Opinion statement
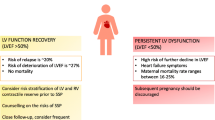
After concerns about survival and recovery from peripartum cardiomyopathy (PPCM), the question commonly asked is, “Is it safe to have another pregnancy?” While important advances have been made in the past decade in the recognition and treatment of PPCM, we still do not know why some apparently recovered PPCM mothers have a relapse of heart failure in a subsequent pregnancy. Knowing that some risk for relapse is always present, careful monitoring of the post-PPCM pregnancy is currently the best way to enable earlier diagnosis with institution of effective evidence-based treatment. In that situation it is reassuring to observe that when a subsequent pregnancy begins with recovered left ventricular systolic function to echocardiographic ejection fraction ≥0.50, even with relapse, the response to treatment is good with much more favorable outcomes. On the other hand, beginning the subsequent pregnancy with echocardiographic ejection fraction <0.50 greatly increases the risk for less favorable outcomes. This article summarizes the current state of knowledge; addresses the important questions facing patients, their families, and caregivers; and identifies the need for a prospective multi-center study of women with post-PPCM pregnancies. The reality is that an estimated 10 % to 20 % of apparently recovered PPCM mothers are going to relapse in a post-PPCM pregnancy; but we do not yet know why. Nevertheless, the lowest risk for relapse is experienced by those who (1) recover to left ventricular ejection fraction 0.55 prior to another pregnancy; (2) have no deterioration of left ventricular ejection fraction after phasing out angiotensin-converting enzyme inhibitor/angiotensin-receptor blocker treatment following recovery; and perhaps, (3) demonstrate adequate contractile reserve on exercise echocardiography.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley CM, Hosenpud JD, et al. Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA. 2000;283:1183–8.
Elkayam U. Clinical characteristics of peripartum cardiomyopathy in the United States: diagnosis, prognosis, and management. J Am Coll Cardiol. 2011;58:659–67.
Sliwa K, Fett JD, Elkayam U. Seminar: peripartum cardiomyopathy. Lancet. 2006;368:687–93.
Fett JD. Peripartum cardiomyopathy: a puzzle closer to solution. World J Cardiol. 2014;6((3):81–114.
Elkayam U, Tummala PP, Rao K, Akhter MW, Karaalp IS, Wani OR, et al. Maternal and fetal outcomes of subsequent pregnancies in women with peripartum cardiomyopathy. N Engl J Med. 2001;344(21):1567–71. Erratum in: N Engl J Med.2001;345(7):552.
Fett JD, Christie LG, Murphy JG. Outcomes of subsequent pregnancy after peripartum cardiomyopathy: a case series from Haiti. Ann Intern Med. 2006;145:30–4.
Sliwa K, Forster O, Zhanje F, Candy G, Kachope J, Essop R. Outcome of subsequent pregnancy in patients with documented peripartum cardiomyopathy. Am J Cardiol. 2004;93:1441–3.
Habli M, O’Brien T, Nowack E, Khoury S, Barton JR, Sibai B. Peripartum cardiomyopathy: prognostic factors for long-term maternal outcome. Am J Obstet Gynecol. 2008;199:415.e1–5.
Modi KA, Illum S, Jariatul K, Caldito G, Reddy PC. Poor outcome of indigent patients with peripartum cardiomyopathy in the United States. Am J Obstet Gynecol. 2009;201:171.e1–5.
Fett JD, Fristoe KL, Welsh SN. Risk of heart failure relapse in subsequent pregnancy among peripartum cardiomyopathy mothers. Int J Gynecol Obstet. 2010;109:34–6.
Mandal D, Mandal S, Mukherjee D, Biswas SC, Maiti TK. Pregnancy and subsequent pregnancy outcomes in peripartum cardiomyopathy. J Obstet Gynaecol Res. 2011;37:222–7.
pt?>Shani H, Kuperstein R, Berlin A, Arad M, Goldenberg I, Simchen MJ. Peripartum cardiomyopathy—risk factors, characteristics and long-term follow-up. J Perinat Med. 2014.
McNamara DM, Damp J Elkayam U, Hsich E, Ewald G, Cooper LT, et al. Abstract 12898: Myocardial recovery at six months in peripartum cardiomyopathy: results of the NHLBI multicenter IPAC study Circulation. 2013;22 (Suppl). First prospective North American study of new PPCM subjects with important identification of predictors of recovery vs non-recovery.
