Abstract
Background
Individuals with spastic hemiplegic cerebral palsy are typically high functioning and walk without assistive devices. The involved limb is usually smaller and shorter, although it is not clear whether the difference in muscle volume has an impact on walking capacity.
Questions/purposes
We determined the volume of muscles important for propulsion and related that volume to concentric muscle work during walking on the hemiplegic and noninvolved sides in patients with cerebral palsy.
Patients and Methods
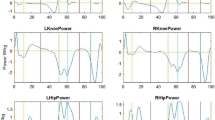
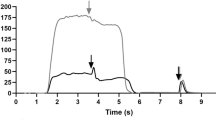
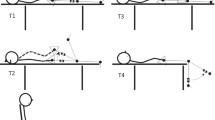
We studied 46 patients (mean age, 17.6 years; range, 13–24 years) with spastic hemiplegic cerebral palsy. We assessed muscle volume using MRI and concentric muscle work in the sagittal plane from the hip, knee, and ankle using three-dimensional gait analysis. Patients were classified by Winters’ criteria to assess the involvement of cerebral palsy and movement pattern during walking.
Results
On the hemiplegic side, muscles were smaller, except for the gracilis muscle, and concentric muscle work from the ankle plantar flexors, knee extensors, and hip flexors and extensors was lower compared to the noninvolved side. Hip extensor work was higher on the hemiplegic and the noninvolved sides compared to a control group of 14 subjects without cerebral palsy. Hemiplegic to noninvolved volume ratios correlated with work ratios (r = 0.40–0.66). The Winters classification and previous calf muscle surgery predicted work ratios.
Conclusions
Our observations of smaller muscles on the hemiplegic side and changes in muscle work on both sides can help us distinguish between primary deviations that may potentially be treatable and compensatory mechanisms that should not be treated.




Similar content being viewed by others
References
Akagi R, Takai Y, Ohta M, Kanehisa H, Kawakami Y, Fukunaga T. Muscle volume compared to cross-sectional area is more appropriate for evaluating muscle strength in young and elderly individuals. Age Ageing. 2009;38:564–569.
Damiano DL. Activity, activity, activity: rethinking our physical therapy approach to cerebral palsy. Phys Ther. 2006;86:1534–1540.
Damiano DL, Arnold AS, Steele KM, Delp SL. Can strength training predictably improve gait kinematics? A pilot study on the effects of hip and knee extensor strengthening on lower-extremity alignment in cerebral palsy. Phys Ther. 2010;90:269–279.
Dobson F, Morris ME, Baker R, Graham HK. Gait classification in children with cerebral palsy: a systematic review. Gait Posture. 2007;25:140–152.
Elder GC, Kirk J, Stewart G, Cook K, Weir D, Marshall A, Leahey L. Contributing factors to muscle weakness in children with cerebral palsy. Dev Med Child Neurol. 2003;45:542–550.
Fukunaga T, Miyatani M, Tachi M, Kouzaki M, Kawakami Y, Kanehisa H. Muscle volume is a major determinant of joint torque in humans. Acta Physiol Scand. 2001;172:249–255.
Gage J. The Treatment of Gait Problems in Cerebral Palsy. London, UK: MacKeith; 2004.
Goldberg EJ, Requejo PS, Fowler EG. Joint moment contributions to swing knee extension acceleration during gait in children with spastic hemiplegic cerebral palsy. J Biomech. 2010;43:893–899.
Johnson DL, Miller F, Subramanian P, Modlesky CM. Adipose tissue infiltration of skeletal muscle in children with cerebral palsy. J Pediatr. 2009;154:715–720.
Lampe R, Grassl S, Mitternacht J, Gerdesmeyer L, Gradinger R. MRT-measurements of muscle volumes of the lower extremities of youths with spastic hemiplegia caused by cerebral palsy. Brain Dev. 2006;28:500–506.
Lang TA, Secic M. How to Report Statistics in Medicine. Philadelphia, PA: American College of Physicians; 2006.
Liu MQ, Anderson FC, Schwartz MH, Delp SL. Muscle contributions to support and progression over a range of walking speeds. J Biomech. 2008;41:3243–3252.
