Opinion statement
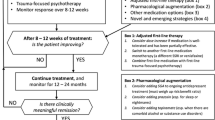
Posttraumatic stress disorder (PTSD) is often comorbid with chronic migraine (CM) and chronic tension-type headache (CTTH). Trauma-focused cognitive behavioral psychotherapies, selective serotonin reuptake inhibitors (SSRIs), and venlafaxine have demonstrated efficacy in the treatment of PTSD. Amitriptyline, topiramate, sodium valproate, and botulinum toxin A are efficacious for treatment of chronic daily headache (CDH). Treatment studies on individuals with CDH and comorbid PTSD, however, are limited. As such, multiple therapeutic agents or modes of interventions typically are necessary, such that comprehensive treatment simultaneously utilizes approaches with established efficacy for each individual condition.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pascual J, Colás R, Castillo J. Epidemiology of chronic daily headache. Curr Pain Headache Rep. 2001;5:529–36.
Scher AI, Stewart WF, Liberman J, et al. Prevalence of frequent headache in a population sample. Headache. 1998;38:497–506.
Stovner LJ, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210.
Buse DC, Manack AN, Fanning KM, et al. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52:1456–70.
Lipton RB, Bigal ME, Hamelsky SW, et al. Headache: epidemiology and impact. In: Silberstein SD, Lipton RB, Dodick DW, editors. Wolff’s headache and other head pain. 8th ed. New York: Oxford University Press; 2008. p. 45–62.
Natoli JL, Manack A, Dean B, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30:599–609.
Schwartz BS, Stewart WF, Simon D, et al. Epidemiology of tension-type headache. JAMA. 1998;279:381–3.
Buse DC, Silberstein SD, Manack AN, et al. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260:1960–9.
Buse DC, Manack A, Serrano D, et al. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. 2010;81:428–32.
Radat F, Lantéri-Minet M, Nachit-Ouinekh F, et al. The GRIM2005 study of migraine consultation in France. III: psychological features of subjects with migraine. Cephalalgia. 2008;29:338–50.
Ashina S, Serrano D, Lipton RB, et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13:615–24.
Radat F, Creac’h C, Swendsen JD, et al. Psychiatric comorbidity in the evolution from migraine to medication overuse headache. Cephalalgia. 2005;25:519–22.
Peterlin BL, Rosso AL, Sheftell FD, et al. Post-traumatic stress disorder, drug abuse and migraine: new findings from the National Comorbidity Survey Replication (NCS-R). Cephalalgia. 2011;31:235–44.
Tietjen GE, Khubchandani J, Herial NA, et al. Adverse childhood experiences are associated with migraine and vascular biomarkers. Headache. 2012;52:920–9.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C., 2013.
Tietjen GE, Brandes JL, Digre KB, et al. History of childhood maltreatment is associated with comorbid depression in women with migraine. Neurology. 2007;69:959–68.
Tietjen GE, Brandes JL, Peterlin L, et al. Childhood maltreatment and migraine (Part I). Prevalence and adult revictimization: a multicenter headache clinic survey. Headache. 2010;50:20–31.
Tietjen GE, Brandes JL, Peterlin L, et al. Childhood maltreatment and migraine (Part II). Emotional abuse as a risk factor for headache chronification. Headache. 2010;50:32–41.
Tietjen GE, Peterlin DO. Childhood abuse and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:869–79.
Afari N, Harder LH, Madra NJ, et al. PTSD, combat injury, and headache in veterans returning from Iraq/Afghanistan. Headache. 2009;49:1267–76.
Bryan CJ, Hernandez AM. Predictors of post-traumatic headache severity among deployed military personnel. Headache. 2011;51:945–53.
Theeler BJ, Erickson JC. Posttraumatic headache in military personnel and veterans of the Iraq and Afghanistan conflicts. Curr Treat Options Neurol. 2012;14:36–49.
Theeler BJ, Flynn FG, Erickson JC. Chronic daily headache in U.S. soldiers after concussion. Headache. 2012;52:732–8.
Theeler B, Lucas S, Riechers II RG, et al. Post-traumatic headaches in civilians and military personnel: a comparative, clinical review. Headache. 2013;53:881–900.
Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–32.
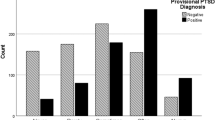
Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49:541–51.
Peterlin BL, Tietjen G, Meng S, et al. Post-traumatic stress disorder in episodic and chronic migraine. Headache. 2008;48:517–22.
Smitherman TA, Kolivas ED. Trauma exposure versus posttraumatic stress disorder: relative associations with migraine. Headache. 2013;53:775–86.
Seng EK, Driscoll MA, Brandt CA, et al. Prescription headache medication in OEF/OIF veterans: results from the Women Veterans Cohort Study. Headache. 2013;53:1312–22.
American Psychiatric Association. Practice guideline for the treatment of patients with Acute Stress Disorder and Posttraumatic Stress Disorder. Arlington: American Psychiatric Publishing, 2009. http://psychiatryonline.org/content.aspx?bookid=28§ionid=1670530#52282 Accessed June 12, 2014.
