Abstract
Background
Multiple studies have reported favorable short-term outcomes using tantalum cones to reconstruct massive bone defects during revision TKA. However, longer-term followup is needed to determine the durability of these reconstructions.
Questions/purposes
We wished to determine the mid-term (1) reoperation rates for septic and aseptic causes, (2) radiologic findings of osseointegration, and (3) clinical outcomes based on the Knee Society score in patients who underwent revision knee arthroplasty with tantalum cones for severe bone loss.
Methods
We retrospectively evaluated records of 18 patients (18 knees) who underwent revision knee arthroplasty with use of tantalum cones between 2005 and 2008; the primary indications for use of this approach were to reconstruct massive bone defects classified as Anderson Orthopaedic Research Institute Types 2B and 3. During this period, all defects of this type were treated with this approach and no cones were used for more-minor defects. A total of 26 cones (13 tibial and 13 femoral) were implanted. There were 12 female and six male patients with a mean age of 73 years (range, 55–84 years) at the time of revision. The indication for the revision included aseptic loosening (five patients) and second-stage reimplantation for deep infection (13 patients). Patients were followed for a mean of 6 years (range, 5–8 years). No patient was lost to followup. Clinical and radiographic outcomes were assessed with the Knee Society clinical rating system and radiographic evaluation system.
Results
There have been two reoperations for recurrent infection; at surgery, the two cones showed osseointegration. No evidence of loosening or migration of any implant was noted on the most recent radiographs. Knee Society knee scores improved from a mean of 31 points before surgery to 77 points at latest followup (p < 0.001), and function scores improved from a mean of 22 points to 65 points (p < 0.001).
Conclusions
Tantalum cones for reconstruction of massive bone defects in revision knee arthroplasty provided secure fixation with excellent results at average followup of 6 years, although this series included relatively few patients. These devices are a viable option for surgeons to use in situations with severe bone loss. Further studies with longer followups are needed to confirm the durability of these reconstructions.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Introduction
Revision TKA often involves severe bone loss that presents the treating surgeon with a complex reconstructive challenge. Major tibial and femoral bone defects, classified as Anderson Orthopaedic Research Institute (AORI) [10] Types 2B and 3, have been reconstructed using impaction bone grafting with or without mesh augmentation [22, 25, 38, 40, 44], structural or bulk allografts [7, 11, 14, 16, 17, 28, 31, 39], modular metal augmentations of prostheses [15, 32], and tumor-type megaprostheses [2]. Studies using structural allografts have reported numerous complications and minimum 5-year survivorship of 67% to 96% [1, 6, 7, 14, 17], whereas reconstructions with tumor-type megaprostheses have shown a 5-year survivorship of 68% [33]. Although there have been studies reporting encouraging mid-term results with these treatment options [6, 43], the best method has not been established [10].
Cone-shaped porous tantalum augments have been proposed as an alternative method to reconstruct severe bone defects during revision knee arthroplasty [9, 18, 21, 23, 24, 26, 34–36, 42]. Porous tantalum is widely used in total hip reconstruction [4], especially for treatment of severe acetabular bone loss during revision hip arthroplasty [4, 5, 30, 37, 41]. High volumetric porosity (average 80%), fully interconnected pores, and a low modulus of elasticity (3 GPa) similar to cancellous bone all enhance the potential for bone ingrowth and allow for a more physiologic load transfer with diminished stress shielding [3, 8]. Multiple studies have shown that tantalum cones provide stable fixation in the treatment of severe bone deficiencies in total knee revision during the short-term with documented osseointegration [9, 18, 21, 23, 24, 26, 34–36, 42], however, longer-term followup is needed to determine the durability of these reconstructions.
The purposes of this study were to determine the mid-term (1) reoperation rates for septic and aseptic causes, (2) radiologic findings of osseointegration, and (3) clinical outcomes based on Knee Society scores in patients who underwent revision knee arthroplasty with tantalum cones for significant bone loss.