Liu XC, Fabry G, Molenaers G, Lammens J, Moens P. Kinematic and kinetic asymmetry in patients with leg-length discrepancy. J Pediatr Orthop. 1998;18:187–189.
McDowell BC, Kerr C, Kelly C, Salazar J, Cosgrove A. The validity of an existing gait classification system when applied to a representative population of children with hemiplegia. Gait Posture. 2008;28:442–447.
McNee AE, Gough M, Morrissey MC, Shortland AP. Increases in muscle volume after plantarflexor strength training in children with spastic cerebral palsy. Dev Med Child Neurol. 2009;51:429–435.
Miller F. Cerebral Palsy. New York, NY: Springer; 2005.
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol. 1998;85:115–122.
Mockford M, Caulton JM. Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Pediatr Phys Ther. 2008;20:318–333.
Modlesky CM, Cavaiola ML, Smith JJ, Rowe DA, Johnson DL, Miller F. A DXA-based mathematical model predicts midthigh muscle mass from magnetic resonance imaging in typically developing children but not in those with quadriplegic cerebral palsy. J Nutr. 2010;140:2260–2265.
Olney SJ, MacPhail HE, Hedden DM, Boyce WF. Work and power in hemiplegic cerebral palsy gait. Phys Ther. 1990;70:431–438.
Ounpuu S, Muik E, Davis RB 3rd, Gage JR, DeLuca PA. Rectus femoris surgery in children with cerebral palsy. Part II. A comparison between the effect of transfer and release of the distal rectus femoris on knee motion. J Pediatr Orthop. 1993;13:331–335.
Riad J, Coleman S, Lundh D, Broström E. Arm posture score and arm movement during walking: a comprehensive assessment in spastic hemiplegic cerebral palsy. Gait Posture. 2011;33:48–53.
Riad J, Haglund-Akerlind Y, Miller F. Classification of spastic hemiplegic cerebral palsy in children. J Pediatr Orthop. 2007;27:758–764.
Riad J, Haglund-Akerlind Y, Miller F. Power generation in children with spastic hemiplegic cerebral palsy. Gait Posture. 2008;27:641–647.
Saraph V, Zwick EB, Steinwender G, Auner C, Schneider F, Linhart W. Leg lengthening as part of gait improvement surgery in cerebral palsy: an evaluation using gait analysis. Gait Posture. 2006;23:83–90.
Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T. Gait compensations caused by foot deformity in cerebral palsy. Gait Posture. 2010;32:226–230.
Steele KM, Seth A, Hicks JL, Schwartz MS, Delp SL. Muscle contributions to support and progression during single-limb stance in crouch gait. J Biomech. 2010;43:2099–2105.
Suckling J, Sigmundsson T, Greenwood K, Bullmore ET. A modified fuzzy clustering algorithm for operator independent brain tissue classification of dual echo MR images. Magn Reson Imaging. 1999;17:1065–1076.
Südhoff I, de Guise JA, Nordez A, Jolivet E, Bonneau D, Khoury V, Skalli W. 3D-patient-specific geometry of the muscles involved in knee motion from selected MRI images. Med Biol Eng Comput. 2009;47:579–587.
Winters TF Jr, Gage JR, Hicks R. Gait patterns in spastic hemiplegia in children and young adults. J Bone Joint Surg Am. 1987;69:437–441.
Acknowledgments
We thank Scott Coleman for help with illustrations; Mesfin Tessma with the statistics; Eleanor Kelly, Deepti Bajaj, Brianne Mulrooney, and K. Michael Rowley with image processing; and Joshua T. Kirby with technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
The work was performed at Skaraborg Hospital and Karolinska Institutet.
About this article
Cite this article
Riad, J., Modlesky, C.M., Gutierrez-Farewik, E.M. et al. Are Muscle Volume Differences Related to Concentric Muscle Work During Walking in Spastic Hemiplegic Cerebral Palsy?. Clin Orthop Relat Res 470, 1278–1285 (2012). https://doi.org/10.1007/s11999-011-2093-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2093-6