Opinion statement
The central event in the development of allograft vasculopathy is the inflammatory response to immune-mediated and nonimmune-mediated endothelial damage. This response is characterized by the release of inflammatory cytokines, upregulation of cell-surface adhesion molecules, and subsequent binding of leukocytes. Growth factors stimulate smooth muscle cell proliferation and circulating progenitor cells are recruited to sites of arterial injury leading to neointima formation. Because of its diffuse nature, intravascular ultrasound is more sensitive than angiography for early diagnosis. Proliferation signal inhibitors (PSIs) have the capacity to slow vasculopathy progression by inhibiting smooth muscle cell proliferation, but its side effects profile makes its use as a first line agent difficult. Retransplantation is still the only definitive therapy but is available only in selected cases. The current hope is that immunomodulation at the time of transplant could induce long-term tolerance and graft accommodation, leading to less vasculopathy.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
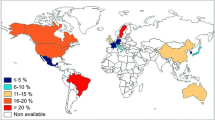
Stehlik J, Edwards LB, Kucheryavaya AY, et al. International Society of Heart and Lung Transplantation. The registry of the International Society for Heart and Lung Transplantation: 29th official adult heart transplant report-2012. J Heart Lung Transplant. 2012;31:1052–64.
Mancini D, Pinney S, Burkhoff D, et al. Use of rapamycin slows progression of cardiac transplantation vasculopathy. Circulation. 2003;108:48–53.
Rogers NJ, Lechler RI. Allorecognition. Am J Transplant. 2001;1:97–102.
Mitchell RN, Libby P. Vascular remodeling in transplant vasculopathy. Circ Res. 2007;100:967–78.
Wehner JR, Fox-Talbot K, Halushka MK, et al. B cells and plasma cells in coronaries of chronically rejected cardiac transplants. Transplantation. 2010;89:1141–8.
Bahlmann FH, DeGroot K, Duckert T, et al. Endothelial progenitor cell proliferation and differentiation is regulated by erythropoietin. Kidney Int. 2003;64:1648–52.
Choi J, Enis DR, Koh KP, et al. T lymphocyte-endothelial cell interactions. Annu Rev Immunol. 2004;22:683–709.
Salomon RN, Hughes CC, Schoen FJ, et al. Human coronary transplantation-associated arteriosclerosis. Evidence for a chronic immune reaction to activated graft endothelial cells. Am J Pathol. 1991;138:791–8.
Zhang XP, Kelemen SE, Eisen HJ. Quantitative assessment of cell adhesion molecule gene expression in endomyocardial biopsy specimens from cardiac transplant recipients using competitive polymerase chain reaction. Transplantation. 2000;70:505–13.
Nabel EG, Shum L, Pompili VJ, et al. Direct transfer of transforming growth factor beta 1 gen into arteries stimulates fibrocellular hyperplasia. Proc Natl Acad Sci U S A. 1993;90:10759–63.
Koh KP, Wang Y, Yi T, et al. T cell-mediated vascular dysfunction of human allografts results from IFN-gamma dysregulation of NO synthase. J Clin Invest. 2004;114:846–56.
Win TS, Rehakova S, Negus MC, et al. Donor CD4 T cells contribute to cardiac allograft vasculopathy by providing help for autoantibody production. Circ Heart Fail. 2009;2:361–9.
Topilsky Y, Gandhi MJ, Hasin T, et al. Donor-specific antibodies to class II antigens are associated with accelerated cardiac allograft vasculopathy: a three-dimensional volumetric intravascular ultrasound study. Transplantation. 2013;95:389–96.
Tambur AR, Pamboukian SV, Costanzo MR, et al. The presence of HLA-directed antibodies after heart transplantation is associated with poor allograft outcome. Transplantation. 2005;80:1019–25.
Wu GW, Kobashigawa JA, Fishbein MC, et al. Asymptomatic antibody-mediated rejection after heart transplantation predicts poor outcomes. J Heart Lung Transplant. 2009;28:417–22.
Loupy A, Cazes A, Guillemain R, et al. Very late heart transplant rejection is associated with microvascular injury, complement deposition and progression to cardiac allograft vasculopathy. Am J Transplant. 2011;11:1478–87.
Nath DS, Ilias Basha H, Tiriveedhi V, et al. Characterization of immune responses to cardiac self-antigens myosin and vimentin in human cardiac allograft recipients with antibody-mediated rejection and cardiac allograft vasculopathy. J Heart Lung Transplant. 2010;29:1277–85.
