Abstract
Background
Large Achilles tendon defects pose a treatment challenge. The standard treatment with a turndown flap requires a large extensile incision, puts the sural nerve at risk, and demands slow, careful rehabilitation. Dual allograft semitendinosus reconstruction is a new clinical alternative that has the theoretical advantages of a smaller incision, less dissection, and a stronger construct that may allow for faster rehabilitation.
Questions/Purposes
In a cadaver biomechanical model, we compared the dual allograft semitendinosus reconstruction with the myofascial turndown in terms of (1) mechanical strength and resistance to deformation and (2) failure mechanisms in reconstruction of large segmental Achilles defects.
Methods
An 8-cm segmental Achilles defect was created in 18 cadaveric lower extremities, nine matched pairs without defect or previous surgery (mean age, 78.4 years; range, 60–97 years; three female and six male pairs). Femoral neck densitometry to determine bone mineral density found that all specimens except two were osteopenic or osteoporotic. Specimens in each pair were assigned to allograft or turndown reconstruction. The constructs were mounted on a load frame and differential variable reluctance transducers were applied to measure deformation. Specimens were preconditioned and then loaded axially. Tensile force and proximal and distal construct deformation were measured at clinical failure, defined as 10 mm of displacement, and at ultimate failure, defined as failure of the reconstruction. Failure mechanism was recorded.
Results
Tensile strength at time zero was higher in the allograft versus the turndown construct at clinical failure (156.9 ± 29.7 N versus 107.2 ± 20.0 N, respectively; mean difference, −49.7 N; 95% CI, −66.3 to −33.0 N; p < 0.001) and at ultimate failure (290.9 ± 83.2 N versus 140.7 ± 43.5 N, respectively; mean difference, −150.2 N; 95% CI, −202.9 to −97.6 N; p < 0.001). Distal construct deformation was lower in the turndown versus the allograft construct at clinical failure (1.6 ± 1.0 mm versus 4.7 ± 0.7 mm medially and 2.2 ± 1.0 mm versus 4.8 ± 1.1 mm laterally; p < 0.001). Semitendinosus allograft failure occurred via calcaneal bone bridge fracture in eight of nine specimens. All myofascial turndowns failed via suture pullout through the fascial tissue at its insertion.
Conclusion
In this comparative biomechanical study, dual semitendinosus allograft reconstruction showed greater tensile strength and construct deformation compared with myofascial turndown in a cadaveric model of large Achilles tendon defects.
Clinical Relevance
Further study of dual semitendinosus allograft for treatment of severe Achilles tendon defects with cyclic loading and investigation of clinical results will better elucidate the clinical utility and indications for this technique.
Similar content being viewed by others
Introduction
Large segmental Achilles tendon defects present a difficult problem to treating surgeons. Various procedures including fascial turndown [2], local autograft tendon transfer [11, 17], allograft reconstruction [14], and synthetic graft reconstruction [6, 15] have been used to reconstruct these defects with varying degrees of success. Fascial turndown has shown good results as a treatment for this condition [7, 16], but this procedure also involves an incision extending proximally in the calf with risk of damage to the sural nerve. The use of a semitendinosus autograft reconstruction has been described [4, 9, 10]. In one study, 22 of 26 patients undergoing this procedure returned to preinjury daily and sport activities at approximately 7 months after surgery [9]. However, autograft harvesting is limited because it yields only one graft. Additionally, it requires a second surgical site incision, can cause postoperative knee pain [1], and extends operative time.
Dual semitendinosus allograft for large-defect Achilles reconstruction [8] is a new technique that obviates a second surgical site and may better resist tensile forces. However, to our knowledge, the strength of this new technique has not been compared biomechanically with the fascial turndown procedure.
The purpose of this cadaveric study was to compare (1) mechanical strength and resistance to longitudinal deformation and (2) failure mechanisms between dual allograft semitendinosus Achilles reconstruction and with the myofascial turndown repair using a large segmental Achilles defect model in cadavers. We theorized that there would be no difference between the two constructs and that failure would occur primarily at the proximal junction in both constructs.
