treatment of cerebral air embolism: report of a case. Arch Neurol. 1979;36(8):504–5.
Armon C, Deschamps C, Adkinson C, Fealey RD, Orszulak TA. Hyperbaric Treatment of Cerebral Air Embolism Sustained During an Open-Heart Surgical Procedure. Mayo ClinProc. 1991;66:565–71.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tekle, W.G., Adkinson, C.D., Chaudhry, S.A. et al. Factors Associated with Favorable Response to Hyperbaric Oxygen Therapy among Patients Presenting with Iatrogenic Cerebral Arterial Gas Embolism. Neurocrit Care 18, 228–233 (2013). https://doi.org/10.1007/s12028-012-9683-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9683-3