Patients and Methods
After obtaining formal institutional review board approval, we retrospectively evaluated the records of 18 patients who underwent revision TKA using porous tantalum cones (Trabecular MetalTM; Zimmer, Warsaw, IN, USA) at one institution from November 2005 to August 2008. We included all patients treated with revision knee arthroplasty in which tantalum cones were used for reconstruction of severe tibial and/or femoral bone defects. During the study period, our indications for use of this approach were the need to reconstruct massive bone defects classified as AORI [10] Types 2B and 3. All defects of this type were treated with this approach during the study, and no cones were used for more minor defects. All patients were followed clinically and radiographically for a mean of 6 years (range, 5–8 years) and no patients were lost to followup. The patient cohort included 12 women and six men with an average age of 73 years (range, 55–84 years) at the time of revision. Mean BMI was 29 kg/cm2 (range, 24–35 kg/cm2). There were six left and 12 right knees. The underlying diagnoses that led to the initial primary TKA were osteoarthritis in 14 knees and rheumatoid arthritis in four knees. Patients had a mean of 2.6 (range, 1–4) previous knee surgeries before the revision procedure that required tantalum cones. The TKAs revised during the procedure reported here included 10 posterior-stabilized implants and eight stemmed varus-valgus constrained implants. The indications for the revision included aseptic loosening of the tibial component (three patients), aseptic loosening of the femoral component (one patient), aseptic loosening of both components (one patient), and second-stage reimplantation for deep infection after antibiotic spacer placement (13 patients). The duration between the stages was no less than 5 weeks [20].
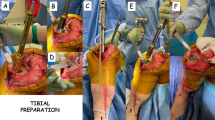
The surgical technique for implantation of femoral and tibial tantalum cones has been described [18, 24, 26, 27]. All tibial and femoral bone defects were carefully assessed intraoperatively using the AORI classification system [10] and rated as Type 2B in three femurs and three tibias and Type 3 in 10 femurs and nine tibias. A total of 26 tantalum cones were impacted into 18 knees. A femoral cone was implanted in six knees, a tibial cone was used in five, and tibial and femoral cones were implanted in seven (femoral and tibial cones in six knees and one femoral and two tibial cones in one knee [Fig. 1]). Two of the tibial cones were stepped. Once the cones were impacted, morselized cancellous bone allografts were used to fill voids between the periphery of the porous cone and the surrounding host bone in 10 knees. The NexGen® (Zimmer, Warsaw, IN, USA) revision system was used in all cases in conjunction with the tantalum cones. A constrained condylar (varus-valgus constrained) implant (LCCK®, Zimmer, Warsaw, IN, USA) was inserted in six knees and a rotating hinge knee implant (RHK®, Zimmer, Warsaw, IN, USA) in 12. The metaphyseal portions of the implants were cemented to the internal surface of the tantalum cones. To enhance implant fixation, stem extensions were used in all reconstructions. The senior surgeon’s (GG) preference was to use a 100-mm diaphyseal-engaging press-fit stem unless a diaphyseal defect required a longer stem or an osteopenic, wide intramedullary canal required cement fixation. Press-fit stems were used in 15 knees and cemented stems in three.
(A) A preoperative radiograph shows the knee of a 67-year-old patient with an infected TKA. (B) The radiograph obtained on postoperative Day 1 shows a revision TKA with use of three cones (one femoral and two tibial) to treat Type 3 bone defects. (C) A radiograph obtained after 5 years postoperative shows good fixation of the femoral and tibial cones and uncemented stems.
