Abstract
Purpose
Selenoprotein P (SELENOP) has been previously related to various metabolic traits with partially conflicting results. The identification of SELENOP-associated metabolites, using an untargeted metabolomics approach, may provide novel biological insights relevant to disentangle the role of SELENOP in human health.
Methods
In this cross-sectional study, 572 serum metabolites were identified by comparing the obtained LC–MS/MS spectra with spectra stored in Metabolon’s spectra library. Serum SELENOP levels were measured in 832 men and women using an ELISA kit.
Results
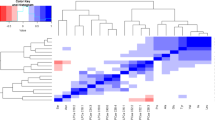
Circulating SELENOP levels were associated with 24 out of 572 metabolites after accounting for the number of independent dimensions in the metabolomics data, including inverse associations with alanine, glutamate, leucine, isoleucine and valine, an unknown compound X-12063, urate and the peptides gamma-glutamyl-leucine, and N-acetylcarnosine. Positive associations were observed between SELENOP and several lipid compounds. Of the identified metabolites, each standard deviation increase in the branched-chain amino acids (isoleucine, leucine, valine), alanine and gamma-glutamyl-leucine was related to higher odds of having T2DM [OR (95% CI): 1.96 (1.41–2.73); 1.62 (1.15–2.28); 1.94 (1.45–2.60), 1.57 (1.17–2.11), and 1.52 (1.13–2.05), respectively].
Conclusions
Higher serum SELENOP levels were associated with an overall healthy metabolomics profile, which may provide further insights into potential mechanisms of SELENOP-associated metabolic disorders.

Similar content being viewed by others
References
R.F. Burk, K.E. Hill, Selenoprotein P: an extracellular protein with unique physical characteristics and a role in selenium homeostasis. Annu. Rev. Nutr. 25, 215–235 (2005). https://doi.org/10.1146/annurev.nutr.24.012003.132120
H. Misu, T. Takamura, H. Takayama, H. Hayashi, N. Matsuzawa-Nagata, S. Kurita, K. Ishikura, H. Ando, Y. Takeshita, T. Ota, M. Sakurai, T. Yamashita, E. Mizukoshi, M. Honda, K. Miyamoto, T. Kubota, N. Kubota, T. Kadowaki, H.J. Kim, I.K. Lee, Y. Minokoshi, Y. Saito, K. Takahashi, Y. Yamada, N. Takakura, S. Kaneko, A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell. Metab. 12(5), 483–495 (2010). https://doi.org/10.1016/j.cmet.2010.09.015
S.J. Yang, S.Y. Hwang, H.Y. Choi, H.J. Yoo, J.A. Seo, S.G. Kim, N.H. Kim, S.H. Baik, D.S. Choi, K.M. Choi, Serum selenoprotein P levels in patients with type 2 diabetes and prediabetes: implications for insulin resistance, inflammation, and atherosclerosis. J. Clin. Endocrinol. Metab. 96(8), E1325–E1329 (2011). https://doi.org/10.1210/jc.2011-0620
H. Misu, K. Ishikura, S. Kurita, Y. Takeshita, T. Ota, Y. Saito, K. Takahashi, S. Kaneko, T. Takamura, Inverse correlation between serum levels of selenoprotein P and adiponectin in patients with type 2 diabetes. PLoS ONE. 7(4), e34952 (2012). https://doi.org/10.1371/journal.pone.0034952