Andrade CF, Waddell TK, Keshavjee S, et al. Innate immunity and organ transplantation: the potential role of toll-like receptors. Am J Transplant. 2005;5:969–75.
Graham JA, Wilkinson RA, Hirohashi T, et al. Viral infection induces de novo lesions of coronary allograft vasculopathy through a natural killer cell-dependent pathway. Am J Transplant. 2009;9:2479–84.
Vassalli G, Gallino A, Weis M, et al. Alloimmunity and nonimmunologic risk factors in cardiac allograft vasculopathy. Eur Heart J. 2003;24:1180–8.
Valantine HA. Role of CMV in transplant coronary artery disease and survival after heart transplantation. Transpl Infect Dis. 1999;1 Suppl 1:25–30.
van Dorp WT, van Wieringen PA, Marselis-Jonges E, et al. Cytomegalovirus directly enhances MHC class I and intercellular adhesion molecule-1 expression on cultured proximal tubular epithelial cells. Transplantation. 1993;55:1367–71.
Weis M, Kledal TN, Lin KY, et al. Cytomegalovirus infection impairs the nitric oxide synthase pathway: role of asymmetric dimethylarginine in transplant arteriosclerosis. Circulation. 2004;109:500–5.
Simmonds J, Fenton M, Dewar C, et al. Endothelial dysfunction and cytomegalovirus replication in pediatric heart transplantation. Circulation. 2008;117:2657–61.
Potena L, Grigioni F, Ortolani P, et al. Relevance of cytomegalovirus infection and coronary-artery remodeling in the first year after heart transplantation: a prospective three-dimensional intravascular ultrasound study. Transplantation. 2003;75:839–43.
Pratschke J, Neuhaus P, Tullius SG. What can be learned from brain-death models? Transpl Int. 2005;18:15–21.
Atkinson C, Floerchinger B, Qiao F, et al. Donor brain death exacerbates complement-dependent ischemia/reperfusion injury in transplanted hearts. Circulation. 2013;127:1290–9.
Mehra MR, Uber PA, Ventura HO, et al. The impact of mode of donor brain death on cardiac allograft vasculopathy: an intravascular ultrasound study. J Am Coll Cardiol. 2004;43:806–10.
Perrault LP, Mahlberg F, Breugnot C, et al. Hypercholesterolemia increases coronary endothelial dysfunction, lipid content, and accelerated atherosclerosis after heart transplantation. Arterioscler Thromb Vasc Biol. 2000;20:728–36.
Biadi O, Potena L, Fearon WF, et al. Interplay between systemic inflammation and markers of insulin resistance in cardiovascular prognosis after heart transplantation. J Heart Lung Transplant. 2007;26:324–30.
Zaguri R, Verbovetski I, Atallah M, et al. “Danger” effect of low-density lipoprotein (LDL) and oxidized LDL on human immature dendritic cells. Clin Exp Immunol. 2007;149:543–52.
Khanna AK, Xu J, Uber PA, et al. Tobacco smoke exposure in either the donor or recipient before transplantation accelerates cardiac allograft rejection, vascular inflammation, and graft loss. Circulation. 2009;120:1814–21.
Kobayashi H, Ouchi N, Kihara S, et al. Selective suppression of endothelial cell apoptosis by the high molecular weight form of adiponectin. Circ Res. 2004;94:e27–31.
Ouedraogo R, Gong Y, Berzins B, et al. Adiponectin deficiency increases leukocyte-endothelium interactions via upregulation of endothelial cell adhesion molecules in vivo. J Clin Invest. 2007;117:1718–26.
Okamoto Y, Kihara S, Funahashi T, et al. Adiponectin: a key adipocytokine in metabolic syndrome. Clin Sci (Lond). 2006;110:267–78.
Lara-Castro C, Luo N, Wallace P, et al. Adiponectin multimeric complexes and the metabolic syndrome trait cluster. Diabetes. 2006;55:249–59.
von Eynatten M, Humpert PM, Bluemm A, et al. High-molecular weight adiponectin is independently associated with the extent of coronary artery disease in men. Atherosclerosis. 2008;199:123–8.
Shu KH, Tsai IC, Ho HC, et al. Serum adiponectin levels in renal transplant recipients with and without metabolic syndrome. Transplant Proc. 2012;44:676–9.