Offset stems were used 21 times (12 femoral and nine tibial), and straight stems were used 15 times (six femoral and nine tibial). Femoral and tibial stem extension lengths ranged from 100 mm to 155 mm, with the majority of patients (89%) having the 100-mm components. The patella was resurfaced in six knees. A primary resurfacing of previous unresurfaced patellae with an all-polyethylene component was done in five knees and revision of a previously placed patellar component with a tantalum patellar component was done in one knee. In the remaining 12 knees the patella was left unresurfaced because of good bone quality. Antibiotic-loaded bone cement was used routinely in all patients. SimplexTM P with Tobramycin Bone Cement (Stryker®, Mahwah NJ, USA) was used in 15 knees, and SimplexTM P Bone Cement (Stryker®) with vancomycin (1 g per batch of cement) and tobramycin (1.2 g per batch of cement) in three knees during a second-stage reimplantation for deep infection with beta-lactam-resistant organisms.
All patients were permitted weightbearing as tolerated using crutches or a cane as necessary, beginning on the first postoperative day. The rehabilitation protocol with active ROM exercises and progressive weightbearing was recommended for 6 weeks until full weightbearing was reached. All patients were able to walk without the aid of a cane by 3 months postoperatively.
Patients were followed clinically and radiographically. All patients were seen within 18 months of data collection for this study. Knee function was assessed with the Knee Society scoring system [19]. Radiographic review was performed by an independent fellowship-trained orthopaedic surgeon according to the Knee Society TKA radiographic evaluation system [13] modified for long-stemmed revision prostheses [29]. Radiographs, consisting of standing AP and lateral views of the knee, were evaluated for signs of fracture, migration, and osseointegration according to the criteria of Engh et al. [12]. Fluoroscopic views were not used, but a standardized protocol with experienced radiology technicians was used.
Knee Society clinical scores at last followup were compared with those collected before revision using a two-tailed paired t-test with SPSS 17.0 (SPSS Inc, Chicago, IL, USA). The preoperative evaluation was before the first-stage explantation for patients with sepsis.
Results
Two of the 18 patients in this study required subsequent surgery. Both reoperations were for recurrent infection in the second-stage reimplantation subgroup (two of 13) and none in the aseptic loosening subgroup (0 of five). The first patient had a recurrent infection develop 8 months postoperatively and underwent an arthrodesis because of extensive bone loss. The second patient had a recurrent infection develop after 36 months and underwent a second two-stage revision and subsequent above-knee amputation. In both circumstances, cones were noted to be well-fixed to the bone at the time of explant. Their removal was difficult and flexible osteotome blades and a high-speed pencil-tip burr were used for both patients. There were no reoperations for aseptic causes.
There was no evidence of loosening or migration of any implant at the latest followup. In addition, no radiolucent lines were seen between the cones and the adjacent tibial and femoral bones at the latest followup. On the immediate postoperative AP radiographs there was a 1-mm radiolucent line at the bone-cement interface adjacent to the tibial stem extension in one of the three patients with cemented stems. This line (unrelated to the cone) was considered completely stable and nonprogressive at the time of the final followup.
The mean Knee Society knee scores improved from 31 points (range, 13–69 points) preoperatively to 77 points (range, 39–100 points) postoperatively (p < 0.001). The mean Knee Society function scores improved from 22 points (range, 10–65 points) preoperatively to 65 points (range, 35–100 points) postoperatively (p < 0.001). Preoperatively the average flexion contracture was 6° (range, 0°–30°) and the average flexion was 88° (range, 70°–100°). At the time of the latest followup, the average flexion contracture was 3° (range, 0°–15°) and the average flexion was 105° (range, 90°–120°).
Discussion
The best treatment method for massive bone defects during revision knee arthroplasty remains uncertain. Options have included the use of impaction bone-grafting [22, 25, 38, 40, 44], structural bulk allografts [7, 11, 14, 16, 17, 28, 31, 39], and tumor-type megaprostheses [2]. Studies with structural allografts and tumor megaprostheses during revision knee arthroplasty have reported encouraging mid-term results, but the high number of complications is a concern. Complications with these techniques include infection, graft resorption, nonunion, failure of graft incorporation, concerns regarding disease transmission, aseptic loosening, and periprosthetic fracture [1, 7, 14, 17, 33]. Although the short-term results with tantalum cones have been promising [9, 18, 21, 23, 24, 26, 34–36, 42], to our knowledge, there have been no studies reporting mid-term outcomes with their use. We therefore sought to determine the mid-term results evaluating (1) reoperation rates for septic and aseptic causes, (2) radiologic findings of osseointegration, and (3) clinical outcomes based on the Knee Society score in patients who underwent revision knee arthroplasty with tantalum cones for significant bone loss.
