Abstract
Purpose of review
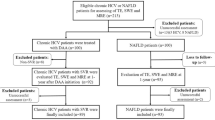
In the USA, there is a growing prevalence of liver disease, particularly from alcohol and fatty liver, as well as improvements in hepatitis C therapy that should be adjusted for level of fibrosis. There is accordingly a great need for rapid non-invasive fibrosis testing (NIT) to determine who should be referred for specialty care, started on specific therapies, screened for varices and malignancy, and selected for clinical trials.
Recent findings
It is not only the accuracy of NIT that matters, but the order in which they are applied and the population selected for screening. All NIT to date have high negative predictive value for ruling out advanced fibrosis, and despite high specificity, have limited positive predictive value due to the relative infrequency of advanced fibrosis in screened populations.
Summary
A testing algorithm based on primary care screening (e.g., with FIB-4) followed by referral for specialty confirmatory testing (e.g., vibration-controlled transient elastography) would best fit most practice models. This focused review will characterize the most validated non-invasive blood tests and imaging and discuss their practical applications for real-world use.

Similar content being viewed by others
References and Recommended Reading
Dulai PS, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65:1557–65. https://doi.org/10.1002/hep.29085.
Angulo P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397.e310. https://doi.org/10.1053/j.gastro.2015.04.043.
de Franchis R. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743–52. https://doi.org/10.1016/j.jhep.2015.05.022.
Younossi ZM, et al. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. https://doi.org/10.1002/hep.28431.
Kabbany MN, Conjeevaram Selvakumar PK, Watt K, Lopez R, Akras Z, Zein N, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of National Health and Nutrition Examination Survey Data. Am J Gastroenterol. 2017;112:581–7. https://doi.org/10.1038/ajg.2017.5.
Dang K, Hirode G, Singal A, Sundaram V, Wong RJ. Alcoholic liver disease epidemiology in the United States: a retrospective analysis of 3 US databases. Am J Gastroenterol. 2019. https://doi.org/10.14309/ajg.0000000000000380.
Xiao G, et al. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66:1486–501. https://doi.org/10.1002/hep.29302.
Armstrong GL, Wasley A, Simard EP, McQuillan G, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–14. https://doi.org/10.7326/0003-4819-144-10-200605160-00004.
Hofmeister MG, et al. Estimating prevalence of hepatitis C virus infection in the United States, 2013–2016. Hepatology. 2019;69:1020–31. https://doi.org/10.1002/hep.30297.
Kowdley KV, Wang CC, Welch S, Roberts H, Brosgart CL. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology. 2012;56:422–33. https://doi.org/10.1002/hep.24804.
Kim WR. Epidemiology of hepatitis B in the United States. Hepatology. 2009;49:S28–34. https://doi.org/10.1002/hep.22975.
Patel EU, Thio CL, Boon D, Thomas DL, Tobian AAR. Prevalence of hepatitis B and hepatitis D virus infections in the United States, 2011-2016. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz001.
Tabibian JH, Ali AH, Lindor KD. Primary sclerosing cholangitis, part 1: epidemiology, etiopathogenesis, clinical features, and treatment. Gastroenterol Hepatol. 2018;14:293–304.
Liang H, Manne S, Shick J, Lissoos T, Dolin P. Incidence, prevalence, and natural history of primary sclerosing cholangitis in the United Kingdom. Medicine. 2017;96:e7116. https://doi.org/10.1097/md.0000000000007116.
Lu M, et al. Increasing prevalence of primary biliary cholangitis and reduced mortality with treatment. Clin Gastroenterol Hepatol. 2018;16:1342–1350.e1341. https://doi.org/10.1016/j.cgh.2017.12.033.
Francque S, Vonghia L, Ramon A, Michielsen P. Epidemiology and treatment of autoimmune hepatitis. Hepat Med. 2012;4:1–10. https://doi.org/10.2147/hmer.s16321.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy. Hepatology. 2009;49:1017–44. https://doi.org/10.1002/hep.22742.
Mehta SH, Lau B, Afdhal NH, Thomas DL. Exceeding the limits of liver histology markers. J Hepatol. 2009;50:36–41. https://doi.org/10.1016/j.jhep.2008.07.039.
Anstee QM, et al. Noninvasive tests accurately identify advanced fibrosis due to NASH: baseline data from the STELLAR Trials. Hepatology. 2019;70:1521–30. https://doi.org/10.1002/hep.30842.Large NASH population with both histopathology and NIT testing. Compares the predictive value of different NIT tests used in isolation, with variable cutoffs, combined, and sequentially.
Soresi M, Giannitrapani L, Cervello M, Licata A, Montalto G. Non invasive tools for the diagnosis of liver cirrhosis. World J Gastroenterol. 2014;20:18131–50. https://doi.org/10.3748/wjg.v20.i48.18131.
Alkhouri N. Putting it all together: noninvasive diagnosis of fibrosis in nonalcoholic fatty liver disease in adults and children. Clin Liver Dis. 2017;9:134–7. https://doi.org/10.1002/cld.636.
Asrani SK. Noninvasive diagnosis of liver fibrosis in adults. Clin Liver Dis. 2017;9:121–4. https://doi.org/10.1002/cld.632.
Loomba R, et al. Validation of serum test for advanced liver fibrosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2019;17:1867–1876.e1863. https://doi.org/10.1016/j.cgh.2018.11.004.
Poynard T, Imbert-Bismut F, Munteanu M, Messous D, Myers RP, Thabut D, et al. Overview of the diagnostic value of biochemical markers of liver fibrosis (FibroTest, HCV FibroSure) and necrosis (ActiTest) in patients with chronic hepatitis C. Comp Hepatol. 2004;3:8. https://doi.org/10.1186/1476-5926-3-8.