Methods
Nine paired full-length cadaveric lower extremities were used. The average age was 78.4 years (range, 60–97 years), with three female and six male pairs. Specimens were screened for musculoskeletal disease, defect, or previous surgery. Semitendinosus allografts were harvested from other cadaveric specimens in the study to keep specimen quality consistent. These allografts were frozen and thawed in normal saline 15 to 30 minutes before implantation during the procedure. The grafts were not pretensioned, packaged, sterilized, or irradiated. The specimens were kept hydrated by spraying frequently with 0.9% saline, and laboratory temperature was maintained at 24°C. Except for two limbs containing hip fracture hardware, bone quality was evaluated using femoral neck dual-energy x-ray absorptiometry scanning [18]. A GE Lunar Prodigy® DXA (GE Healthcare, Chicago, IL, USA) scanner was used to obtain the bone mineral density. The young-adult T-score was used to determine the level of osteopenia. Bone mineral density was osteopenic (−2.5 ≤ T-score ≤ −1.0) or osteoporotic (T-score ≤ −2.5) [3] on all but two specimens based on femoral neck densitometry (0.69 ± 0.25 g/cm2). Specimens in each pair were randomized to either myofascial turndown or semitendinosus allograft. One hip fracture specimen was in the turndown group and the other was in the allograft group. A posterior midline approach was used, and an 8-cm segmental defect was created by scalpel incision from the Achilles insertion and measured proximally.
Surgical Technique
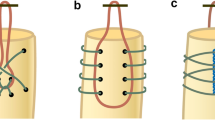
A single fellowship-trained orthopaedic surgeon (MCA) performed all procedures. After completely thawing in normal saline, both semitendinosus allografts were tubularized with a Number 2-0 braided suture and brought through the end of the proximal Achilles stump. Each allograft limb underwent three Pulvertaft weaves and was anchored with a Number 5 braided polyester suture at each allograft-Achilles stump weave junction. The two limbs were sutured to one another with the same suture and excess graft was trimmed and contoured. Distally, a central dorsal bone tunnel 8 mm wide was created in the calcaneus with a 4-mm burr. Medial and lateral walls of the calcaneus were exposed, and two exit tunnels at 90° angles to the central tunnel were fashioned with the same burr. A suture passer was used to shuttle each limb through the central tunnel and out the medial and lateral tunnels, respectively. The graft was tensioned in standard clinical fashion and then sutured to itself with Number 5 braided polyester suture (Fig. 1).
The myofascial turndown flap was first measured and drawn proximally on the myofascial junction. A 10-cm flap one-third the width of the proximal Achilles myofascial origin was used, leaving a 2-cm overlap and enough length to cover the defect. This was cut and freed with a Number 10 blade. The turndown junction was secured with Number 5 braided polyester suture in a figure-of-eight fashion. The remaining defect was closed with a running whipstitch of the same suture. Distally, the myofascial tissue was secured with three equally spaced modified Kessler stitches with Number 5 braided polyester suture brought through bone tunnels from 0.062-inch K-wire holes in the calcaneus (Fig. 2). We chose this repair technique based on the study by McCoy and Haddad [12] that showed no difference between the Krackow, Bunnell, or Kessler suture techniques for Achilles repair.
Biomechanical Testing
The foot was disarticulated through the subtalar joint and the Achilles was dissected free of excess soft tissues, preserving the gastrocnemius soleus complex proximally. The calcaneus was mounted with two centrally threaded 5-mm Steinmann pins and secured in a servohydraulic load frame (MTS Systems Corp, Eden Prairie, MN, USA). The proximal myotendinous tissue was anchored proximally through a custom-designed and fabricated soft tissue cryogenic grip, which was packed with dry ice to prevent slippage. Four differential variable reluctance transducers (DVRTs; LORD Microstrain, Williston, VT, USA), resolution 4.5 µm, were applied to the reconstruction to measure displacement proximally and distally and medially and laterally, two at the proximal and two at the distal junctions (Figs. 1 and 2). The DVRTs were placed within 3 mm of the medial and lateral edges of the myofascia in the turndown samples and in the center of each of the legs of the semitendinosus grafts. The DVRTs were attached to soft tissue via small barbed pins. For placement in bone, a 0.5-mm pilot hole was drilled to facilitate insertion.