This study has several limitations. First, as a retrospective series, it is reasonable to be concerned that some patients with severe defects might have been treated in other ways, or that patients with milder defects might have received cones. However, we carefully reviewed our institutional registry and found that this was not the case during the study period, therefore selection bias was unlikely to have influenced our findings. Second, there may be some selection bias against the use of press-fit stems in revision TKAs by the senior author (GG). Cemented stems were used sporadically during the study period by the senior author in selected patients with wide intramedullary canals and poor bone stock. Third, the patient cohort was relatively small but similar in size to cohorts in previous reports [9, 18, 21, 23, 24, 26, 34–36, 42]. Even so, with small series, it is impossible to detect uncommon complications and lower-frequency events that might be clinically important. Fourth, although mid-term at 5 years to 8 years, the followup was relatively short, and these patients therefore still need to be followed to make sure that fixation remains durable during longer service periods. Fifth, fluoroscopic positioning of the knee was not done and the presence of radiolucent lines between the cones and the adjacent tibial and femoral bone may be underestimated. We hoped to minimize this concern using a standardized protocol with experienced radiology technicians to ensure knee positioning, and by reviewing serial postoperative radiographs for reactive trabeculae formation at the cone-host bone interface. Sixth, this study was a combined analysis of femoral and tibial cones, resulting in small numbers of each. Larger numbers, longer followup, and perhaps multicenter trials will be needed to determine whether femoral and tibial cones are similarly durable.
In this cohort, two of 18 patients had a reoperation, both for recurrent infection. This compares favorably with the reoperation frequencies reported by Meneghini et al. [26] (27%), Howard et al. [18] (21%), and Lachiewicz et al. [23] (15%) for patients with AORI Types 2B and 3 defects. However, if we take into consideration only the reoperations for infection and aseptic loosening of the cone, our revision frequency was in line with the reoperation frequencies reported by Meneghini et al. [26] (two of 15) and Lachiewicz et al. [23] (two of 27), although it was higher than reported by Howard et al. [18] (0 of 24). Other studies reported reoperation rates similar to ours, between 5% and 14% [9, 21, 24, 34–36, 42]. However, in those cohorts cones also were used to reconstruct less-severe defects (AORI Type 2A).
The results of our patients may be compared with those of patients treated with structural bulk allografts during revision knee arthroplasty. Bauman et al. [1], Engh and Ammeen [11], and Chun et al. [6] reported reoperation rates of 23% (16 of 70), 19% (nine of 46), and 0% (0 of 27) in their series of 70, 46, and 27 knees respectively at minimum 5 years followup. Our revision frequency compares favorably with the reoperation frequencies reported by Bauman et al. [1] and Engh and Ammeen [11], but unfavorable with the rate reported by Chun et al. [6].
The proportion of patients who had infections in our study (two of 18) was comparable to that reported by Meneghini et al. [26] (13%) and Long and Scuderi [24] (13%), but was lower than reported in other studies [9, 18, 21, 23, 34–36, 42] (Table 1). Furthermore, in our cohort, 13 of the 18 revisions were second-stage reimplantations for deep infection and yet, at this longer followup, had an infection rate comparable to those in the other reports. Our data compare unfavorably with the infection frequencies reported in the bulk allografts studies [1, 6, 11]. Bauman et al. [1], Engh and Ammeen [11], and Chun et al. [6] reported infection rates of 7% (five of 70), 4% (two of 46), and 4% (one of 27) respectively in their series. However, only 9% to 11% of these reconstructions with bulk allografts were reimplantations for infection, whereas in our study 13 of the 18 revisions were second-stage reimplantations for deep infection. Our reinfection frequency (two of 13) compares favorably with those reported in the bulk allograft studies. Bauman et al. [1], Engh and Ammeen [11], and Chun et al. [6] reported reinfection rates of 33% (two of six), 17% (one of six), and 33% (one of three), respectively, in their series.
