Abstract
Background
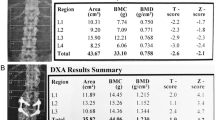
Low mineral mass and reduced bone strength with increased fracture risk are the main causes of morbidity in Thalassemia Major (TM). The pathogenesis is multifactorial and includes ineffective erythropoiesis with medullary expansion, multiple endocrine dysfunctions, direct iron bone deposition, deferoxamine-induced bone dysplasia, and reduced physical activity associated with disease complications. Dual-energy X-ray absorptiometry (DXA) is the “gold standard” for bone mineral density (BMD) assessment and for bone strength and quality evaluation. This method identifies patients at greater risk of fragility fractures, guiding treatment and monitoring response to therapy. In TM, DXA shows limitations concerning BMD calculation accuracy and fracture risk prediction. One of the main challenges in the assessment of bone health in patients with TM is the accurate interpretation of densitometric results.
Purpose
This review investigates the major pitfalls in DXA implementation and interpretation in TM.
Methods
Available literature has been assessed.
Conclusions
DXA shows limitations in assessing bone mineral “status” in TM, especially in the paediatric population, due to the peculiar characteristics of bone architecture and deformities associated with the disease. A radiological technique adjustment in this population is mandatory.








Similar content being viewed by others
References
E. Voskaridou et al. A national registry of haemoglobinopathies in Greece: deducted demographics, trends in mortality and affected births. Ann. Hematol. 91, 1451–1458 (2012)
M. Baldini et al. Endocrine and bone disease in appropriately treated adult patients with beta-thalassemia major. Ann. Hematol. 89, 1207–1213 (2010)
M. Di Stefano et al. Bone mass and metabolism in thalassemic children and adolescents treated with different iron-chelating drugs. J. Bone Miner. Metab. 22, 53–57 (2004)
M.G. Vogiatzi et al. Bone disease in Thalassemia: a frequent and still unresolved problem. J. Bone Miner. Res. 24, 543–557 (2009)
E.B. Fung et al. Characterization of low bone mass in young patients with thalassemia by DXA, pQCT and markers of bone turnover. Bone 48, 1305–1312 (2011)
Y.G. Chen et al. Risk of fracture in transfusion-naïve thalassemia population: a nationwide population-based retrospective cohort study. Bone 106, 121–125 (2018)
A.A. Shamshirsaz et al. Bone mineral density in Iranian adolescents and young adults with β-thalassemia major. Pediatr. Hematol. Oncol. 24, 469–479 (2007)
W. Sutipornpalangkul et al. Prevalence of fractures among Thais with Thalassaemia syndromes. Singap. Med. J. 51(10), 817–821 (2010)
D.J. Weatherall, Fortnightly review: the thalassaemias. BMJ (1997). https://doi.org/10.1136/bmj.314.7095.1675
R. Haidar et al. Bone disease and skeletal complications in patients with β thalassemia major. Bone 48, 425–432 (2011)
M. Angastiniotis, A. Eleftheriou, Thalassaemic bone disease: an overview. Pediatr. Endocrinol. Rev. 6, 73–80 (2008)
J.A. Kanis et al. FRAXTM and the assessment of fracture probability in men and women from the UK. Osteoporos. Int. 19, 385–397 (2008)
P. Wong et al. Thalassemia bone disease: the association between nephrolithiasis, bone mineral density and fractures. Osteoporos. Int. 24, 1965–1971 (2013)
P. Mahachoklertwattana et al. Association between bone mineral density and erythropoiesis in Thai children and adolescents with thalassemia syndromes. J. Bone Miner. Metab. (2006). https://doi.org/10.1007/s00774-005-0661-0
P. Pootrakul, Relation between erythropoiesis and bone metabolism in thalassemia. J. Pediatr. Orthop. (1981). https://doi.org/10.1097/01241398-198112000-00054
T. Diamond et al. Osteoporosis in hemochromatosis: iron excess, gonadal deficiency, or others factors? Ann. Intern. Med. (1989). https://doi.org/10.7326/0003-4819-110-6-430
