Abstract
Introduction
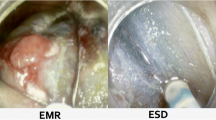
Colonic laterally spreading lesions (LSL) are increasingly managed using endoscopic methods that comprise two main techniques: endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD).
Purpose of Review
In this review, we aimed to review the most recent literature on selection of the best endoscopic technique in the management of colonic LSL.
Recent Findings
EMR and ESD are complimentary techniques in the management of patients with colonic LSL.
Summary
EMR is safe and effective in most patients with LSL, except for cancers with submucosal invasion in whom R0 resection is favored.




Similar content being viewed by others
Abbreviations
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- G-LSL:
-
Granular laterally spreading lesion
- LSL:
-
Laterally spreading lesion
- NG-LSL:
-
Non-granular laterally spreading lesion
- SMIC:
-
Submucosa-invasive cancer
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bourke MJ, Neuhaus H, Bergman JJ. Endoscopic submucosal dissection: indications and application in Western endoscopy practice. Gastroenterology. 2018;154:1887–900.
Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2017;49:270–97.
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417–34.
Rex DK, Hassan C, Bourke MJ. The colonoscopist’s guide to the vocabulary of colorectal neoplasia: histology, morphology, and management. Gastrointest Endosc. 2017;86:253–63.
Moss A, Bourke MJ, Williams SJ, Hourigan LF, Brown G, Tam W, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology. 2011;140:1909–18.
Uraoka T, Saito Y, Matsuda T, Ikehara H, Gotoda T, Saito D, et al. Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut. 2006;55:1592–7.
• Burgess NG, Hourigan LF, Zanati SA, et al. Risk stratification for covert invasive cancer among patients referred for colonic endoscopic mucosal resection: a large multicenter cohort. Gastroenterology. 2017;153:732–742.e1. This study examines endoscopic features of colonic LSL associated with malignant lesions.
Klein A, Bourke MJ. Advanced polypectomy and resection techniques. Gastrointest Endosc Clin N Am. 2015;25:303–33.
Hassan C, Repici A, Sharma P, Correale L, Zullo A, Bretthauer M, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut. 2016;65:806–20.
Tate DJ, Bahin FF, Desomer L, Sidhu M, Gupta V, Bourke MJ. Cold-forceps avulsion with adjuvant snare-tip soft coagulation (CAST) is an effective and safe strategy for the management of non-lifting large laterally spreading colonic lesions. Endoscopy. 2018;50:52–62.
Sidhu M, Tate DJ, Desomer L, Brown G, Hourigan LF, Lee EYT, et al. The size, morphology, site, and access score predicts critical outcomes of endoscopic mucosal resection in the colon. Endoscopy. 2018;50:684–92.
Tate DJ, Desomer L, Klein A, et al. Adenoma recurrence after piecemeal colonic EMR is predictable: the Sydney EMR recurrence tool. Gastrointest Endosc. 2017;85:647–656.e6.
Klein A, Jayasekeran V, Hourigan LF, Tate DJ, Singh R, Brown GJ, et al. 812b a multi-center randomized control trial of thermal ablation of the margin of the post endoscopic mucosal resection (EMR) mucosal defect in the prevention of adenoma recurrence following EMR: preliminary results from the SCAR; study. Gastroenterology. 2016;150:S1266–7.
Moss A, Williams SJ, Hourigan LF, Brown G, Tam W, Singh R, et al. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut. 2015;64:57–65.
Desomer L, Tutticci N, Tate DJ, Williams SJ, McLeod D, Bourke MJ. A standardized imaging protocol is accurate in detecting recurrence after EMR. Gastrointest Endosc. 2017;85:518–26.
Fahrtash-Bahin F, Holt BA, Jayasekeran V, et al. Snare tip soft coagulation achieves effective and safe endoscopic hemostasis during wide-field endoscopic resection of large colonic lesions (with videos). Gastrointest Endosc. 2013;78:158–163.e1.
Bahin FF, Rasouli KN, Byth K, Hourigan LF, Singh R, Brown GJ, et al. Prediction of clinically significant bleeding following wide-field endoscopic resection of large sessile and laterally spreading colorectal lesions: a clinical risk score. Am J Gastroenterol. 2016;111:1115–22.
Albeniz E, Fraile M, Ibanez B, et al. A scoring system to determine risk of delayed bleeding after endoscopic mucosal resection of large colorectal lesions. Clin Gastroenterol Hepatol. 2016;14:1140–7.
Bahin FF, Rasouli KN, Williams SJ, Lee EY, Bourke MJ. Prophylactic clipping for the prevention of bleeding following wide-field endoscopic mucosal resection of laterally spreading colorectal lesions: an economic modeling study. Endoscopy. 2016;48:754–61.
Burgess NG, Bassan MS, McLeod D, Williams SJ, Byth K, Bourke MJ. Deep mural injury and perforation after colonic endoscopic mucosal resection: a new classification and analysis of risk factors. Gut. 2017;66:1779–89.
Swan MP, Bourke MJ, Moss A, Williams SJ, Hopper A, Metz A. The target sign: an endoscopic marker for the resection of the muscularis propria and potential perforation during colonic endoscopic mucosal resection. Gastrointest Endosc. 2011;73:79–85.
Fuccio L, Hassan C, Ponchon T, et al. Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:74–86.e17.
Takamaru H, Saito Y, Yamada M, et al. Clinical impact of endoscopic clip closure of perforations during endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2016;84:494–502.e1.
• Fujiya M, Tanaka K, Dokoshi T, et al. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc. 2015;81:583–95. This meta-analysis summarized the efficacy and safety of EMR compared to ESD in the managmeent of colonic LSL.
Bahin FF, Heitman SJ, Rasouli KN, Mahajan H, McLeod D, Lee EYT, et al. Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions: a cost-effectiveness analysis. Gut. 2017. https://doi.org/10.1136/gutjnl-2017-313823. This study examines the cost-effectiveness of EMR and ESD in the management of colonic LSL.
Schmidt A, Bauerfeind P, Gubler C, Damm M, Bauder M, Caca K. Endoscopic full-thickness resection in the colorectum with a novel over-the-scope device: first experience. Endoscopy. 2015;47:719–25.
Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag HJ, Messmann H, et al. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut. 2018;67:1280–9.
Awadie H, Repici A, Bourke MJ. Endoscopic management of large nonpedunculated colorectal polyps: selective treatment algorithms are needed. Endoscopy. 2017;49:214–6.
Heitman SJ, Bourke MJ. Endoscopic submucosal dissection and EMR for large colorectal polyps: “the perfect is the enemy of good”. Gastrointest Endosc. 2017;86:87–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ji Young Bang declares that she has no conflict of interest. Michael Bourke declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Endoscopy
Rights and permissions
About this article
Cite this article
Bang, J.Y., Bourke, M.J. Selection of EMR and ESD for Laterally Spreading Lesions of the Colon. Curr Treat Options Gastro 16, 376–385 (2018). https://doi.org/10.1007/s11938-018-0198-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-018-0198-7