R. di Giuseppe, M. Koch, S. Schlesinger, J. Borggrefe, M. Both, H.P. Muller, J. Kassubek, G. Jacobs, U. Nothlings, W. Lieb, Circulating selenoprotein P levels in relation to MRI-derived body fat volumes, liver fat content, and metabolic disorders. Obesity. 25(6), 1128–1135 (2017). https://doi.org/10.1002/oby.21841
M. Gharipour, M. Sadeghi, M. Salehi, M. Behmanesh, E. Khosravi, M. Dianatkhah, S. Haghjoo Javanmard, R. Razavi, A. Gharipour, Association of expression of selenoprotein P in mRNA and protein levels with metabolic syndrome in subjects with cardiovascular disease: Results of the Selenegene study. J. Gene Med. 19(3) (2017). https://doi.org/10.1002/jgm.2945
B.J. Ko, S.M. Kim, K.H. Park, H.S. Park, C.S. Mantzoros, Levels of circulating selenoprotein P, fibroblast growth factor (FGF) 21 and FGF23 in relation to the metabolic syndrome in young children. Int. J. Obes. 38(12), 1497–1502 (2014). https://doi.org/10.1038/ijo.2014.45
H.Y. Choi, S.Y. Hwang, C.H. Lee, H.C. Hong, S.J. Yang, H.J. Yoo, J.A. Seo, S.G. Kim, N.H. Kim, S.H. Baik, D.S. Choi, K.M. Choi, Increased selenoprotein p levels in subjects with visceral obesity and nonalcoholic fatty liver disease. Diabetes Metab. J. 37(1), 63–71 (2013). https://doi.org/10.4093/dmj.2013.37.1.63
A.N. Ogawa-Wong, M.J. Berry, L.A. Seale, Selenium and metabolic disorders: an emphasis on type 2 diabetes risk. Nutrients 8(2), 80 (2016). https://doi.org/10.3390/nu8020080
J. Mao, W. Teng, The relationship between selenoprotein P and glucose metabolism in experimental studies. Nutrients 5(6), 1937–1948 (2013). https://doi.org/10.3390/nu5061937
K. Hesse-Bahr, I. Dreher, J. Kohrle, The influence of the cytokines Il-1beta and INFgamma on the expression of selenoproteins in the human hepatocarcinoma cell line HepG2. Biofactors 11(1-2), 83–85 (2000)
H. Traulsen, H. Steinbrenner, D.P. Buchczyk, L.O. Klotz, H. Sies, Selenoprotein P protects low-density lipoprotein against oxidation. Free Radic. Res. 38(2), 123–128 (2004)
H. Steinbrenner, E. Bilgic, L. Alili, H. Sies, P. Brenneisen, Selenoprotein P protects endothelial cells from oxidative damage by stimulation of glutathione peroxidase expression and activity. Free. Radic. Res. 40(9), 936–943 (2006). https://doi.org/10.1080/10715760600806248
C.D. Davis, P.A. Tsuji, J.A. Milner, Selenoproteins and cancer prevention. Annu. Rev. Nutr. 32, 73–95 (2012). https://doi.org/10.1146/annurev-nutr-071811-150740
Y. Saito, N. Sato, M. Hirashima, G. Takebe, S. Nagasawa, K. Takahashi, Domain structure of bi-functional selenoprotein P. Biochem. J. 381(Pt 3), 841–846 (2004). https://doi.org/10.1042/BJ20040328
U. Nothlings, M. Krawczak, PopGen. A population-based biobank with prospective follow-up of a control group. Bundesgesundheitsblatt. Gesundh. Gesundh. 55(6-7), 831–835 (2012). https://doi.org/10.1007/s00103-012-1487-2
M. Koch, J. Borggrefe, J. Barbaresko, G. Groth, G. Jacobs, S. Siegert, W. Lieb, M.J. Muller, A. Bosy-Westphal, M. Heller, U. Nothlings, Dietary patterns associated with magnetic resonance imaging-determined liver fat content in a general population study. Am. J. Clin. Nutr. 99(2), 369–377 (2014). https://doi.org/10.3945/ajcn.113.070219