Goland S, Modi K, Bitar F, Janmohamed M, Mirocha JM, Lawrence SC, et al. Clinical profile and predictors of complications in peripartum cardiomyopathy. J Card Fail. 2009;15:645–50.
Fett JD, Christie LG, Carraway RD, Murphy JG. Five-year prospective study of the incidence and prognosis of peripartum cardiomyopathy at a single institution. Mayo Clin Proc. 2005;80:1602–6.
McNamara DM, Starling RC, Cooper LT, Boehmer JP, Mather PJ, Janosko KM, et al. IMAC Investigators. Clinical and demographic predictors of outcomes in recent onset dilated cardiomyopathy: results of the IMAC (Intervention in Myocarditis and Acute Cardiomyopathy)-2 study. J Am Coll Cardiol. 2011;58:1112–8. Identifies sub-set of 39 PPCM subjects in whom echocardiographic measure of left ventricular remodeling/dilation serves as strong predictor of non-recovery.
Johnson-Coyle L, Jensen L, Sobey A, American College of Cardiology Foundation, American Heart Association. Peripartum cardiomyopathy: review and practice guidelines. Am J Crit Care. 2012;21:89–98.
Fett JD. Personal Commentary: monitoring subsequent pregnancy in recovered peripartum cardiomyopathy mothers. Crit Pathw Cardiol. 2010;9:1–3.
Tanaka H, Tanabe M, Simon MA, Starling RC, Markham D, Thohan V, et al. Left ventricular mechanical dyssynchrony in acute onset cardiomyopathy: association of its resolution with improvements in ventricular function. JACC Cardiovasc Imaging. 2011;4:445–56.
Lampert MB, Weinert L, Hibbard J, Korcarz C, Lindheimer M, Lang RM. Contractile reserve in patients with peripartum cardiomyopathy and recovered left ventricular function. Am J Obstet Gynecol. 1997;176:189–95.
Pellikka PA, Naqueh SF, Elhendy AA, Kuehl CA, Sawada SG. American Society of Echocardiography. American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echjocardiogr. 2007;20:1021–41.
Sicari R, Nihoyannopoulos P, Evangelista A, et al. European Association of Echocardiography. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr. 2008;9:415–37.
Lang CC, Karlin P, Haythe J, Tsao L, Mancini DM. Ease of noninvasive measurement of cardiac output coupled with peak V02 determination at rest and during exercise in patients with heart failure. Am J Cardiol. 2007;99:404–5.
Blauwet LA, Cooper LT. Diagnosis and management of peripartum cardiomyopathy. Heart. 2011;97:1970–81.
Fett JD. Earlier detection can help avoid many serious complications of peripartum cardiomyopathy. Futur Cardiol. 2013;9(6):809–16.
Fett JD. Validation of a self-test for early diagnosis of heart failure in peripartum cardiomyopathy. Crit Pathw Cardiol. 2011;10:44–5. Identifies simple, inexpensive self-test to help with early identification of heart failure in PPCM subjects; early recognition helps in diagnosis while heart function relatively intact, and therefore recovery more likely.
Rana S, Powe CE, Salahuddin S, Verlohren S, Perschel FH, Levine RJ, et al. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation. 2012;125:911–9.
Rana S, Shahul S, Rowe GC, Jang C, Liu L, Hacker MR, et al. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature. 2012;485:333–8.
American Heart Association. In: Fuster V, editor. The AHA guidelines and scientific statements handbook. Oxford: Wiley; 2009.
European Society of Cardiology. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur Heart J. 2012;33:1787–847.
Bernstein PS, Magriples U. Cardiomyopathy in pregnancy: a retrospective study. Am J Perinatol. 2001;18:163–8.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. James D. Fett, Dr. Tina P. Shah, and Dr. Dennis M. McNamara each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Fett, J.D., Shah, T.P. & McNamara, D.M. Why Do Some Recovered Peripartum Cardiomyopathy Mothers Experience Heart Failure With a Subsequent Pregnancy?. Curr Treat Options Cardio Med 17, 354 (2015). https://doi.org/10.1007/s11936-014-0354-x
Published:
DOI: https://doi.org/10.1007/s11936-014-0354-x