A. Filosa et al. Longitudinal monitoring of bone mineral density in thalassemic patients. Genetic structure and osteoporosis. Acta Paediatr. Int. J. Paediatr. (1997). https://doi.org/10.1111/j.1651-2227.1997.tb09019.x
R. Lala et al. Bone density and metabolism in thalassaemia. J. Pediatr. Endocrinol. Metab. 11(Suppl 3), 785–790 (1998)
B.K. Bielinski et al. Impact of disordered puberty on bone density in β-thalassaemia major. Br. J. Haematol. 120, 353–358 (2003)
M. L. G. Anapllotou et al. The contribution of hypogonadism to the development of osteoporosis in thalassaemia major: new therapeutic approaches. Clin. Endocrinol. (Oxf.) (2008). https://doi.org/10.1111/j.1365-2265.1995.tb01876.x
M. D. Cappellini et al. (eds), Guidelines for the Management of Transfusion Dependent Thalassemia (TDT) (Thalassemia International Federation, Nicosia, 2014)
Y.L. Chan et al. Patterns of bone diseases in transfusion-dependent homozygous thalassaemia major: predominance of osteoporosis and desferrioxamine-induced bone dysplasia. Pediatr. Radiol. 32, 492–497 (2002)
E.M. Lewiecki, Update on bone density testing. Curr. Osteoporos. Rep. (2005). https://doi.org/10.1007/s11914-996-0016-3
H.E. Meema, H. Meindok, Advantages of peripheral radiogrametry over dual-photon absorptiometry of the spine in the assessment of prevalence of osteoporotic vertebral fractures in women. J. Bone Miner. Res. 7(8), 897–903 (1992)
C.M. Gordon et al. 2013 pediatric position development conference: executive summary and reflections. J. Clin. Densitom. 17, 219–224 (2014)
J.A. Shepherd et al. Executive Summary of the 2015 ISCD Position Development Conference on Advanced Measures From DXA and QCT: fracture prediction beyond BMD. J. Clin. Densitom. (2015). https://doi.org/10.1016/j.jocd.2015.06.013
E. Voskaridou, E. Terpos, New insights into the pathophysiology and management of osteoporosis in patients with beta thalassaemia. Br. J. Haematol. (2004). https://doi.org/10.1111/j.1365-2141.2004.05143.x
R.I. Gafni, J. Baron, Overdiagnosis of osteoporosis in children due to misinterpretation of dual-energy X-ray absorptiometry (DEXA). J. Pediatr. (2004). https://doi.org/10.1016/j.jpeds.2003.08.054
E.B. Fung et al. Fracture prevalence and relationship to endocrinopathy in iron overloaded patients with sickle cell disease and thalassemia. Bone 43, 162–168 (2008)
J. A. Kanis, Osteoporosis III: diagnosis of osteoporosis and assessment of fracture risk. Lancet (2002). https://doi.org/10.1016/S0140-6736(02)08761-5
M.G. Vogiatzi et al. Prevalence of fractures among the Thalassemia syndromes in North America. Bone 38, 571–575 (2006)
N. Bishop et al. Fracture prediction and the definition of osteoporosis in children and adolescents: The ISCD 2013 Pediatric Official Positions. J. Clin. Densitom. 17, 275–280 (2014)
P. Wong et al. Thalassemia bone disease: a 19-year longitudinal analysis. J. Bone Miner. Res. 29, 2468–2473 (2014)
F. Najafipour et al. A cross-sectional study of metabolic and endocrine complications in beta-thalassemia major. Ann. Saudi Med. 28(5), 361–366 (2008)
I. Aslan et al. Bone mineral density in thalassemia major patients from Antalya, Turkey. Int. J. Endocrinol. 2012, 573298 (2012)
A. Prentice et al. Uncritical use of bone mineral density in absorptiometry may lead to size- related artifacts in the identification of bone mineral determinants. Am. J. Clin. Nutr. (1994). https://doi.org/10.1093/ajcn/60.6.837
C.M. Gordon et al. Dual energy X-ray absorptiometry interpretation and reporting in children and adolescents: The 2007 ISCD Pediatric Official Positions. J. Clin. Densitom. 11, 43–58 (2008)
K.A. Ward et al. UK reference data for the Hologic QDR Discovery dual-energy x ray absorptiometry scanner in healthy children and young adults aged 6-17 years. Arch. Dis. Child. (2007). https://doi.org/10.1136/adc.2006.097642