A monotonic loading model was used to model mechanical forces in a patient who bears full weight after a large reconstruction. Cyclic loading was not used because the reconstruction techniques tested in our study generally are not used in treating acute rupture. At our institution they are salvage procedures used to reconstruct large defects that arise after many chronic ruptures. A 15-N load was applied for 30 seconds across the construct to precondition specimens. After preconditioning, the specimens were loaded at rate of 1 mm per second to failure. Tensile forces representing time zero clinical forces were recorded at clinical failure (defined as 10 mm of load frame actuator displacement) and at ultimate failure (failure of the construct). Mullaney et al. [13] reported statistically significant weakness after Achilles repair when the affected side was measured against the contralateral side at 10° of plantar flexion. Ten patients had a clinically significant strength deficit greater than 20% at 10° of plantar flexion, and 15 patients had a clinically significant strength deficit at 20° of plantar flexion. A basic trigonometric analysis showed that 8 to 10 mm of Achilles tendon excursion is required for 10° of ankle motion, depending on the size of the foot and associated soft structures. This assumes a 50-mm moment arm about which the Achilles acts (50 mm SIN(10) = 9 mm); therefore we chose 10 mm of displacement to represent clinical failure.
Construct deformation was measured via DVRT at clinical and ultimate failure. After testing, specimens were removed from the frame and the mechanism of failure was documented.
Statistical Analysis
Power analysis using pilot data from our laboratory found that nine specimens per group would provide 90% power to detect a difference of 51 N in tensile force at 10 mm displacement at the p = 0.05 significance level. This difference was considered to be clinically relevant. The four specimen pairs used for the power analysis were all male with mean age 77.25 years (range, 67-97 years). A paired t-test with alpha level 0.05 was used to compare tensile strength, distal construct deformation, and bone mineral density between allograft and turndown groups (SPSS, Version 22.0, IBM SPSS Statistics, Armonk, NY, USA).
Results
The tensile strength at time zero was higher in the allograft versus the turndown construct at clinical (156.9 ± 29.7 N versus 107.2 ± 20.0 N, respectively; difference of means, −49.7 N; 95% CI, −66.3 to −33.0 N; p < 0.001) and ultimate failure (290.9 ± 83.3 N versus 140.7 ± 43.5 N; 95% CI, −202.9 to −97.6 N; p < 0.001) (Table 1). Distal construct deformation was lower in the allograft construct versus the turndown construct at clinical failure medially (1.6 ± 1.0 mm versus 4.7 ± 0.7 mm; p < 0.001) and laterally (2.2 ± 1.0 mm versus 4.8 ± 1.1 mm; p < 0.001) (Table 2; Fig. 3). No difference in proximal construct deformation was found.
Semitendinosus allograft failure occurred via calcaneal bone bridge fracture in eight of nine specimens (Fig. 4), and all myofascial turndowns failed through suture pullout through the fascial tissue at its insertion (Fig. 5). One semitendinosus allograft failure occurred via one of the two semitendinosus grafts as it entered the bone tunnel in the calcaneus (Fig. 6). No failures occurred at the grip sites through the triceps surae complex, the proximal myotendinous junction, or via de novo tendon substance rupture.
Discussion
Large Achilles tendon defects pose a treatment challenge. The standard treatment with a turndown flap needs a large extensile incision, poses a risk to the sural nerve, and requires slow, careful rehabilitation. In addition, some parts of the turndown flap may include damaged tendon tissue. Dual allograft semitendinosus reconstruction is a new clinical alternative that has the theoretical advantages of smaller incision, less dissection, and a stronger construct that may allow for faster rehabilitation. The strength of these two constructs has not been compared biomechanically, to our knowledge. We compared tensile strength and deformation in the constructs to determine whether the allograft construct differs from the standard turndown procedure in these outcome measures. We found greater strength and greater resistance to distal deformation in the allograft construct compared with the turndown construct.