M. Koch, S. Freitag-Wolf, S. Schlesinger, J. Borggrefe, J.R. Hov, M.K. Jensen, J. Pick, M.R.P. Markus, T. Hopfner, G. Jacobs, S. Siegert, A. Artati, G. Kastenmuller, W. Romisch-Margl, J. Adamski, T. Illig, M. Nothnagel, T.H. Karlsen, S. Schreiber, A. Franke, M. Krawczak, U. Nothlings, W. Lieb, Serum metabolomic profiling highlights pathways associated with liver fat content in a general population sample. Eur. J. Clin. Nutr. 71(8), 995–1001 (2017). https://doi.org/10.1038/ejcn.2017.43
C.D. Dehaven, A.M. Evans, H. Dai, K.A. Lawton, Organization of GC/MS and LC/MS metabolomics data into chemical libraries. J. Chemin-. 2(1), 9 (2010). https://doi.org/10.1186/1758-2946-2-9
K. Fischer, D. Moewes, M. Koch, H.P. Muller, G. Jacobs, J. Kassubek, W. Lieb, U. Nothlings, MRI-determined total volumes of visceral and subcutaneous abdominal and trunk adipose tissue are differentially and sex-dependently associated with patterns of estimated usual nutrient intake in a northern German population. Am. J. Clin. Nutr. 101(4), 794–807 (2015). https://doi.org/10.3945/ajcn.114.101626
J. Barbaresko, S. Siegert, M. Koch, I. Aits, W. Lieb, S. Nikolaus, M. Laudes, G. Jacobs, U. Nothlings, Comparison of two exploratory dietary patterns in association with the metabolic syndrome in a Northern German population. Br. J. Nutr. 112(8), 1364–1372 (2014). https://doi.org/10.1017/S0007114514002098
B.E. Ainsworth, W.L. Haskell, S.D. Herrmann, N. Meckes, D.R. Bassett Jr., C. Tudor-Locke, J.L. Greer, J. Vezina, M.C. Whitt-Glover, A.S. Leon, 2011 Compendium of physical activities: a second update of codes and MET values. Med. Sci. Sports Exerc. 43(8), 1575–1581 (2011). https://doi.org/10.1249/MSS.0b013e31821ece12
K.G. Alberti, R.H. Eckel, S.M. Grundy, P.Z. Zimmet, J.I. Cleeman, K.A. Donato, J.C. Fruchart, W.P. James, C.M. Loria, S.C. Smith Jr., International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity, Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16), 1640–1645 (2009). https://doi.org/10.1161/CIRCULATIONAHA.109.192644
R. Wehrens, J.A. Hageman, F. van Eeuwijk, R. Kooke, P.J. Flood, E. Wijnker, J.J. Keurentjes, A. Lommen, H.D. van Eekelen, R.D. Hall, R. Mumm, R.C. de Vos, Improved batch correction in untargeted MS-based metabolomics. Metabolomics 12, 88 2016). https://doi.org/10.1007/s11306-016-1015-8
S.M. Nelson, O.A. Panagiotou, G.M. Anic, A.M. Mondul, S. Mannisto, S.J. Weinstein, D. Albanes, Metabolomics analysis of serum 25-hydroxy-vitamin D in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) Study. Int. J. Epidemiol. 45(5), 1458–1468 (2016). https://doi.org/10.1093/ije/dyw148
C.B. Newgard, J. An, J.R. Bain, M.J. Muehlbauer, R.D. Stevens, L.F. Lien, A.M. Haqq, S.H. Shah, M. Arlotto, C.A. Slentz, J. Rochon, D. Gallup, O. Ilkayeva, B.R. Wenner, W.S. Yancy Jr., H. Eisenson, G. Musante, R.S. Surwit, D.S. Millington, M.D. Butler, L.P. Svetkey, A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell. Metab. 9(4), 311–326 (2009). 10.1016/j.cmet.2009.02.002
O. Zhenyukh, E. Civantos, M. Ruiz-Ortega, M.S. Sanchez, C. Vazquez, C. Peiro, J. Egido, S. Mas, High concentration of branched-chain amino acids promotes oxidative stress, inflammation and migration of human peripheral blood mononuclear cells via mTORC1 activation. Free Radic. Biol. Med. 104, 165–177 (2017). https://doi.org/10.1016/j.freeradbiomed.2017.01.009