In our cohort, all cones showed signs of radiographic osseointegration at the latest followup. Our results are in agreement with those of other studies [9, 18, 21, 23, 24, 26, 34–36, 42]. In these studies, with a total of 285 cones used during 242 knee revisions, there are only two knees with cones showing no bone ingrowth (0.7%). Our radiographic osseointegration rate (18 of 18) compares favorably with those reported in the bulk allografts studies. Bauman et al. [1] reported two knees with progressive radiolucencies and two knees with asymptomatic allograft-host nonunion among the 33 knees with adequate radiographs. Engh and Ammeen [11] reported osteolytic lesions in six of 33 knees, however the osteolysis did not involve the metaphyseal area repaired with the bulk allograft. Compared with tantalum cones, the use of bulk allografts is associated with some disadvantages including nonunion of the graft, late collapse of the graft, and fracture of the graft.
Knee Society knee scores for our patients improved on average 46 points from their preoperative state to the latest followup and their functional scores improved by a mean 43 points. The increase between mean pre- and postoperative Knee Society scores in our patients was similar to the mean reported in other studies of cones [9, 18, 23, 26, 35, 36] and bulk allografts [1, 11].
The use of tantalum cones in the treatment of severe bone loss encountered during revision TKA was found to be successful in our patients with a minimum 5-year followup. These devices are a viable option for surgeons when faced with patients with severe bone loss during total knee revisions. Given that each revision presents its own challenges, tantalum cones can aid in providing a stable construct for joint reconstruction that show excellent osseointegration and clinical outcomes at mid-term followup. Further studies with longer followups are needed to confirm the durability of these reconstructions.
References
Bauman RD, Lewallen DG, Hanssen AD. Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res. 2009;467:818–824.
Berend KR, Lombardi AV Jr. Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009;467:485–492.
Bobyn JD, Pilliar RM, Cameron HU, Weatherly GC. The optimum pore size for the fixation of porous-surfaced metal implants by the ingrowth of bone. Clin Orthop Relat Res. 1980;150:263–270.
Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M. Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am. 2004;86(suppl 2):123–129.
Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914.
Chun CH, Kim JW, Kim SH, Kim BG, Chun KC, Kim KM. Clinical and radiological results of femoral head structural allograft for severe bone defects in revision TKA: a minimum 8-year follow-up. Knee. 2014;21:420–423.
Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty: a minimum five-year review. J Bone Joint Surg Am. 2001;83:404–411.
Cohen R. A porous tantalum trabecular metal: basic science. Am J Orthop (Belle Mead NJ). 2002;31:216–217.
Derome P, Sternheim A, Backstein D, Malo M. Treatment of large bone defects with trabecular metal cones in revision total knee arthroplasty: short term clinical and radiographic outcomes. J Arthroplasty. 2014;29:122–126.
Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175.
Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89:2640–2647.
Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128.
Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12.
Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE. Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Joint Surg Am. 1997;79:17–25.
Haas SB, Insall JN, Montgomery W 3rd, Windsor RE. Revision total knee arthroplasty with use of modular components with stems inserted without cement. J Bone Joint Surg Am. 1995;77:1700–1707.
Harris AI, Poddar S, Gitelis S, Sheinkop MB, Rosenberg AG. Arthroplasty with a composite of an allograft and a prosthesis for knees with severe deficiency of bone. J Bone Joint Surg Am. 1995;77:373–386.
