Abstract
Purpose of Review
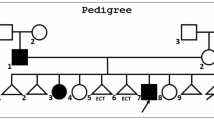
The term osteopetrosis refers to a group of rare skeletal diseases sharing the hallmark of a generalized increase in bone density owing to a defect in bone resorption. Osteopetrosis is clinically and genetically heterogeneous, and a precise molecular classification is relevant for prognosis and treatment. Here, we review recent data on the pathogenesis of this disorder.
Recent Findings
Novel mutations in known genes as well as defects in new genes have been recently reported, further expanding the spectrum of molecular defects leading to osteopetrosis.
Summary
Exploitation of next-generation sequencing tools is ever spreading, facilitating differential diagnosis. Some complex phenotypes in which osteopetrosis is accompanied by additional clinical features have received a molecular classification, also involving new genes. Moreover, novel types of mutations have been recognized, which for their nature or genomic location are at high risk being neglected. Yet, the causative mutation is unknown in some patients, indicating that the genetics of osteopetrosis still deserves intense research efforts.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Sobacchi C, Schulz A, Coxon FP, Villa A, Helfrich MH. Osteopetrosis: genetics, treatment and new insights into osteoclast function. Nat Rev Endocrinol. 2013;9(9):522–36. This review offered a comprehensive overview of the genetics, clinical aspects, cellular pathogenesis and treatment of osteopetrosis.
Sobacchi C, Villa A, Schulz A, Kornak U. CLCN7-Related Osteopetrosis. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Ledbetter N, Mefford HC, Smith RJH, Stephens K, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2017. 2007 Feb 12 [updated 2016 Jun 9].
Döffinger R, Smahi A, Bessia C, Geissmann F, Feinberg J, Durandy A, et al. X-linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappaB signaling. Nat Genet. 2001;27(3):277–85.
Dupuis-Girod S, Corradini N, Hadj-Rabia S, Fournet JC, Faivre L, Le Deist F, et al. Osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia, and immunodeficiency in a boy and incontinentia pigmenti in his mother. Pediatrics. 2002;109(6):e97.
Roberts CM, Angus JE, Leach IH, McDermott EM, Walker DA, Ravenscroft JC. A novel NEMO gene mutation causing osteopetrosis, lymphoedema, hypohidrotic ectodermal dysplasia and immunodeficiency (OL-HED-ID). Eur J Pediatr. 2010;169(11):1403–7.
Carlberg VM, Lofgren SM, Mann JA, Austin JP, Nolt D, Shereck EB, et al. Hypohidrotic ectodermal dysplasia, osteopetrosis, lymphedema, and immunodeficiency in an infant with multiple opportunistic infections. Pediatr Dermatol. 2014;31(6):716–21.
Miot C, Imai K, Imai C, Mancini AJ, Kucuk ZY, Kawai T, et al. Hematopoietic stem cell transplantation in 29 patients hemizygous for hypomorphic IKBKG/NEMO mutations. Blood. 2017;130(12):1456–67.
Sly WS, Whyte MP, Sundaram V, Tashian RE, Hewett-Emmett D, Guibaud P, et al. Carbonic anhydrase II deficiency in 12 families with the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification. N Engl J Med. 1985;313(3):139–45.
Hu PY, Ernst AR, Sly WS, Venta PJ, Skaggs LA, Tashian RE. Carbonic anhydrase II deficiency: single-base deletion in exon 7 is the predominant mutation in Caribbean Hispanic patients. Am J Hum Genet. 1994;54(4):602–8.
Villa A, Guerrini MM, Cassani B, Pangrazio A, Sobacchi C. Infantile malignant, autosomal recessive osteopetrosis: the rich and the poor. Calcif Tissue Int. 2009;84(1):1–12.
Bollerslev J, Henriksen K, Nielsen MF, Brixen K, Van Hul W. Autosomal dominant osteopetrosis revisited: lessons from recent studies. Eur J Endocrinol. 2013;69(2):R39–57.
Qin A, Cheng TS, Pavlos NJ, Lin Z, Dai KR, Zheng MH. V-ATPases in osteoclasts: structure, function and potential inhibitors of bone resorption. Int J Biochem Cell Biol. 2012;44(9):1422–35.