Cañas L, Bayés B, Granada ML, et al. Is adiponectin a marker of preclinical atherosclerosis in kidney transplantation? Clin Transplant. 2012;26:259–66.
Roos M, Baumann M, Liu D, et al. Low pre-transplant adiponectin multimers are associated with adverse allograft outcomes in kidney transplant recipients a 3-year prospective study. Regul Pept. 2012;178:11–5.
Okamoto Y, Christen T, Shimizu K, et al. Adiponectin inhibits allograft rejection in murine cardiac transplantation. Transplantation. 2009;88:879–83.
Ishihara T, Haraguchi G, Konishi M, et al. Effect of adiponectin on cardiac allograft vasculopathy. Circ J. 2011;75:2005–12.
Wehner JR, Baldwin III WM. Cardiac allograft vasculopathy: do adipocytes bridge alloimmune and metabolic risk factors? Curr Opin Organ Transplant. 2010;15:639–44.
Minami E, Laflamme MA, Saffitz JE, et al. Extracardiac progenitor cells repopulate most major cell types in the transplanted human heart. Circulation. 2005;112:2951–8.
Simper D, Wang S, Deb A, et al. Endothelial progenitor cells are decreased in blood of cardiac allograft patients with vasculopathy and endothelial cells of noncardiac origin are enriched in transplant atherosclerosis. Circulation. 2003;108:143–9.
Lagaaij EL, Cramer-Knijnenburg GF, van Kemenade FJ, et al. Endothelial cell chimerism after renal transplantation and vascular rejection. Lancet. 2001;357:33–7.
Schober A, Hristov M, Kofler S, et al. CD34 + CD140b + cells and circulating CXCL12 correlate with the angiographically assessed severity of cardiac allograft vasculopathy. Eur Heart J. 2011;32:476–84.
Costanzo MR, Dipchand A, Starling R, et al. International Society of Heart and Lung Transplantation. Guidelines. The International Society of Heart and Lung Transplantation. Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29:914–56. Latest and extensive guidelines covering all aspects of heart transplant care.
Tuzcu EM, Hobbs RE, Rincon G, et al. Occult and frequent transmission of atherosclerotic coronary disease with cardiac transplantation: insights from intravascular ultrasound. Circulation. 1995;91:1706–13.
Johnson DE, Aldermann EL, Schroeder JS, et al. Transplant coronary artery disease: histopathologic correlations with angiographic morphology. J Am Coll Cardiol. 1991;17:449–57.
Lavine KJ, Sintek M, Novak E, et al. Coronary collaterals predict improved survival and allograft function in patients with coronary allograft vasculopathy. Circ Heart Fail. 2013;6:773–84.
Kobashigawa JA, Tobis JM, Starling RC, et al. Multicenter intravascular ultrasound validation study among heart transplant recipients: outcomes after five years. J Am Coll Cardiol. 2005;45:1532–7.
Raichlin E, Bae JH, Kushwaha SS, et al. Inflammatory burden of cardiac allograft coronary atherosclerotic plaque is associated with early recurrent cellular rejection and predicts a higher risk of vasculopathy progression. J Am Coll Cardiol. 2009;53:1279–86.
Tomai F, Adorisio R, De Luca L, et al. Coronary plaque composition assessed by intravascular ultrasound virtual histology: association with long-term clinical outcomes after heart transplantation in young adult recipients. Catheter Cardiovasc Interv. 2013; [In press].
Khandhar SJ, Yamamoto H, Teuteberg JJ, et al. Optical coherence tomography for characterization of cardiac allograft vasculopathy after heart transplantation (OCTCAV study). J Heart Lung Transplant. 2013;32:596–602.
Hirohata A, Nakamura M, Waseda K, et al. Changes in coronary anatomy and physiology after heart transplantation. Am J Cardiol. 2007;99:1603–7.
Hollenberg SM, Klein LW, Parrillo JE, et al. Changes in coronary endothelial function predict progression of allograft vasculopathy after heart transplantation. J Heart Lung Transplant. 2004;23:265–71.
Weis M, Hartmann A, Olbrich HG, et al. Prognostic significance of coronary flow reserve on left ventricular ejection fraction in cardiac transplant recipients. Transplantation. 1998;65:103–8.
Haddad F, Khazanie P, Deuse T, et al. Clinical and functional correlates of early microvascular dysfunction after heart transplantation. Circ Heart Fail. 2012;5:759–68.