C.J. Lynch, S.H. Adams, Branched-chain amino acids in metabolic signalling and insulin resistance. Nat. Rev. Endocrinol. 10(12), 723–736 (2014). https://doi.org/10.1038/nrendo.2014.171
S. Cheng, E.P. Rhee, M.G. Larson, G.D. Lewis, E.L. McCabe, D. Shen, M.J. Palma, L.D. Roberts, A. Dejam, A.L. Souza, A.A. Deik, M. Magnusson, C.S. Fox, C.J. O’Donnell, R.S. Vasan, O. Melander, C.B. Clish, R.E. Gerszten, T.J. Wang, Metabolite profiling identifies pathways associated with metabolic risk in humans. Circulation 125(18), 2222–2231 (2012). https://doi.org/10.1161/CIRCULATIONAHA.111.067827
M.A. Reeves, P.R. Hoffmann, The human selenoproteome: recent insights into functions and regulation. Cell. Mol. Life Sci. 66(15), 2457–2478 (2009). https://doi.org/10.1007/s00018-009-0032-4
K. Renko, P.J. Hofmann, M. Stoedter, B. Hollenbach, T. Behrends, J. Kohrle, U. Schweizer, L. Schomburg, Down-regulation of the hepatic selenoprotein biosynthesis machinery impairs selenium metabolism during the acute phase response in mice. FASEB J. 23(6), 1758–1765 (2009). https://doi.org/10.1096/fj.08-119370
W.E. Gall, K. Beebe, K.A. Lawton, K.P. Adam, M.W. Mitchell, P.J. Nakhle, J.A. Ryals, M.V. Milburn, M. Nannipieri, S. Camastra, A. Natali, E. Ferrannini, alpha-hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS. One. 5(5), e10883 (2010). https://doi.org/10.1371/journal.pone.0010883
J. Cobb, A. Eckhart, A. Motsinger-Reif, B. Carr, L. Groop, E. Ferrannini, alpha-Hydroxybutyric acid is a selective metabolite biomarker of impaired glucose tolerance. Diabetes Care 39(6), 988–995 (2016). https://doi.org/10.2337/dc15-2752
G. Peddinti, J. Cobb, L. Yengo, P. Froguel, J. Kravic, B. Balkau, T. Tuomi, T. Aittokallio, L. Groop, Early metabolic markers identify potential targets for the prevention of type 2 diabetes. Diabetologia 60(9), 1740–1750 (2017). https://doi.org/10.1007/s00125-017-4325-0
W. Koenig, C. Meisinger, Uric acid, type 2 diabetes, and cardiovascular diseases: fueling the common soil hypothesis? Clin. Chem. 54(2), 231–233 (2008). https://doi.org/10.1373/clinchem.2007.099705
A.M. Evans, C.D. DeHaven, T. Barrett, M. Mitchell, E. Milgram, Integrated, nontargeted ultrahigh performance liquid chromatography/electrospray ionization tandem mass spectrometry platform for the identification and relative quantification of the small-molecule complement of biological systems. Anal. Chem. 81(16), 6656–6667 (2009). https://doi.org/10.1021/ac901536h
S.C. Kalhan, L. Guo, J. Edmison, S. Dasarathy, A.J. McCullough, R.W. Hanson, M. Milburn, Plasma metabolomic profile in nonalcoholic fatty liver disease. Metabolism 60(3), 404–413 (2011). https://doi.org/10.1016/j.metabol.2010.03.006
Y. Zhang, X. Chen, Reducing selenoprotein P expression suppresses adipocyte differentiation as a result of increased preadipocyte inflammation. Am. J. Physiol. Endocrinol. Metab. 300(1), E77–E85 (2011). https://doi.org/10.1152/ajpendo.00380.2010