N. Shaw, N. Crabtree, Bone density in children: what are we measuring? Arch. Dis. Child. (2019). https://doi.org/10.1136/archdischild-2019-316940
R.P. Heaney, Bone mineral content, not bone mineral density, is the correct bone measure for growth studies. Am. J. Clin. Nutr. 78, 350–351 (2003)
M.B. Leonard et al. Interpretation of whole body dual energy X-ray absorptiometry measures in children: comparison with peripheral quantitative computed tomography. Bone 34, 1044–1052 (2004)
L.A. Binkovitz, M.J. Henwood, Pediatric DXA: technique and interpretation. Pediatr. Radiol. 37, 21–31 (2007)
M.S. Fewtrell et al. Dual X-ray absorptiometry (DXA) of the lumbar spine in a clinical paediatric setting: does the method of size-adjustment matter? Bone 37, 413–419 (2005)
B.S. Zemel et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J. Clin. Endocrinol. Metab. 95, 1265–1273 (2010)
L.K. Bachrach et al. Clinical report—bone densitometry in children and adolescents. Pediatrics 127, 189–194 (2011)
L.K. Bachrach, Osteoporosis in children: still a diagnostic challenge. J. Clin. Endocrinol. Metab. 92, 2030–2032 (2007)
P.W. Brill et al. Deferoxamine-induced bone dysplasia in patients with thalassemia major. Am. J. Roentgenol. 156, 561–565 (1991)
T. Rand et al. Impact of spinal degenerative changes on the evaluation of bone mineral density with dual energy x-ray absorptiometry (DXA). Calcif. Tissue Int. 60, 430–433 (1997)
S. Desigan et al. Degenerative disc disease as a cause of back pain in the thalassaemic population: a case-control study using MRI and plain radiographs. Skelet. Radiol. 35, 95–102 (2006)
S. De Virgillis et al. Deferoxamine-induced growth retardation in patients with thalassemia major. J. Pediatr. 113, 661–669 (1988)
Y.L. Chan et al. Desferrioxamine-induced long bone changes in thalassaemic patients — radiographic features, prevalence and relations with growth. Clin. Radiol. 55, 610–614 (2000)
M.J. Hartkamp et al. Spinal deformities in deferoxamine-treated homozygous beta-thalassemia major patients. Pediatr. Radiol. 23, 525–528 (1993)
A. Naselli et al. Long-term follow-up of skeletal dysplasia in thalassaemia major. J. Pediatr. Endocrinol. Metab. 11(Suppl 3), 817–825 (1998)
T.L. Levin et al. Deferoxamine-induced platyspondyly in hypertransfused thalassemic patients. Pediatr. Radiol. 25(Suppl 1), S122–S124 (1995)
L.N. Grinberg et al. Hydroxyl radical generation in β-thalassemic red blood cells. Free Radic. Biol. Med. 18, 611–615 (1995)
T. Yamaza et al. Oxidative stress-induced DNA damage in the synovial cells of the temporomandibular joint in the rat. J. Dent. Res. (2004). https://doi.org/10.1177/154405910408300807
D.J. Peacock et al. Lateral bone density measurements in osteoarthritis of the lumbar spine. Ann. Rheum. Dis. (1996). https://doi.org/10.1136/ard.55.3.196
G. Jones et al. A longitudinal study of the effect of spinal degenerative disease on bone density in the elderly. J. Rheumatol. 22(5), 932–936 (1995)
P. Korovessis et al. Incidence of scoliosis in β-thalassemia and follow-up evaluation. Spine (Phila. Pa. 1976). 21, 1798–1801 (1996)
P.G. Korovessis et al. Prevalence of scoliosis in beta-thalassemia. J. Spinal Disord. 9, 170–173 (1996)
D.A. Papanastasiou et al. Correlative analysis of the sagittal profile of the spine in patients with β-thalassemia and in healthy persons. J. Spinal Disord. (2000). https://doi.org/10.1097/00002517-200004000-00004
J.C. Cheng et al. The effect of vertebral rotation of the lumbar spine on dual energy X-ray absorptiometry measurements: observational study. Hong Kong Med. J. 7(3), 241–245 (2001)
P.A. Tyler et al. The radiological appearances of thalassaemia. Clin. Radiol. 61, 40–52 (2006)
M. Yildiz, D. Canatan, Soft tissue density variations in thalassemia major: a possible pitfall in lumbar bone mineral density measurements by dual-energy X-ray absorptiometry. Pediatr. Hematol. Oncol. 22, 723–726 (2005)