Korosoglou G, Riedle N, Erbacher M, et al. Quantitative myocardial blush grade for the detection of cardiac allograft vasculopathy. Am Heart J. 2010;159:643–51.
Derumeaux G, Redonnet M, Mouton-Schleifer D, et al. Dobutamine stress echocardiography in orthotopic heart transplant recipients. J Am Coll Cardiol. 1995;25:1665–72.
Bacal F, Moreira L, Souza G, et al. Dobutamine stress echocardiography predicts cardiac events or death in asymptomatic patients long-term after heart transplantation: 4-year prospective evaluation. J Heart Lung Transplant. 2004;23:1238–44.
Eroglu E, D’hooge J, Sutherland GR, et al. Quantitative dobutamine stress echocardiography for the early detection of cardiac allograft vasculopathy in heart transplant recipients. Heart. 2008;94:e3.
Carlsen J, Toft JC, Mortensen SA, et al. Myocardial perfusion scintigraphy as a screening method for significant coronary artery stenosis in cardiac transplant recipients. J Heart Lung Transplant. 2000;19:873–8.
Ciliberto GR, Ruffini L, Mangiavacchi M, et al. Resting echocardiography and quantitative dipyridamole technetium-99m sestamibi tomography in the identification of cardiac allograft vasculopathy and the prediction of long-term prognosis after heart transplantation. Eur Heart J. 2001;22:964–71.
Gregory SA, Ferencik M, Achenbach S, et al. Comparison of sixty-four-slice multidetector computed tomographic coronary angiography to coronary angiography with intravascular ultrasound for the detection of transplant vasculopathy. Am J Cardiol. 2006;98:877–84.
Steen H, Merten C, Refle S, et al. Prevalence of different gadolinium enhancement patterns in patients after heart transplantation. J Am Coll Cardiol. 2008;52:1160–7.
Muehling OM, Wilke NM, Panse P, et al. Reduced myocardial perfusion reserve and transmural perfusion gradient in heart transplant arteriopathy assessed by magnetic resonance imaging. J Am Coll Cardiol. 2003;42:1054–60.
Labarrere CA, Lee JB, Nelson DR, et al. C-reactive protein, arterial endothelial activation, and development of transplant coronary artery disease: a prospective study. Lancet. 2002;360:1462–7.
Labarrere CA, Nelson DR, Cox CJ, et al. Cardiac-specific troponin I levels and risk of coronary artery disease and graft failure following heart transplantation. JAMA. 2000;284:457–64.
Shaw SM, Williams SG. Is brain natriuretic peptide clinically useful after cardiac transplantation? J Heart Lung Transplant. 2006;25:1396–401.
Mehra MR, Uber PA, Walther D, et al. Gene expression profiles and B-type natriuretic peptide elevation in heart transplantation: more than a hemodynamic marker. Circulation. 2006;114(Suppl I):I-21–26.
Mehra MR, Uber PA, Potluri S, et al. Usefulness of an elevated B-type natriuretic peptide to predict allograft failure, cardiac allograft vasculopathy, and survival after heart transplantation. Am J Cardiol. 2004;94:454–8.
Yamani MH, Taylor DO, Rodriguez ER, et al. Transplant vasculopathy is associated with increased AlloMap gene expression score. J Heart Lung Transplant. 2007;26:403–6.
Singh N, Van Craeyveld E, Tjwa M, et al. Circulating apoptotic endothelial cells and apoptotic endothelial microparticles independently predict the presence of cardiac allograft vasculopathy. J Am Coll Cardiol. 2012;60:324–31.
Lin D, Cohen Freue G, Hollander Z, et al. Plasma protein biosignatures for detection of cardiac allograft vasculopathy. J Heart Lung Transplant. 2013;32:723–33.
Mehra MR, Crespo-Leiro MG, Dipchand A, et al. International Society for Heart and Lung Transplantation. Working formulation of a standardized nomenclature for cardiac allograft vasculopathy-2010. J Heart Lung Transplant. 2010;29:717–27. Explains the rationale behind the proposed nomenclature and its research importance.
Weis M, Pehlivanli S, Meiser BM, et al. Simvastatin treatment is associated with improvement in coronary endothelial function and decreased cytokine activation in patients after heart transplantation. J Am Coll Cardiol. 2001;38:814–8.
Kobashigawa JA, Katznelson S, Laks H, et al. Effect of pravastatin on outcomes after cardiac transplantation. N Engl J Med. 1995;333:621–7.