The limitations of this study are those inherent to human cadaveric experiments and in vitro experiments. Some specimens were from elderly individuals. However, we do not believe bone quality limited us from detecting a difference between the two reconstruction modes because we used matched specimen pairs. In fact, a cohort of specimens with normal bone density may have shown a larger difference between the turndown and semitendinosus constructs because there would be less potential for early fracture through the bone tunnels. The allografts in our study did not undergo sterilization processing or irradiation. However, we did expose the grafts to the same freezing process used to store allografts in the United States. Irradiation and processing has been shown to have little effect on biomechanical properties of allograft tissues used for ACL reconstruction, with no difference reported between structural properties in a particular threshold of irradiation [5]. We attempted to limit variables by mounting the construct securely in the frame and maintaining fixation throughout testing for each specimen. There were no failures through the grip or anchor sites. Grafts and the turndown were tensioned tight in standard clinical fashion by a single investigator (MCA). However, tension was not measured and we are not aware of any reference standard for tension in these procedures. There may have been variability among specimens, but clinical standards were used.
The tensile forces in this study were measured at time zero and do not reflect the extensive bone remodeling and repair that would occur clinically with healing with time. Patients undergoing this salvage procedure would be well immobilized and nonweightbearing for an extended postoperative period, during which healing would occur. Extensive bone remodeling and repair would likely increase the strength of the bone where the allograft failed in this study. Collagen remodeling during a longer period could increase the strength of the turndown construct. These properties contribute substantially to the strength of the final construct. Therefore, our study provides a glimpse only of comparative strength of the constructs at the time of surgery. However, the difference at time zero along with other theoretical advantages of the allograft procedure represents a potential overall benefit of the procedure.
In this study, semitendinosus allograft Achilles tendon reconstruction showed higher strength and lower deformation at time zero compared with myofascial turndown at clinical and ultimate failure. The difference in failure load that we observed between the groups may reflect the larger cross-sectional area at the distal insertion of the allograft compared with that of the myofascial flap turndown. The findings suggest that this allograft construct might have potential for use in augmentation of Achilles reconstruction with large segmental Achilles defects that result from chronic or missed ruptures, severe tendinopathy, or tendon loss from prior infection. Defects greater than 5 cm typically call for a reconstructive procedure requiring graft augmentation [11, 17]. The potential advantages of using allograft over other materials for reconstruction include variety of graft options, avoidance of donor morbidity, ability to select appropriate graft size and length, and potential for use of a second graft for added support. The potential disadvantages of allograft compared with a turndown are cost and uncertainty regarding final integration in the healed Achilles tendon construct. However, the turndown requires more operative time than the allograft procedure, and therefore an overall cost comparison would be needed to compare the cost of the two procedures. The findings at time zero appear to favor the allograft technique, but clinical studies are needed to confirm these advantages while taking healing into account.
In our study, the most-common mode of failure for the semitendinosus reconstruction was fracture through the bone tunnel. This finding is not surprising given that most specimens were osteopenic or osteoporotic. However, these results suggest it may be advisable to burr the smallest exit tunnel possible to accommodate the graft thickness and avoid an aggressive calcaneal exostosis resection to achieve the largest bone bridge possible. One semitendinosus construct failed through a single graft limb where it entered the bone tunnel, leaving the other graft intact and functional. This observation suggests that the redundancy of dual graft reconstruction may offer clinical benefit because failure of a single graft may not cause clinical failure of the reconstruction as a whole. Failure of the myofascial turndown occurred through pullout of the sutures through the distal end of the myofascial graft in all specimens. Typically failure of this construct occurs at the proximal turndown junction [11]. However, each specimen received three equally spaced modified Kessler sutures in the fascial turndown tissue and we did not observe abnormalities in failure mechanism in the matching specimens. Turndown reconstruction has generally good clinical results [7, 16] but requires slow, careful rehabilitation to avoid reinjury.