Frattini A, Orchard PJ, Sobacchi C, Giliani S, Abinun M, Mattsson JP, et al. Defects in TCIRG1 subunit of the vacuolar proton pump are responsible for a subset of human autosomal recessive osteopetrosis. Nat Genet. 2000;25(3):343–6.
Sobacchi C, Frattini A, Orchard P, Porras O, Tezcan I, Andolina M, et al. The mutational spectrum of human malignant autosomal recessive osteopetrosis. Hum Mol Genet. 2001;10(17):1767–73.
Pangrazio A, Caldana ME, Lo Iacono N, Mantero S, Vezzoni P, Villa A, et al. Autosomal recessive osteopetrosis: report of 41 novel mutations in the TCIRG1 gene and diagnostic implications. Osteoporos Int. 2012;23(11):2713–8.
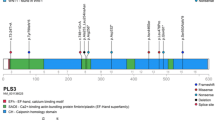
•• Palagano E, Blair HC, Pangrazio A, Tourkova I, Strina D, Angius A, et al. Buried in the middle but guilty: intronic mutations in the TCIRG1 gene cause human autosomal recessive osteopetrosis. J Bone Miner Res. 2015;30(10):1814–21. This manuscript highlighted the possible involvement of deep intronic mutations in disease pathogenesis, with relevant implications for WES data analysis.
Demir K, Nalbantoglu O, Karaer K, Korkmaz HA, Yildiz M, Tunc S, et al. Genetic diagnosis using whole exome analysis in two cases with malignant osteopetrosis of infancy. J Clin Res Pediatr Endocrinol. 2015;7(4):356–7.
Bahr TL, Lund T, Sando NM, Orchard PJ, Miller WP. Haploidentical transplantation with post-transplant cyclophosphamide following reduced-intensity conditioning for osteopetrosis: outcomes in three children. Bone Marrow Transplant. 2016;51:1546–8.
•• Palagano E, Susani L, Menale C, Ramenghi U, Berger M, Uva P, et al. Synonymous mutations add a layer of complexity in the diagnosis of human osteopetrosis. J Bone Miner Res. 2017;32(1):99–105. This manuscript highlighted the possible involvement of synonymous but not silent mutations in disease pathogenesis, with relevant implications for WES data analysis.
Zhang X, He J, Fu W, Wang C, Zhang Z. Novel mutations of TCIRG1 cause a malignant and mild phenotype of autosomal recessive osteopetrosis (ARO) in four Chinese families. Acta Pharmacol Sin 2017.
Leisle L, Ludwig CF, Wagner FA, Jentsch TJ, Stauber T. ClC-7 is a slowly voltage-gated 2Cl(−)/1H(+)-exchanger and requires Ostm1 for transport activity. EMBO J. 2011;30(11):2140–52.
•• Ludwig CF, Ullrich F, Leisle L, Stauber T, Jentsch TJ. Common gating of both CLC transporter subunits underlies voltage-dependent activation of the 2Cl-/1H+ exchanger ClC-7/Ostm1. J Biol Chem. 2013;288(40):28611–9. This and the previous work essentially contributed to the dissection of ClC7/Ostm1 pathophysiology.
Kornak U, Kasper D, Bösl MR, Kaiser E, Schweizer M, Schulz A, et al. Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001;104(2):205–15.
Chen X, Zhang K, Hock J, Wang C, Yu X. Enhanced but hypofunctional osteoclastogenesis in an autosomal dominant osteopetrosis type II case carrying a c.1856C>T mutation in CLCN7. Bone Res. 2016;4:16035.
Deng H, He D, Rong P, Xu H, Yuan L, Li L, et al. Novel CLCN7 mutation identified in a Han Chinese family with autosomal dominant osteopetrosis-2. Mol Pain 2016;12.
González-Rodríguez JD, Luis-Yanes MI, Inglés-Torres E, Arango-Sancho P, Cabrera-Sevilla JE, Duque-Fernández MR, et al. Can acetazolamide be used to treat diseases involving increased bone mineral density? Intractable Rare Dis Res. 2016;5(4):284–9.