Hockman DE, Ammeen D, Engh GA. Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. 2005;20:35–41.
Howard JL, Kudera J, Lewallen DG, Hanssen AD. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011;93:478–484.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14.
Jacobs C, Christensen CP, Berend ME. Static and mobile antibiotic-impregnated cement spacers for the management of prosthetic joint infection. J Am Acad Orthop Surg. 2009;17:356–368.
Jensen CL, Winther N, Schrøder HM, Petersen MM. Outcome of revision total knee arthroplasty with the use of trabecular metal cone for reconstruction of severe bone loss at the proximal tibia. Knee. 2014;21:1233–1237.
Jones RE, Skedros JG, Chan AJ, Beauchamp DH, Harkins PC. Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis. J Arthroplasty. 2001;16:279–287.
Lachiewicz PF, Bolognesi MP, Henderson RA, Soileau ES, Vail TP. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012;470:199–204.
Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009;24:1086–1092.
Lonner JH, Lotke PA, Kim J, Nelson C. Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res. 2002;404:145–151.
Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90:78–84.
Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement: surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2):131–138.
Mnaymneh W, Emerson RH, Borja F, Head WC, Malinin TI. Massive allografts in salvage revisions of failed total knee arthroplasties. Clin Orthop Relat Res. 1990;260:144–153.
Murray PB, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. Clin Orthop Relat Res. 1994;309:116–123.
Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208.
Parks NL, Engh GA. The Ranawat Award: Histology of nine structural bone grafts used in total knee arthroplasty. Clin Orthop Relat Res. 1997;345:17–23.
Patel JV, Masonis JL, Guerin J, Bourne RB, Rorabeck CH. The fate of augments to treat type-2 bone defects in revision knee arthroplasty. J Bone Joint Surg Br. 2004;86:195–199.
Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF. Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am. 2007;89:1735–1741.
Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83–92.
Rao BM, Kamal TT, Vafaye J, Moss M. Tantalum cones for major osteolysis in revision knee replacement. Bone Joint J. 2013;95:1069–1074.
Schmitz HC, Klauser W, Citak M, Al-Khateeb H, Gehrke T, Kendoff D. Three-year follow up utilizing tantal cones in revision total knee arthroplasty. J Arthroplasty. 2013;28:1556–1560.
Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21(6 suppl 2):83–86.
Suárez-Suárez MA, Murcia A, Maestro A. Filling of segmental bone defects in revision knee arthroplasty using morsellized bone grafts contained within a metal mesh. Acta Orthop Belg. 2002;68:163–167.
Tsahakis PJ, Beaver WB, Brick GW. Technique and results of allograft reconstruction in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;303:86–94.
Toms AD, Barker RL, Jones RS, Kuiper JH. Impaction bone-grafting in revision joint replacement surgery. J Bone Joint Surg Am. 2004;86:2050–2060.
Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009.
Villanueva-Martínez M, De la Torre-Escudero B, Rojo-Manaute JM, Ríos-Luna A, Chana-Rodriguez F. Tantalum cones in revision total knee arthroplasty: a promising short-term result with 29 cones in 21 patients. J Arthroplasty. 2013;28:988–993.
Wang JW, Hsu CH, Huang CC, Lin PC, Chen WS. Reconstruction using femoral head allograft in revision total knee replacement: an experience in Asian patients. Bone Joint J. 2013;95:643–648.
Whiteside LA. Morselized allografting in revision total knee arthroplasty. Orthopedics. 1998;21:1041–1043.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Geriatrics, Neurosciences, and Orthopedics, Agostino Gemelli University Hospital, Catholic University of the Sacred Heart, Rome, Italy.
About this article
Cite this article
De Martino, I., De Santis, V., Sculco, P.K. et al. Tantalum Cones Provide Durable Mid-term Fixation in Revision TKA. Clin Orthop Relat Res 473, 3176–3182 (2015). https://doi.org/10.1007/s11999-015-4338-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4338-2