Australian National Health and Medical Research Council, Australian Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of adults with Acute Stress Disorder and Posttraumatic Stress Disorder. Melbourne; 2007. www.nhmrc.gov.au/publications/synopses/mh13syn.htm. Accessed June 12, 2014.
Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2007;190:97–104.
Foa EB, Keane TM, Friedman MJ, Cohen J. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York: Guilford Press; 2009.
Management of Post-Traumatic Stress Working Group. VA/DoD clinical practice guideline for the management of post-traumatic stress. Washington, DC: Office of Quality and Performance, Department of Veterans Affairs; 2010. Available from http://www.healthquality.va.gov/ptsd.ptsd_full.pdf. Accessed June 12, 2014.
National Institute for Health and Clinical Excellence. Post-traumatic stress disorder. NICE clinical guidelines, no. 26. London: RCPsych Publications; 2005.
Cahill SP, Carrigan MH, Frueh BC. Does EMDR work? And if so, why?: A critical review of controlled outcome and dismantling research. J Anxiety Disord. 1999;13:5–33.
Davidson PR, Parker KCH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol. 2001;69:305–16.
Lohr JM, Tolin DF, Lilienfeld SO. Efficacy of eye movement desensitization and reprocessing: implications for behavior therapy. Behav Ther. 1998;29:123–56.
Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. In: Foa EB, Keane TM, Friedman MJ (eds). New York: Guilford Press; 2000.
Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for post traumatic stress disorder [PTSD] [Review]. Cochrane Libr. 2009;1:1–108.
Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non-SSRIs in post-traumatic stress disorder: an update with recommendations. Drugs. 2004;64:383–404.
Jeffreys M, Capehart B, Friedman MJ. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev. 2012;49:703–15.
Jonas DE, Cusack K, Forneris CA, et al. Psychological and Pharmacological Treatments for Adults With Posttraumatic Stress Disorder (PTSD). Comparative Effectiveness Review No. 92. (Prepared by the RTI International–University of North Carolina Evidence-based Practice Center under Contract No. 290-2007-10056-I.) AHRQ Publication No. 13-EHC011-EF. Rockville, MD: Agency for Healthcare Research and Quality; April 2013. This is a very recent review of treatments for PTSD under the auspices of the Agency for Healthcare Research and Quality.
Steckler T, Risbrough V. Pharmacological treatment of PTSD – established and new approaches. Neuropharmacology. 2012;62:617–27.
Pae CU, Lim HK, Ajwani N, Lee C, Patkar AA. Extended-release formulation of venlafaxine in the treatment of post-traumatic stress disorder. Expert Rev Neurother. 2007;7:603–15.
Watts BV, Schnurr PP, Mayo L, et al. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiatry. 2013;74:e541–50.
Andrus MR, Gilbert E. Treatment of civilian and combat-related posttraumatic stress disorder with topiramate. Ann Pharmacother. 2010;44:1810–6.
van Minnen A, Arntz A, Keijsers GP. Prolonged exposure in patients with chronic PTSD: predictors of treatment outcome and dropout. Behav Res Ther. 2002;40:439–57.
Evers S, Jensen R. Treatment of medication overuse headache – guideline of the EFNS headache panel. Eur J Neurol. 2011;18:1115–21.
Evers S, Marziniak M. Clinical features, pathophysiology, and treatment of medication-overuse headache. Lancet Neurol. 2010;9:391–401.
Seifert TD, Evans RW. Posttraumatic headache: a review. Curr Pain Headache Rep. 2010;14:292–8.
Vargas BB. Posttraumatic headache in combat soldiers and civilians: what factors influence the expression of tension-type versus migraine headache? Curr Pain Headache Rep. 2009;13:470–3.
Couch JR. Update on chronic daily headache. Curr Treat Options Neurol. 2011;13:41–55. This paper reviews in detail the pharmacologic options for treating CDH.
Halker RB, Hastriter EV, Dodick DW. Chronic daily headache: an evidence-based and systematic approach to a challenging problem. Neurology. 2011;76:37–43. This paper reviews the causes of CDH and various treatment options.
Bendtsen L, Jensen R, Olesen J. A non-selective (amitriptyline), but not a selective (citalopram), serotonin reuptake inhibitor is effective in the prophylactic treatment of chronic tension-type headache. J Neurol Neurosurg Psychiatry. 1996;61:285–90.
Couch JR. Amitriptyline versus placebo study group. Amitriptyline in the prophylactic treatment of migraine and chronic daily headache. Headache. 2011;51:33–51.
Holroyd KA, O'Donnell FJ, Stensland M, et al. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA. 2001;285:2208–15.
Bartolini M, Silvestrini M, Taffi R, et al. Efficacy of topiramate and valproate in chronic migraine. Clin Neuropharmacol. 2005;28:277–9.