E.E. Drakonaki et al. Bone marrow changes in beta-thalassemia major: quantitative MR imaging findings and correlation with iron stores. Eur. Radiol. 17, 2079–2087 (2007)
L.K. Bachrach et al. Bone mineral acquisition in healthy Asian, Hispanic, black, and Caucasian youth: a longitudinal study. J. Clin. Endocrinol. Metab. (1999). https://doi.org/10.1210/jc.84.12.4702
N.J. Crabtree et al. Amalgamated reference data for size-adjusted bone densitometry measurements in 3598 children and young adults—the ALPHABET Study. J. Bone Miner. Res. 32, 172–180 (2017)
N.J. Crabtree et al. Diagnostic evaluation of bone densitometric size adjustment techniques in children with and without low trauma fractures. Osteoporos. Int. 24, 2015–2024 (2013)
N.J. Crabtree et al. Dual-energy x-ray absorptiometry interpretation and reporting in children and adolescents: The Revised 2013 ISCD Pediatric Official Positions. J. Clin. Densitom. 17, 225–242 (2014)
R.J. Kuczmarski et al. CDC growth charts: United States. Adv. Data 1–27 (2000)
D.F. Short et al. Anthropometric models of bone mineral content and areal bone mineral density based on the bone mineral density in childhood study. Osteoporos. Int. (2015). https://doi.org/10.1007/s00198-014-2916-x
J.M. Kindler et al. Lumbar spine bone mineral apparent density in children: results from the bone mineral density in childhood study. J. Clin. Endocrinol. Metab. (2019). https://doi.org/10.1210/jc.2018-01693
C. Mølgaard et al. Whole body bone mineral content in healthy children and adolescents. Arch. Dis. Child. (1997). https://doi.org/10.1136/adc.76.1.9
J.P. Bonjour et al. Critical years and stages of puberty for spinal and femoral bone mass accumulation during adolescence. J. Clin. Endocrinol. Metab. 73, 555–563 (1991)
A. Arabi et al. Bone mineral density by age, gender, pubertal stages, and socioeconomic status in healthy Lebanese children and adolescents. Bone (2004). https://doi.org/10.1016/j.bone.2004.06.015
N. Di Iorgi et al. Update on bone density measurements and their interpretation in children and adolescents. Best. Pract. Res. Clin. Endocrinol. Metab. 32, 477–498 (2018)
N.J. Crabtree et al. The relationship between lean body mass and bone mineral content in paediatric health and disease. Bone 35, 965–972 (2004)
W. Högler et al. Importance of lean mass in the interpretation of total body densitometry in children and adolescents. J. Pediatr. (2003). https://doi.org/10.1016/S0022-3476(03)00187-2
M.A. Petit et al. Examining the developing bone: what do we measure and how do we do it? J. Musculoskelet. Neuronal Interact. 5, 213–224 (2005)
N.J. Crabtree, K. Kent, in Bone Health Assessment in Pediatrics, ed. by E. Fung, L. Bachrach, A. Sawyer (Springer, Cham, 2016), pp. 89–114
G.M. Blake et al. Comparison of effective dose to children and adults from dual X-ray absorptiometry examinations. Bone 38, 935–942 (2006)
J. Damilakis et al. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur. Radiol. 20, 2707–2714 (2010)
H.M. Allard et al. Vertebral bone density measurements by DXA are influenced by hepatic iron overload in patients with hemoglobinopathies. J. Clin. Densitom. (2018). https://doi.org/10.1016/j.jocd.2018.07.001
C. Rodd et al. Incident vertebral fractures 12 months following glucocorticoid initiation in children with rheumatic disorders. Pediatr. Rheumatol. (2012)
L. Ruggiero, V. De Sanctis, Multicentre study on prevalence of fractures in transfusion-dependent thalassaemic patients. J. Pediatr. Endocrinol. Metab. 11(Suppl 3), 773–778 (1998)
P.D. Delmas et al. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J. Bone Miner. Res. (2005). https://doi.org/10.1359/JBMR.041214
N. Kim et al. Underreporting of vertebral fractures on routine chest. Radiogr. Am. J. Roentgenol. 182, 297–300 (2004)