Kobashigawa JA, Moriguchi JD, Laks H, et al. Ten-year follow-up of a randomized trial of pravastatin in heart transplant patients. J Heart Lung Transplant. 2005;24:1736–40.
Wenke K, Meiser B, Thiery J, et al. Simvastatin initiated early after heart transplantation: 8-year prospective experience. Circulation. 2003;107:93–7.
Steinhauff S, Pehlivanli S, Bakovic-Alt R, et al. Beneficial effects of quinaprilat on coronary vasomotor function, endothelial oxidative stress, and endothelin activation after human heart transplantation. Transplantation. 2004;77:1859–65.
Bae JH, Rihal CS, Edwards BS, et al. Association of angiotensin-converting enzyme inhibitors and serum lipids with plaque regression in cardiac allograft vasculopathy. Transplantation. 2006;82:1108–11.
Schroeder JS, Gao SZ, Alderman EL, et al. A preliminary study of diltiazem in the prevention of coronary artery disease in heart-transplant recipients. N Engl J Med. 1993;328:164–70.
Erinc K, Yamani MH, Starling RC, et al. The effect of combined Angiotensin-converting enzyme inhibition and calcium antagonism on allograft coronary vasculopathy validated by intravascular ultrasound. J Heart Lung Transplant. 2005;24:1033–8.
Fang JC, Kinlay S, Beltrame J, et al. Effect of vitamins C and E on progression of transplant-associated arteriosclerosis: a randomized trial. Lancet. 2002;359:1108–13.
Lim DS, Mooradian SJ, Goldberg CS, et al. Effect of oral L-arginine on oxidant stress, endothelial dysfunction, and systemic arterial pressure in young cardiac transplant recipients. Am J Cardiol. 2004;94:828–31.
Grimm M, Rinaldi M, Yonan NA, et al. Superior prevention of acute rejection by tacrolimus vs cyclosporine in heart transplant recipients: a large European trial. Am J Transplant. 2006;6:1387–97.
Meiser BM, Groetzner J, Kaczmarek I, et al. Tacrolimus or cyclosporine: which is the better partner for mycophenolate mofetil in heart transplant recipients? Transplantation. 2004;78:591–8.
Kobashigawa JA, Patel J, Furukawa H, et al. Five-year results of a randomized, single-center study of tacrolimus vs microemulsion cyclosporine in heart transplant patients. J Heart Lung Transplant. 2006;25:434–9.
Eisen HJ, Kobashigawa J, Keogh A, et al. Three-year results of a randomized, double-blind, controlled trial of mycophenolate mofetil vs azathioprine in cardiac transplant recipients. J Heart Lung Transplant. 2005;24:517–25.
Kaczmarek I, Ertl B, Schmauss D, et al. Preventing cardiac allograft vasculopathy: long-term beneficial effects of mycophenolate mofetil. J Heart Lung Transplant. 2006;25:550–6.
Keogh A, Richardson M, Ruygrok P, et al. Sirolimus in de novo heart transplant recipients reduces acute rejection and prevents coronary artery disease at 2 years: a randomized clinical trial. Circulation. 2004;110:2694–700.
Raichlin E, Bae JH, Khalpey Z, et al. Conversion to sirolimus as primary immunosuppression attenuates the progression of allograft vasculopathy after cardiac transplantation. Circulation. 2007;116:2726–33.
Eisen HJ, Tuzcu EM, Dorent R, et al. Everolimus for the prevention of allograft rejection and vasculopathy in cardiac-transplant recipients. N Engl J Med. 2003;349:847–58.
Hill JA, Hummel M, Starling RC, et al. A lower incidence of cytomegalovirus infection in de novo heart transplant recipients randomized to everolimus. Transplantation. 2007;15(84):1436–42.
Eisen HJ, Kobashigawa J, Starling RC, et al. Everolimus vs mycophenolate mofetil in heart transplantation: a randomized, multi-center trial. Am J Transplant. 2013;13:1203–16. This is a very important clinical study that showed that Everolimus is not associated with improved survival compared with MMF despite decreased vasculopathy progression and at the expense of increased risk of adverse events. It raises the question about the PSI benefit and safety in transplant medicine.
Arora S, Erikstad I, Ueland T, et al. Virtual histology assessment of cardiac allograft vasculopathy following introduction of everolimus–results of a multi-center trial. Am J Transplant. 2012;12:2700–9. Since the Mancini et al. trial [2], the PSI class has been the great hope to slow CAV progression. This study shows possible vasculopathy worsening associated with late PSI introduction.
