Abstract
Background
Lumbar degenerative scoliosis is a common condition in the elderly. Open traditional surgical approaches are associated with high-morbidity complication rates. Less invasive options may carry fewer risks in this patient population. A minimally disruptive lateral transpsoas retroperitoneal technique to accomplish interbody fusion was developed to avoid the morbidity of traditional open surgery, but this approach as an anterior stand-alone construction has not been reported yet for the treatment of adult degenerative scoliosis.
Questions/purposes
We determined (1) the clinical outcomes (VAS scores for back and leg, Oswestry Disability Index), (2) the radiographic outcomes (Cobb angle, lumbar lordosis, sacral slope, high-grade subsidence, osseous fusion), and (3) the reoperation and complication rates in an older population undergoing this surgical approach.
Methods
Between 2004 and 2008, 62 patients were treated surgically for adult degenerative scoliosis, of whom 46 (74%) were treated with stand-alone lateral lumbar interbody fusion; 11 of these (24%) were lost to followup before 24 months, leaving the records of 35 patients (nine men, 26 women; mean ± SD age, 68 ± 10 years) available for this retrospective review. General indications for this approach included neurogenic claudication and radicular symptoms with history of chronic low-back pain. A total of 107 levels were treated (mean, three; range, one to seven). Clinical and radiographic outcomes were assessed at a followup of 24 months.
Results
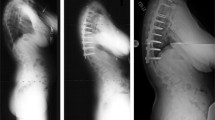
Mean VAS back pain scores improved from 85 mm preoperatively to 27 mm at latest followup (p < 0.001). VAS leg pain scores improved from 91 mm to 24 mm (p < 0.001). Oswestry Disability Index scores improved from 51 to 29 (p < 0.001). Coronal alignment improved from Cobb angles of 21° to 12° (p < 0.001). Lumbar lordosis improved from 33° to 41° (p < 0.001). Sacral slope was enhanced from 28° to 35° (p < 0.001). Fusion rate was 84% at final evaluation. High-grade subsidence was seen in 10 patients (29%). Three patients (9%) needed further surgical intervention.
Conclusions
Use of the lateral approach achieved reasonable coronal and sagittal correction, as well as improvements in pain and function, in mild scoliotic deformities; however, subsidence was a concern, occurring in 29% of patients. Questions still remain regarding the need for additional supplementation or the use of wider cages to prevent subsidence.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.




Similar content being viewed by others
References
Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 2011;15:92–96.
Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech. 2008;21:459–467.
Anand N, Rosemann R, Khalsa B, Baron EM. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28:E6.
Arnold PM, Anderson KK, McGuire RA Jr. The lateral transpsoas approach to the lumbar and thoracic spine: a review. Surg Neurol Int. 2012;3:S198–S215.
Bridwell KH. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:1–8.
Burkus JK, Foley K, Haid RW, LeHuec JC. Surgical Interbody Research Group—radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus. 2001;10:E11.
Cappuccino A, Cornwall GB, Turner AW, Fogel GR, Duong HT, Kim KD, Brodke DS. Biomechanical analysis and review of lateral lumbar fusion constructs. Spine (Phila Pa 1976). 2010;35(26 suppl):S361–S367.
Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092.
Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ). 2003;32:77–82.
Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28:E8.
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007;32:2238–2244.
Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine: the influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543.
Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146.
Fogel GR, Toohey JS, Neidre A, Brantigan JW. Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: x-ray films and helical computed tomography scans compared with surgical exploration of fusion. Spine J. 2008;8:570–577.
Goldstein C, Drew B. When is a spine fused? Injury. 2011;42:306–313.
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J. 2005;14:551–558.
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007;7:379–386.
Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM. A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976). 2010;35(26 suppl):S322–S330.
Kepler CK, Huang RC, Sharma AK, Meredith DS, Metitiri O, Sama AA, Girardi FP, Cammisa FP. Factors influencing segmental lumbar lordosis after lateral transpsoas interbody fusion. Orthop Surg. 2012;4:71–75.
Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, Uribe JS. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37:1268–1273.
Le TV, Burkett CJ, Deukmedjian AR, Uribe JS. Postoperative lumbar plexus injury following lumbar retroperitoneal transpsoas minimally invasive lateral interbody fusion. Spine (Phila Pa 1976). 2013;38:E13–E20.
Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19:110–118.
Marchi L, Abdala, N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. ScienceWorldJournal. 2012;2012:456346.
Marchi L, Oliveira L, Coutinho E, Pimenta L. The importance of the anterior longitudinal ligament in lumbar disc arthroplasty: 36-month follow-up experience in extreme lateral total disc replacement. Int J Spine Surg. 2012;6:18–23.
Mundis GM, Akbarnia BA, Phillips FM. Adult deformity correction through minimally invasive lateral approach techniques. Spine (Phila Pa 1976). 2010;35(26 suppl):S312–S321.
Niemeyer TK, Koriller M, Claes L, Kettler A, Werner K, Wilke HJ. In vitro study of biomechanical behavior of anterior and transforaminal lumbar interbody instrumentation techniques. Neurosurgery. 2006;59:1271–1276.
Oliveira L, Marchi L, Coutinho E, Abdala N, Pimenta L. The use of rh-BMP2 in standalone eXtreme Lateral Interbody Fusion (XLIF®): clinical and radiological results after 24 months follow-up. World Spinal Column J. 2010;1:19–25.
Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 2010;35(26 suppl):S331–S337.
Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435–443.
Ploumis A, Wu C, Fischer G, Mehbod AA, Wu W, Faundez A, Transfeldt EE. Biomechanical comparison of anterior lumbar interbody fusion and transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2008;21:120–125.
Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech. 2005;18:337–346.
Rodgers WB, Cox CS, Gerber EJ. Early Complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech. 2010;23:393–397.
Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: the promise of minimally invasive surgery. Spine (Phila Pa 1976). 2010;35(26 suppl):S355–S360.
Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24:242–250.
Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28:E1.
Transfeldt EE, Topp R, Mehbod AA, Winter RB. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine (Phila Pa 1976). 2010;35:1872–1875.
Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174–183.
Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28:1–8.
Wu CH, Wong CB, Chen LH, Niu CC, Tsai TT, Chen WJ. Instrumented posterior lumbar interbody fusion for patients with degenerative lumbar scoliosis. J Spinal Disord Tech. 2008;21:310–315.
Acknowledgments
The authors thank Thabata Bueno MS for her assistance with paper review.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors certifies that he (LP), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD (USD 100,001 to USD 1,000,000), from NuVasive, Inc, CA, USA.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Instituto de Patologia da Coluna, São Paulo, Brazil.
About this article
Cite this article
Castro, C., Oliveira, L., Amaral, R. et al. Is the Lateral Transpsoas Approach Feasible for the Treatment of Adult Degenerative Scoliosis?. Clin Orthop Relat Res 472, 1776–1783 (2014). https://doi.org/10.1007/s11999-013-3263-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3263-5