In this in vitro biomechanical study, dual semitendinosus allograft reconstruction showed increased tensile strength and decreased construct deformation compared with myofascial turndown in a cadaveric model of large Achilles tendon defects. Further studies with cyclic loading and investigation of clinical results will better elucidate the clinical utility and indications for this new surgical technique.
References
Ardern CL, Webster KE. Knee flexor strength recovery following hamstring tendon harvest for anterior cruciate ligament reconstruction: a systematic review. Orthop Rev (Pavia). 2009;1:e12.
Bosworth DM. Repair of defects in the tendo achillis. J Bone Joint Surg Am. 1956;38:111–114.
Carey JJ, Delaney MF. T-scores and Z-scores. Clinic Rev Bone Miner Metab. 2010;8:113–121.
Dumbre Patil SS, Dumbre Patil VS, Basa VR, Dombale AB. Semitendinosus tendon autograft for reconstruction of large defects in chronic Achilles tendon ruptures. Foot Ankle Int. 2014;35:699–705.
Fideler BM, Vangsness CT Jr, Lu B, Orlando C, Moore T. Gamma irradiation: effects on biomechanical properties of human bone-patellar tendon-bone allografts. Am J Sports Med. 1995;23:643–646.
Giza E, Frizzell L, Farac R, Williams J, Kim S. Augmented tendon Achilles repair using a tissue reinforcement scaffold: a biomechanical study. Foot Ankle Int. 2011;32:S545–S549.
Guclu B, Basat HC, Yildirim T, Bozduman O, Us AK. Long-term results of chronic Achilles tendon ruptures repaired With V-Y tendon plasty and fascia turndown. Foot Ankle Int. 2016;37:737–742.
Hsu NN, Tan EW, Miller SD. Dual semitendinous allograft reconstruction of large Achilles tendon defects. Tech Foot Ankle Surg. 2016;15:202–209.
Maffulli N, Del Buono A, Spiezia F, Maffulli GD, Longo UG, Denaro V. Less-invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achilles tendon. Am J Sports Med. 2013;41:865–871.
Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008;9:100.
Mann RA, Holmes GB Jr, Seale KS, Collins DN. Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am. 1991;73:214–219.
McCoy BW, Haddad SL. The strength of achilles tendon repair: a comparison of three suture techniques in human cadaver tendons. Foot Ankle Int. 2010;31:701–705.
Mullaney MJ, McHugh MP, Tyler TF, Nicholas SJ, Lee SJ. Weakness in end-range plantar flexion after Achilles tendon repair. Am J Sports Med. 2006;34:1120–1125.
Nellas ZJ, Loder BG, Wertheimer SJ. Reconstruction of an Achilles tendon defect utilizing an Achilles tendon allograft. J Foot Ankle Surg. 1996;35:144-148; discussion 190.
Ozaki J, Fujiki J, Sugimoto K, Tamai S, Masuhara K. Reconstruction of neglected Achilles tendon rupture with Marlex mesh. Clin Orthop Relat Res. 1989;238:204–208.
Us AK, Bilgin SS, Aydin T, Mergen E. Repair of neglected Achilles tendon ruptures: procedures and functional results. Arch Orthop Trauma Surg. 1997;116:408–411.
Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle. 1993;14:443–449.
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1-129. Available at: http://apps.who.int/iris/bitstream/10665/39142/1/WHO_TRS_843_eng.pdf. Accessed June 1, 2017.
Acknowledgments
We thank Lyn Camire, MA, ELS, of our department for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
About this article
Cite this article
Aynardi, M.C., Atwater, L.C., Melvani, R. et al. Is Dual Semitendinosus Allograft Stronger Than Turndown for Achilles Tendon Reconstruction? An In Vitro Analysis. Clin Orthop Relat Res 475, 2588–2596 (2017). https://doi.org/10.1007/s11999-017-5410-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-017-5410-x