G. Mingrone, L. Castagneto-Gissey, K. Mace, Use of dicarboxylic acids in type 2 diabetes. Br. J. Clin. Pharmacol. 75(3), 671–676 (2013). https://doi.org/10.1111/j.1365-2125.2012.04177.x
M.L. Garg, R.J. Blake, R.B. Wills, Macadamia nut consumption lowers plasma total and LDL cholesterol levels in hypercholesterolemic men. J. Nutr. 133(4), 1060–1063 (2003)
K. Nagao, T. Yanagita, Medium-chain fatty acids: functional lipids for the prevention and treatment of the metabolic syndrome. Pharmacol. Res. 61(3), 208–212 (2010). https://doi.org/10.1016/j.phrs.2009.11.007
R.N. Lemaitre, A.M. Fretts, C.M. Sitlani, M.L. Biggs, K. Mukamal, I.B. King, X. Song, L. Djousse, D.S. Siscovick, B. McKnight, N. Sotoodehnia, J.R. Kizer, D. Mozaffarian, Plasma phospholipid very-long-chain saturated fatty acids and incident diabetes in older adults: the Cardiovascular Health Study. Am. J. Clin. Nutr. 101(5), 1047–1054 (2015). https://doi.org/10.3945/ajcn.114.101857
R. di Giuseppe, S. Plachta-Danielzik, M. Koch, U. Nothlings, S. Schlesinger, J. Borggrefe, M. Both, H.P. Muller, J. Kassubek, G. Jacobs, W. Lieb, Dietary pattern associated with selenoprotein P and MRI-derived body fat volumes, liver signal intensity, and metabolic disorders. Eur. J. Nutr. (2018). https://doi.org/10.1007/s00394-018-1624-2
A.E. Altinova, O.T. Iyidir, C. Ozkan, D. Ors, M. Ozturk, O. Gulbahar, N. Bozkurt, F.B. Toruner, M. Akturk, N. Cakir, M. Arslan, Selenoprotein P is not elevated in gestational diabetes mellitus. Gynecol. Endocrinol. 31(11), 874–876 (2015). https://doi.org/10.3109/09513590.2015.1103220
E. Ferrannini, A. Natali, S. Camastra, M. Nannipieri, A. Mari, K.P. Adam, M.V. Milburn, G. Kastenmuller, J. Adamski, T. Tuomi, V. Lyssenko, L. Groop, W.E. Gall, Early metabolic markers of the development of dysglycemia and type 2 diabetes and their physiological significance. Diabetes 62(5), 1730–1737 (2013). https://doi.org/10.2337/db12-0707
Y. Saito, T. Hayashi, A. Tanaka, Y. Watanabe, M. Suzuki, E. Saito, K. Takahashi, Selenoprotein P in human plasma as an extracellular phospholipid hydroperoxide glutathione peroxidase. Isolation and enzymatic characterization of human selenoprotein p. J. Biol. Chem. 274(5), 2866–2871 (1999)
R. Stoffaneller, N.L. Morse, A review of dietary selenium intake and selenium status in Europe and the Middle East. Nutrients 7(3), 1494–1537 (2015). nu7031494[pii]10.3390/nu7031494
Funding
The PopGen 2.0 network is supported by the German Federal Ministry of Education and Research [Grant Number 01EY1103]. R.d.G. is supported by the Deutsche Forschungsgemeinschaft Excellence Cluster “Inflammation at Interfaces” (Grant EXC306/2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study procedures have been approved by the Ethics Committee of the Medical Faculty of the University of Kiel, Germany.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
di Giuseppe, R., Koch, M., Nöthlings, U. et al. Metabolomics signature associated with circulating serum selenoprotein P levels. Endocrine 64, 486–495 (2019). https://doi.org/10.1007/s12020-018-1816-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1816-9