Diener HC, Bussone G, Van Oene JC, et al. Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27:814–23.
Diener HC, Dodick DW, Goadsby PJ, et al. Utility of topiramate for the treatment of patients with chronic migraine in the presence or absence of acute medication overuse. Cephalalgia. 2009;29:1021–7.
Silberstein SD, Lipton RB, Dodick DW, et al. Efficacy and safety of topiramate for the treatment of chronic migraine: a randomized, double-blind, placebo-controlled trial. Headache. 2007;47:170–80.
Silvestrini M, Bartolini M, Coccia M, et al. Topiramate in the treatment of chronic migraine. Cephalalgia. 2003;23:820–4.
Yurekli VA, Akhan G, Kutuhan S, et al. The effect of sodium valproate on chronic daily headache and its subgroups. J Headache Pain. 2008;9:37–41.
Freitag FG, Diamond S, Diamond ML, et al. Divalproex in the long-term treatment of chronic daily headache. Headache. 2001;41:271–8.
Zissis N, Harmoussi S, Vlaikidis N, et al. A randomized, double-blind, placebo-controlled study of venlafaxine XR in out-patients with tension-type headache. Cephalalgia. 2007;27:315–24.
Aurora SK, Dodick DW, Turkel CC, et al. PREEMPT 1 Chronic Migraine Study Group. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793–803.
Diener HC, Dodick DW, Aurora SK, et al. PREEMPT 2 Chronic Migraine Study Group. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30:804–14.
Jackson JL, Kuriyama A, Hayashino Y. Botulinum toxin A for prophylactic treatment of migraine and tension headaches in adults: a meta-analysis. JAMA. 2012;307:1736–45.
Blumenfeld A, Silberstein SD, Dodick DW, et al. Method of injection of onabotulinumtoxinA for chronic migraine: a safe, well-tolerated, and effective treatment paradigm based on the PREEMPT clinical program. Headache. 2010;50:1406–18.
Goslin RE, Gray RN, McCrory DC, et al. Behavioral and physical treatments for migraine headache. Rockville (MD): Agency for Health Care Policy and Research (US); 1999 Feb. (Technical Reviews, No. 2.2.) Available from: http://www.ncbi.nlm.nih.gov/books/NBK45267/?part. Accessed March 10, 2014.
McCrory DC, Penzien DB, Hasselblad V, et al. Evidence report: behavioral and physical treatments for tension-type and cervicogenic headache. Des Moines: Foundation for Chiropractic Education and Research, Product No. 2085; 2001.
Penzien DB, Rains JC, Lipchik GL, et al. Behavioral interventions for tension-type headache: overview of current therapies and recommendation for a self-management model for chronic headache. Curr Pain Headache Rep. 2004;8:489–99.
Rains JC, Penzien DB, McCrory DC, et al. Behavioral headache treatment: history, review of the empirical literature, and methodological critique. Headache. 2005;45:S91–S108.
Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55:754–62.
Trautmann E, Lackschewitz H, Kröner-Herwig B. Psychological treatment of recurrent headache in children and adolescents –a meta-analysis. Cephalalgia. 2006;26:1411–26.
Powers SW, Kashikar-Zuck SM, Allen JR, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents: a randomized clinical trial. JAMA. 2013;310:2622–30. This RCT, although focused on adolescents, underscores the value of combining behavioral and pharmacologic interventions for optimal CM outcomes.
Schafer AM, Rains JC, Penzien DB, et al. Direct costs of preventive headache treatments: comparison of behavioral and pharmacologic approaches. Headache. 2011;51:985–91.
Mo’tamedi H, Rezaiemaram P, Tavallaie A. The effectiveness of a group-based acceptance and commitment additive therapy on rehabilitation of female outpatients with chronic headache: preliminary findings reducing 3 dimensions of headache impact. Headache. 2012;52:1106–19.
Moja L, Cusi C, Sterzi R, et al. Selective serotonin re-uptake inhibitors (SSRIs) for preventing migraine and tension-type headaches. Cochrane Database Syst Rev. 2005;3, CD002919. doi:10.1002/14651858.CD002919.pub2.
Smitherman TA, Walters AB, Maizels M, et al. The use of antidepressants for headache prophylaxis. CNS Neurosci Ther. 2011;17:462–9.
Lipchik GL, Smitherman TA, Penzien DB, et al. Basic principles and techniques of cognitive-behavioral therapies for comorbid psychiatric symptoms among headache patients. Headache. 2006;46:119–32.
Compliance with Ethics Guidelines
Conflict of Interest
Todd A. Smitherman has received research support from Merck. Anna Katherine Black and Christal N. Davis declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Headache
Rights and permissions
About this article
Cite this article
Smitherman, T.A., Black, A.K. & Davis, C.N. Treatment of PTSD and Chronic Daily Headache. Curr Treat Options Neurol 16, 312 (2014). https://doi.org/10.1007/s11940-014-0312-7
Published:
DOI: https://doi.org/10.1007/s11940-014-0312-7