Abstract
Background
The literature contains proposals for creating value by creating exceptional patient experiences rather than simply improving services. However, few articles describe replicable applications focused on the patient experience.
Questions/purposes
We (1) describe the refinement and exportation of an approach that focuses on the patient and family experience; and (2) report changes in patient satisfaction, infection rates, length of stay, mortality rates, clinical indicators, staff turnover, and cost.
Methods
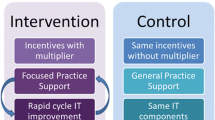
The Patient and Family-Centered Care Methodology and Practice (PFCC M/P) is a six-step process: (1) selecting a care experience needing improvement; (2) establishing a guiding council; (3) evaluating the current state; (4) developing a permanent working group; (5) creating a shared vision of the ideal experience; and (6) identifying improvement projects to address the gap between the current and ideal experience. We assessed patient satisfaction, changes in clinical indicators, staff turnover, and cost in three clinical programs.
Results
In TJA, patient satisfaction is at the 99th percentile; length of stay, infection rates, and mortality rates are substantially better than the national average. In trauma, patient satisfaction increased, time in cervical collars decreased, staff turnover decreased, and the incidence of lost patient belongings was eliminated. In orthopaedic spine, patient satisfaction is higher than the national average, average time for transfer to bed decreased (%), length of stay decreased, and average discharge time decreased. Each of these would have a positive impact on cost.
Conclusions
PFCC M/P offers a road map for redefining value as what is important to patients and families.



Similar content being viewed by others
References
Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006;15:307–310.
Brown T. Change by Design. New York: HarperCollins Publishers, Inc; 2009.
Christensen C. The Innovator’s Dilemma: The Revolutionary Book That Will Change the Way You Do Business. New York: HarperCollins Publishers, Inc; 2003.
DiGioia A, Greenhouse PK. Patient and family shadowing: creating urgency for change. J Nurs Adm. 2011;41:23–28.
DiGioia A, Greenhouse PK, Levison MS. Patient and family centered collaborative care: an orthopaedic model. Clin Orthop Relat Res. 2007;463:13–19.
DiGioia A, Lorenz H, Greenhouse PK, Bertoty D, Rocks S. A patient centered model to improve metrics without cost increase: viewing all care through the eyes of patients and families. J Nurs Adm. 2010;40:540–546.
Herzlinger R. Who Killed Health Care? America’s $2 Trillion Medical Problem—and the Consumer-driven Cure. New York: McGraw Hill; 2007.
Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 1999.
Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. Washington, DC: National Academies Press; 2001.
Jones CB, Gates M. The cost and benefits of nurse turnover: a business case for nurse retention. Online Journal of Issues in Nursing. Available at: http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/Tableofcontents/Volume122007/No3Sept07/NurseRetention/aspx. Accessed July 23, 2011.
McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645.
Meyer H. At UPMC, improving care processes to serve patients better and cut costs. Health Aff. 2011;30:400–403.
Pine JB. Staging the Healthcare Experience. Available at: www.couragetobefirst.com/Courage%20to%20Be%20First_Staging%20Healthcare%20Experience_Joe%20Pine.pdf. Accessed August 19, 2010.
Pine JB, Gilmore JH. The Experience Economy: Work is Theatre & Every Business a Stage. Boston: Harvard Business School Press; 1999.
Porter ME, Teisberg EO. Redefining Health Care: Creating Value-based Competition on Results. Boston: Harvard Business School Press; 2006.
Simon HA. The Sciences of the Artificial. Boston: Massachusetts Institute of Technology Press Books; 1996.
Acknowledgments
We thank Holly Lorenz, David Bertoty, Dee Nicholas, and Mary Beth Pais as well as the entire PFCC Level I Trauma and Surgical Care Experience Working Groups and the Orthopaedic Spine Project Improvement Team at UPMC Presbyterian, all of whom played key roles in the refinement and exportation of the PFCC M/P. Also, special thanks to Patricia Embree and the staff of the Innovation Center of UPMC for their help in guiding these teams.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases and that all investigations were conducted in conformity with ethical principles of research.
Appendix 1. Glossary of terms
Appendix 1. Glossary of terms
Caregiver = Defined broadly as any person within the healthcare setting whose work touches a patient’s or family’s care experience, including the doctors, nurses, therapists, technicians, dietitians, appointment schedulers, parking attendants, janitors, and even hospital leaders, purchase and supply chain employees, and financial representatives who the patient and family might never see.
Guiding Council = A small group of committed healthcare professionals, including administrators, to: (1) serve as champions to guide and expand the use of the PFCC M/P; and (2) to perform the essential function of communicating with all levels of the organization.
PFCC Toolbox = Tools to help gather accurate information about patient and family experiences. The PFCC Toolbox includes Shadowing, Care Flow Mapping, storytelling, advisory councils, surveys (phone and paper), digital recording systems, and real-time location systems.
Shadowing = Following patients and families through every step of a defined care experience pathway to observe and record the care experience through their eyes.
About this article
Cite this article
DiGioia, A.M., Greenhouse, P.K. Care Experience-based Methodologies: Performance Improvement Roadmap to Value-driven Health Care. Clin Orthop Relat Res 470, 1038–1045 (2012). https://doi.org/10.1007/s11999-011-2051-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2051-3