Abstract
Background
The minimally invasive lateral transpsoas retroperitoneal approach to address lumbar stenosis offers advantages to traditional approaches, including sparing of the AP annulus and longitudinal ligament and less risk to the peritoneal contents and retroperitoneal vascular structures. Few studies have presented longitudinal measures of radiographic indirect decompression and relief of pain and restoration of function using the lateral approach to spine fusion.
Question/purposes
We determined (1) whether radiographic measures suggestive of decompression were achieved after surgery and maintained 1 year after surgery, (2) whether the intervention resulted in sustained improvements in patient-reported outcomes scores 1 year after surgery, and (3) the frequency of pseudarthrosis on CT scans at 1 year after surgery in patients with moderate or severe lumbar stenosis treated with the approach.
Methods
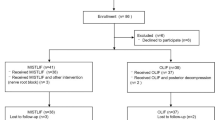
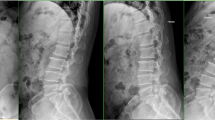
Between 2008 and 2012, 158 patients were surgically treated to alleviate symptoms associated with degenerative lumbar stenosis, of whom 60 (38%) were treated with lateral lumbar interbody fusion. Of these 60 patients, 36 (60%) received CT scans preoperatively and at 1-year postoperatively and were available for radiographic analysis. Of the 60 treated patients, 16 (27%) were lost to followup before 12 months, leaving the records of 44 patients available for review of patient-reported improvements in pain and return to function. Radiographic increases in disc height, foraminal area, and canal area were measured by one observer on CT scans postoperatively and at 1 year and compared to preoperative values. Patient-reported scores, including VAS pain score and Oswestry Disability Index (ODI), were collected preoperatively and at 3 and 12 months postoperatively.
Results
Increases in disc height (67%, p < 0.001), foraminal area (24%–31%, p < 0.001), and canal area (7%, p = 0.011) measured immediately postoperatively were sustained at 1-year followup. VAS pain score and ODI both improved (p < 0.001) at 3 months and were maintained at 1 year. No pseudarthroses were noted radiographically.
Conclusions
The lateral transpsoas approach to interbody fusion is capable of sustaining indirect decompression of the neural structures and resolving preoperative claudication and radiculopathy. A larger series of patients with longer followup should be studied to substantiate these early clinical results.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Arbit E, Pannullo S. Lumbar stenosis: a clinical review. Clin Orthop Relat Res. 2001;384:137–143.
Brier-Jones JE, Palmer DK, Inceoglu S, Cheng WK. Vertebral body fractures after transpsoas interbody fusion procedures. Spine J. 2011;11:1068–1072.
Cappuccino A, Cornwall GB, Turner AW, Fogel GR, Duong HT, Kim KD, Brodke DS. Biomechanical analysis and review of lateral lumbar fusion constructs. Spine (Phila Pa 1976). 2010;35:S361–S367.
Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092.
Castro C, Oliveira L, Amaral R, Marchi L, Pimenta L. Is the Lateral Transpsoas Approach Feasible for the Treatment of Adult Degenerative Scoliosis? Clin Orthop Relat Res. 2013 August 31 [Epub ahead of print].
Czerwein JK Jr, Thakur N, Migliori SJ, Lucas P, Palumbo M. Complications of anterior lumbar surgery. J Am Acad Orthop Surg. 2011;19:251–258.
Huskisson EC. Measurement of pain. Lancet. 1974;2:1127–1131.
Iida Y, Kataoka O, Sho T, Sumi M, Hirose T, Bessho Y, Kobayashi D. Postoperative lumbar spinal instability occurring or progressing secondary to laminectomy. Spine (Phila Pa 1976). 1990;15:1186–1189.
Issack PS, Cunningham ME, Pumberger M, Hughes AP, Cammisa FP Jr. Degenerative lumbar spinal stenosis: evaluation and management. J Am Acad Orthop Surg. 2012;20:527–535.
Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976). 2009;34:1963–1969.
Kepler CK, Sharma AK, Huang RC. Lateral transpsoas interbody fusion (LTIF) with plate fixation and unilateral pedicle screws: a preliminary report. J Spinal Disord Tech. 2011;24:363–367.
Lehman RA Jr, Kang DG. Commentary: an increasing awareness of the complications after transpsoas lumbar interbody fusion procedure. Spine J. 2011;11:1073–1075.
Marulanda GA, Nayak A, Murtagh R, Santoni BG, Billys JB, Castellvi AE. A Cadaveric Radiographic Analysis on the Effect of Extreme Lateral Interbody Fusion Cage Placement with Supplementary Internal Fixation on Indirect Spine Decompression. J Spinal Disord Tech. 2013 November 5 [Epub ahead of print].
McAfee PC, Phillips FM, Andersson G, Buvenenadran A, Kim CW, Lauryssen C, Isaacs RE, Youssef JA, Brodke DS, Cappuccino A, Akbarnia BA, Mundis GM, Smith WD, Uribe JS, Garfin S, Allen RT, Rodgers WB, Pimenta L, Taylor W. Minimally invasive spine surgery. Spine (Phila Pa 1976). 2010;35:S271–S273.
Nayak AN, Gutierrez S, Billys JB, Santoni BG, Castellvi AE. Biomechanics of lateral plate and pedicle screw constructs in lumbar spines instrumented at two levels with laterally placed interbody cages. Spine J. 2013;13:1331–1338.
Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 2010;35:S331–S337.
Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435–443.
Pratt RK, Fairbank JC, Virr A. The reliability of the Shuttle Walking Test, the Swiss Spinal Stenosis Questionnaire, the Oxford Spinal Stenosis Score, and the Oswestry Disability Index in the assessment of patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 2002;27:84–91.
Rodgers WB, Cox CS, Gerber EJ. Early complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech. 2010;23:393–397.
Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976). 2011;36:26–32.
Santoni BG, Alexander GE 3rd, Nayak A, Cabezas A, Marulanda GA, Murtagh R, Castellvi AE. Effects of inadvertant endplate fracture following lateral cage placement on range of motion and indirect spine decompression in lumbar spine fusion constructs. Int J Spine Surg. 2013;7:e101–e108.
Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976). 2005;30:670–674.
Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24:242–250.
Slosar PJ, Josey R, Reynolds J. Accelerating lumbar fusions by combining rhBMP-2 with allograft bone: a prospective analysis of interbody fusion rates and clinical outcomes. Spine J. 2007;7:301–307.
Thaler M, Lechner R, Gstottner M, Kobel C, Bach C. The use of beta-tricalcium phosphate and bone marrow aspirate as a bone graft substitute in posterior lumbar interbody fusion. Eur Spine J. 2013;22:1173–1182.
Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ. Perioperative complications in transforaminal lumbar interbody fusion versus anterior-posterior reconstruction for lumbar disc degeneration and instability. J Spinal Disord Tech. 2006;19:92–97.
Acknowledgments
The authors thank Deborah Warren RN, CCRP, Ann-Meredith Baldy, and Christopher Walker for their assistance with data collection and database management.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors certifies that he (AEC), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD (less than USD 10,000), from Crocker Spinal Technologies, Inc (Provo, UT, USA) and Nanovis, Inc (Columbia City, IN, USA); and an amount of USD (USD 10,000 to USD 100,000), from Alphatec Spine, Inc (Carlsbad, CA, USA). Each of the remaining authors certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Florida Orthopaedic Institute, Tampa, FL, USA.
About this article
Cite this article
Castellvi, A.E., Nienke, T.W., Marulanda, G.A. et al. Indirect Decompression of Lumbar Stenosis With Transpsoas Interbody Cages and Percutaneous Posterior Instrumentation. Clin Orthop Relat Res 472, 1784–1791 (2014). https://doi.org/10.1007/s11999-014-3464-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3464-6