H.K. Genant et al. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 8, 1137–1148 (2009)
D.M. Black et al. A new approach to defining normal vertebral dimensions. J. Bone Miner. Res. 6, 883–892 (2009)
M. Grigoryan et al. Recognizing and reporting osteoporotic vertebral fractures. Eur. Spine J. 12, S104–S112 (2003)
W. Yu et al. Spinal bone mineral assessment in postmenopausal women: a comparison between dual X-ray absorptiometry and quantitative computed tomography. Osteoporos. Int. 5, 433–439 (1995)
P. Engkakul et al. Unrecognized vertebral fractures in adolescents and young adults with thalassemia syndromes. J. Pediatr. Hematol. Oncol. 35, 212–217 (2013)
A. Guermazi et al. Identification of vertebral fractures in osteoporosis. Semin. Musculoskelet. Radiol. 06, 241–252 (2002)
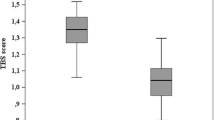
F.M. Ulivieri et al. Utility of the trabecular bone score (TBS) in secondary osteoporosis. Endocrine 47, 435–448 (2014)
O. Johnell et al. Predictive value of BMD for hip and other fractures. J. Bone Miner. Res. 20, 1185–1194 (2005)
M. Mylona et al. Comparison of DXA, QCT and trabecular structure in beta-thalassaemia. Eur. J. Haematol. 74, 430–437 (2005)
B.C. Silva et al. Trabecular bone score: a noninvasive analytical method based upon the DXA image. J. Bone Miner. Res. 29, 518–530 (2014)
B.C. Silva et al. Fracture risk prediction by non-BMD DXA measures: The 2015 ISCD Official Positions. Part 2: Trabecular bone score. J. Clin. Densitom. (2015). https://doi.org/10.1016/j.jocd.2015.06.008
M. Baldini et al. Spine bone texture assessed by trabecular bone score (TBS) to evaluate bone health in thalassemia major. Calcif. Tissue Int. 95, 540–546 (2014)
L. Pothuaud et al. Evaluation of the potential use of trabecular bone score to complement bone mineral density in the diagnosis of osteoporosis: a preliminary spine BMD–matched, case-control study. J. Clin. Densitom. 12, 170–176 (2009)
L. Pothuaud et al. Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone 42, 775–787 (2008)
J.M. Burnham et al. Bone density, structure, and strength in juvenile idiopathic arthritis: Importance of disease severity and muscle deficits. Arthritis Rheum. 58, 2518–2527 (2008)
J. Kalef-Ezra et al. Body composition in homozygous β-thalassemia. Ann. NY Acad. Sci. 904, 621–624 (2006)
S. Akpek et al. Evaluation of osteoporosis in thalassemia by quantitative computed tomography: is it reliable? Pediatr. Hematol. Oncol. 18, 111–116 (2001)
L. Danesi et al. Evaluation of spine and hip bone density by DXA and QCT in thalassemic patients. J. Pediatr. Endocrinol. Metab. 11(Suppl 3), 961–962 (1998)
T.L. Levin et al. MRI marrow observations in thalassemia: the effects of the primary disease, transfusional therapy, and chelation. Pediatr. Radiol. (1995). https://doi.org/10.1007/BF02011827
M. Tunacı et al. Imaging features of thalassemia. Eur. Radiol. 9, 1804–1809 (1999)
Jensen et al. High prevalence of low bone mass in thalassaemia major. Br. J. Haematol. 103, 911–915 (1998)
E.P. Vichinsky, The morbidity of bone disease in thalassemia. Ann. NY Acad. Sci. 850, 344–348 (1998)
B. Wonke, et al. Genetic and acquired predisposing factors and treatment of osteoporosis in thalassaemia major. J. Pediatr. Endocrinol. Metab. 11, 795–801 (1998)
U. Dundar, et al. Bone metabolism and mineral density in patients with beta-thalassemia major. Saudi Med. J. 28, 1425–1429 (2007)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants whose radiological images were included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pellegrino, F., Zatelli, M.C., Bondanelli, M. et al. Dual-energy X-ray absorptiometry pitfalls in Thalassemia Major. Endocrine 65, 469–482 (2019). https://doi.org/10.1007/s12020-019-02003-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02003-x