Sebastiani G, Castera L, Halfon P, Pol S, Mangia A, di Marco V, et al. The impact of liver disease aetiology and the stages of hepatic fibrosis on the performance of non-invasive fibrosis biomarkers: an international study of 2411 cases. Aliment Pharmacol Ther. 2011;34:1202–16. https://doi.org/10.1111/j.1365-2036.2011.04861.x.
Wei R, Wang J, Wang X, Xie G, Wang Y, Zhang H, et al. Clinical prediction of HBV and HCV related hepatic fibrosis using machine learning. EBioMedicine. 2018;35:124–32. https://doi.org/10.1016/j.ebiom.2018.07.041.
Zarski JP, Sturm N, Guechot J, Paris A, Zafrani ES, Asselah T, et al. Comparison of nine blood tests and transient elastography for liver fibrosis in chronic hepatitis C: the ANRS HCEP-23 study. J Hepatol. 2012;56:55–62. https://doi.org/10.1016/j.jhep.2011.05.024.
Wai CT, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–26. https://doi.org/10.1053/jhep.2003.50346.
Vallet-Pichard A, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–6. https://doi.org/10.1002/hep.21669.
Omran D, Yosry A, Darweesh SK, Nabeel MM, el-Beshlawey M, Saif S, et al. Enhanced liver fibrosis test using ELISA assay accurately discriminates advanced stage of liver fibrosis as determined by transient elastography fibroscan in treatment naive chronic HCV patients. Clin Exp Med. 2018;18:45–50. https://doi.org/10.1007/s10238-017-0463-4.
Harrison SA. Utilization of FibroScan testing in hepatitis C virus management. Gastroenterol Hepatol. 2015;11:187–9.
Vuppalanchi R, et al. Performance characteristics of vibration-controlled transient elastography for evaluation of nonalcoholic fatty liver disease. Hepatology. 2018;67:134–44. https://doi.org/10.1002/hep.29489.
Bonder A, Afdhal N. Utilization of FibroScan in clinical practice. Curr Gastroenterol Rep. 2014;16:372. https://doi.org/10.1007/s11894-014-0372-6.
Park CC, et al. Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease. Gastroenterology. 2017;152:598–607.e592. https://doi.org/10.1053/j.gastro.2016.10.026.
Imajo K, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016;150:626–637.e627. https://doi.org/10.1053/j.gastro.2015.11.048.
Bohte AE, de Niet A, Jansen L, Bipat S, Nederveen AJ, Verheij J, et al. Non-invasive evaluation of liver fibrosis: a comparison of ultrasound-based transient elastography and MR elastography in patients with viral hepatitis B and C. Eur Radiol. 2014;24:638–48. https://doi.org/10.1007/s00330-013-3046-0.
Thiele M, Madsen BS, Hansen JF, Detlefsen S, Antonsen S, Krag A. Accuracy of the enhanced liver fibrosis test vs FibroTest, elastography, and indirect markers in detection of advanced fibrosis in patients with alcoholic liver disease. Gastroenterology. 2018;154:1369–79. https://doi.org/10.1053/j.gastro.2018.01.005.
Cui J, Ang B, Haufe W, Hernandez C, Verna EC, Sirlin CB, et al. Comparative diagnostic accuracy of magnetic resonance elastography vs. eight clinical prediction rules for non-invasive diagnosis of advanced fibrosis in biopsy-proven non-alcoholic fatty liver disease: a prospective study. Aliment Pharmacol Ther. 2015;41:1271–80. https://doi.org/10.1111/apt.13196.
Hagstrom H, Talback M, Andreasson A, Walldius G, Hammar N. Ability of noninvasive scoring systems to identify individuals in the population at risk for severe liver disease. Gastroenterology. 2020;158:200–14. https://doi.org/10.1053/j.gastro.2019.09.008. Large Swedish cohort determination of the predictive value of five noninvasive clinical fibrosis scores. Clinical scores have excellent NPV but poor PPV due to low prevalence of disease in the general population.
Afdhal NH, et al. Accuracy of fibroscan, compared with histology, in analysis of liver fibrosis in patients with hepatitis B or C: a United States multicenter study. Clin Gastroenterol Hepatol. 2015;13:772–779.e771–773. https://doi.org/10.1016/j.cgh.2014.12.014.
Cardoso AC, Carvalho-Filho RJ, Stern C, Dipumpo A, Giuily N, Ripault MP, et al. Direct comparison of diagnostic performance of transient elastography in patients with chronic hepatitis B and chronic hepatitis C. Liver Int. 2012;32:612–21. https://doi.org/10.1111/j.1478-3231.2011.02660.x.
Hartl J, et al. Transient elastography in autoimmune hepatitis: timing determines the impact of inflammation and fibrosis. J Hepatol. 2016;65:769–75. https://doi.org/10.1016/j.jhep.2016.05.023.
Siddiqui MS, et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:156–163.e152. https://doi.org/10.1016/j.cgh.2018.04.043.
Cheung A, et al. Defining improvement in nonalcoholic steatohepatitis for treatment trial endpoints: recommendations from the liver forum. Hepatology. 2019;70:1841–55. https://doi.org/10.1002/hep.30672. Pertinent discussion on the need for NIT testing that can corrrelate with changes in histology and meaningful clinical outcomes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joseph Redman declares that he has no conflict of interest. Richard K. Sterling declares that he has no conflict of interest
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Liver
Rights and permissions
About this article
Cite this article
Redman, J., Sterling, R.K. Non-invasive Assessment of Liver Fibrosis. Curr Treat Options Gastro 18, 255–269 (2020). https://doi.org/10.1007/s11938-020-00285-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-020-00285-z