Abstract
Background
Artificial bone graft substitutes are widely used to fill bony defects after curettage of benign tumors. We sought to evaluate the efficacy of one such bone graft substitute, geneX®, which contains tricalcium phosphate and calcium sulphate; however, during the course of this study we observed a high number of complications.
Questions/purposes
The primary aim of this prospective series was assessment of the effectiveness of geneX® concerning resorption profile and bone healing and remodeling after surgery. We present the types and frequencies of complications observed in patients treated for bone tumors by curettage and filling the defect using geneX®.
Methods
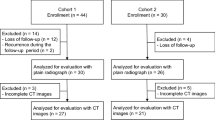
We planned to study 40 patients; however, after enrollment of the first 31 patients, the study was stopped as a result of serious complications. There were 20 female and 11 male patients with a mean age at surgery of 40 years (range, 6–71 years). Plain radiographs were obtained at different intervals during followup and CT scans were obtained 6 and 12 months postoperatively. Complications were assessed using a 5-point scale according to Goslings and Gouma.
Results
Five of the 31 patients (16%) had complications develop after surgery. In three cases, a sterile inflammation adjacent to the geneX® occurred, with delayed wound healing in two patients and local pain. In the third patient, geneX® produced moderate to severe skin damage in the area of the scar, needing revision surgery. In two other patients, inflammatory cystic formations developed in the soft tissues with sizes up to 15 cm, which gradually reduced in size with time. Overall, there were four Grade 1 complications and one Grade 2 according to Goslings and Gouma.
Conclusions
We concluded from this series of patients that geneX® causes soft tissue inflammation and pain with its use. Based on this experience we believe that this type of bone substitute should not be used in the treatment of bony defects.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Biocomposites L. geneX®; Injectable Bone graft with ZPC. Biocomposites, Ltd. Available at: http://www.biocomposites.com/ortho/Genex2.asp. Accessed May 1, 2013.
Evaniew N, Tan V, Parasu N, Jurriaans E, Finlay K, Deheshi B, Ghert M. Use of a calcium sulfate-calcium phosphate synthetic bone graft composite in the surgical management of primary bone tumors. Orthopedics. 2013;36:e216–222.
Goslings JC, Gouma DJ. What is a surgical complication? World J Surg. 2008;32:952.
Gupta MC, Theerajunyaporn T, Maitra S, Schmidt MB, Holy CE, Kadiyala S, Bruder SP. Efficacy of mesenchymal stem cell enriched grafts in an ovine posterolateral lumbar spine model. Spine (Phila Pa 1976). 2007;32:720–726; discussion 727.
Johnson LJ, Clayer M. Aqueous calcium sulphate as bone graft for voids following open curettage of bone tumours. ANZ J Surg. 2013;83:564–570.
Kelly CM, Wilkins RM. Treatment of benign bone lesions with an injectable calcium sulfate-based bone graft substitute. Orthopedics. 2004;27(1 suppl):S131–135.
Liu B, Lun DX. Current application of β-tricalcium phosphate composites in orthopaedics. Orthop Surg. 2012;4:139–144.
Okuda T, Ioku K, Yonezawa I, Minagi H, Kawachi G, Gonda Y, Murayama H, Shibata Y, Minami S, Kamihira S, Kurosawa H, Ikeda T. The effect of the microstructure of beta-tricalcium phosphate on the metabolism of subsequently formed bone tissue. Biomaterials. 2007;28:2612–2621.
Orii H, Sotome S, Chen J, Wang J, Shinomiya K. Beta-tricalcium phosphate (beta-TCP) graft combined with bone marrow stromal cells (MSCs) for posterolateral spine fusion. J Med Dent Sci. 2005;52:51–57.
Prosser GH, Baloch KG, Tillman RM, Carter SR, Grimer RJ. Does curettage without adjuvant therapy provide low recurrence rates in giant-cell tumors of bone? Clin Orthop Relat Res. 2005;435:211–218.
Saadoun S, Macdonald C, Bell BA, Papadopoulos MC. Dangers of bone graft substitutes: lessons from using GeneX. J Neurol Neurosurg Psychiatry. 2011;82:e3.
Van Hoff C, Samora JB, Griesser MJ, Crist MK, Scharschmidt TJ, Mayerson JL. Effectiveness of ultraporous beta-tricalcium phosphate (vitoss) as bone graft substitute for cavitary defects in benign and low-grade malignant bone tumors. Am J Orthop (Belle Mead NJ). 2012;41:20–23.
Walsh WR, Langdown AJ, Auld JW, Stephens P, Yu Y, Vizesi F, Bruce WJ, Pounder N. Effect of low intensity pulsed ultrasound on healing of an ulna defect filled with a bone graft substitute. J Biomed Mater Res B Appl Biomater. 2008;86:74–81.
Walsh WR, Morberg P, Yu Y, Yang JL, Haggard W, Sheath PC, Svehla M, Bruce WJ. Response of a calcium sulfate bone graft substitute in a confined cancellous defect. Clin Orthop Relat Res. 2003;406:228–236.
Yang HL, Zhu XS, Chen L, Chen CM, Mangham DC, Coulton LA, Aiken SS. Bone healing response to a synthetic calcium sulfate/β-tricalcium phosphate graft material in a sheep vertebral body defect model. J Biomed Mater Res B Appl Biomater. 2012;100:1911–1921.
Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3:192–195.
Zhan BL, Ye Z. [Significance of percutaneous vertebroplasty with Genex in the treatment of thoracolumbar burst fractures]. Zhongguo Gu Shang. 2011;24:223–226.
Zhang S, Jiang J, Zhu Q, Huang Z. [Biomechanical study of vertebroplasty with geneX((R)) cement augmentation in a calf osteoporotic vertebral compression fracture model][in Chinese]. Nan Fang Yi Ke Da Xue Xue Bao. 2012;32:843–846.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Friesenbichler, J., Maurer-Ertl, W., Sadoghi, P. et al. Adverse Reactions of Artificial Bone Graft Substitutes: Lessons Learned From Using Tricalcium Phosphate geneX® . Clin Orthop Relat Res 472, 976–982 (2014). https://doi.org/10.1007/s11999-013-3305-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3305-z