Matsuo Y, Cassar A, Yoshino S, et al. Attenuation of cardiac allograft vasculopathy by sirolimus: relationship to time interval after heart transplantation. J Heart Lung Transplant. 2013;32:784–91. This an important study because it confirms Arora et al. [99] finding that late PSI introduction may make vasculopathy worse.
Masetti M, Potena L, Nardozza M, et al. Differential effect of everolimus on progression of early and late cardiac allograft vasculopathy in current clinical practice. Am J Transplant. 2013;13:1217–26.
Bader FM, Kfoury AG, Gilbert EM, et al. Percutaneous coronary interventions with stents in cardiac transplant recipients. J Heart Lung Transplant. 2006;25:298–301.
Benza RL, Zoghbi GJ, Tallaj J, et al. Palliation of allograft vasculopathy with transluminal angioplasty: a decade of experience. J Am Coll Cardiol. 2004;43:1973–81.
Lee MS, Kobashigawa J, Tobis J. Comparison of percutaneous coronary intervention with bare-metal and drug-eluting stents for cardiac allograft vasculopathy. JACC Cardiovasc Interv. 2008;1:710–5.
Nfor T, Ansaarie I, Gupta A, et al. Comparing long-term outcomes between drug-eluting and bare-metal stents in the treatment of cardiac allograft vasculopathy. Catheter Cardiovasc Interv. 2009;74:543–9.
Musci M, Loebe M, Wellnhofer E, et al. Coronary angioplasty, bypass surgery, and retransplantation in cardiac transplant patients with graft coronary disease. Thorac Cardiovasc Surg. 1998;46:268–74.
Patel VS, Radovancevic B, Springer W, et al. Revascularization procedures in patients with transplant coronary artery disease. Eur J Cardiothorac Surg. 1997;11:895–901.
Tsai VW, Cooper J, Garan H, et al. The efficacy of implantable cardioverter-defibrillators in heart transplant recipients: results from a multi-center registry. Circ Heart Fail. 2009;2:197–201.
Srivastava R, Keck BM, Bennett LE, et al. The results of cardiac retransplantation: an analysis of the Joint International Society for Heart and Lung Transplantation/United Network for Organ Sharing Thoracic Registry. Transplantation. 2000;70:606–12.
Topkara VK, Dang NC, John R, et al. A decade experience of cardiac retransplantation in adult recipients. J Heart Lung Transplant. 2005;24:1745–50.
Mogollón Jiménez MV, Sobrino Márquez JM, Arizón Muñoz JM, et al. Incidence and importance of de novo diabetes mellitus after heart transplantation. Transplant Proc. 2008;40:3053–5.
Hamblin M, Chang L, Zhang H, et al. Vascular smooth muscle cell peroxisome proliferator-activated receptor-γ mediates pioglitazone-reduced vascular lesion formation. Arterioscler Thromb Vasc Biol. 2011;31:352–9.
Kosuge H, Haraguchi G, Koga N, et al. Pioglitazone prevents acute and chronic cardiac allograft rejection. Circulation. 2006;113:2613–22.
Hermann TS, Dall CH, Christensen SB, et al. Effect of high intensity exercise on peak oxygen uptake and endothelial function in long-term heart transplant recipients. Am J Transplant. 2011;11:536–41.
Nytrøen K, Annette Rustad L, Erikstad I, et al. Effect of high-intensity interval training on progression of cardiac allograft vasculopathy. J Heart Lung Transplant. 2013; [In press].
Kelishadi SS, Azimzadeh AM, Zhang T, et al. Preemptive CD20+ B cell depletion attenuates cardiac allograft vasculopathy in cyclosporine-treated monkeys. J Clin Invest. 2010;120:1275–84.
Heslan JM, Renaudin K, Thebault P, et al. New evidence for a role of allograft accommodation in long-term tolerance. Transplantation. 2006;82:1185–93.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Rodolfo Denadai Benatti declares that he has no conflict of interest.
Dr. David O. Taylor declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Benatti, R.D., Taylor, D.O. Evolving Concepts and Treatment Strategies for Cardiac Allograft Vasculopathy. Curr Treat Options Cardio Med 16, 278 (2014). https://doi.org/10.1007/s11936-013-0278-x
Published:
DOI: https://doi.org/10.1007/s11936-013-0278-x