Ledemazel J, Plantaz D, Pagnier A, Girard P, Lasfargue M, Hullo E, et al. Malignant infantile osteopetrosis: case report of a 5-month-old boy. Arch Pediatr. 2016;23(4):389–93.
Pang Q, Chi Y, Zhao Z, Xing X, Li M, Wang O, et al. Novel mutations of CLCN7 cause autosomal dominant osteopetrosis type II (ADO-II) and intermediate autosomal recessive osteopetrosis (IARO) in Chinese patients. Osteoporos Int. 2016;27(3):1047–55.
Piret SE, Gorvin CM, Trinh A, Taylor J, Lise S, Taylor JC, et al. Autosomal dominant osteopetrosis associated with renal tubular acidosis is due to a CLCN7 mutation. Am J Med Genet A. 2016;170(11):2988–92.
Zeng B, Li R, Hu Y, Hu B, Zhao Q, Liu H, et al. A novel mutation and a known mutation in the CLCN7 gene associated with relatively stable infantile malignant osteopetrosis in a Chinese patient. Gene. 2016;576(1 Pt 1):176–81.
Zheng H, Shao C, Zheng Y, He JW, Fu WZ, Wang C, et al. Two novel mutations of CLCN7 gene in Chinese families with autosomal dominant osteopetrosis (type II). J Bone Miner Metab. 2016;34(4):440–6.
Okamoto N, Kohmoto T, Naruto T, Masuda K, Komori T, Imoto I. Novel CLCN7 compound heterozygous mutations in intermediate autosomal recessive osteopetrosis. Hum Genome Var. 2017;4:17036.
Worby CA, Dixon JE. Sorting out the cellular functions of sorting nexins. Nat Rev Mol Cell Biol. 2002;3(12):919–31.
Zhou C, Wang Y, Peng J, Li C, Liu P, Shen X. SNX10 plays a critical role in MMP9 secretion via JNK-p38-ERK signaling pathway. J Cell Biochem 2017.
Aker M, Rouvinski A, Hashavia S, Ta-Shma A, Shaag A, Zenvirt S, et al. An SNX10 mutation causes malignant osteopetrosis of infancy. J Med Genet. 2012;49(4):221–6.
Pangrazio A, Fasth A, Sbardellati A, Orchard PJ, Kasow KA, Raza J, et al. SNX10 mutations define a subgroup of human autosomal recessive osteopetrosis with variable clinical severity. J Bone Miner Res. 2013;28(5):1041–9.
•• Stattin EL, Henning P, Klar J, McDermott E, Stecksen-Blicks C, Sandström PE, et al. SNX10 gene mutation leading to osteopetrosis with dysfunctional osteoclasts. Sci Rep. 2017;7(1):3012. This work contributed to unravel the mechanism elicited by SNX10 mutation in the pathogenesis of osteopetrosis.
Amirfiroozy A, Hamidieh AA, Golchehre Z, Rezamand A, Yahyaei M, Beiranvandi F, et al. A novel mutation in SNX10 gene causes malignant infantile Osteopetrosis. Avicenna J Med Biotechnol. 2017;9(4):205–8.
Xu M, Stattin EL, Murphy M, Barry F. Generation of induced pluripotent stem cells (ARO-iPSC1–11) from a patient with autosomal recessive osteopetrosis harboring the c.212+1G>T mutation in SNX10 gene. Stem Cell Res. 2017;24:51–4.
Lange PF, Wartosch L, Jentsch TJ, Fuhrmann JC. ClC-7 requires Ostm1 as a beta-subunit to support bone resorption and lysosomal function. Nature. 2006;440(7081):220–3.
Fischer T, De Vries L, Meerloo T, Farquhar MG. Promotion of Gαi3 subunit down-regulation by GIPN, a putative E3 ubiquitin ligase that interacts with RGS-GAIP. Proc Natl Acad Sci. 2003;100:8270–5.
Feigin ME, Malbon CC. OSTM1 regulates beta-catenin/Lef1 interaction and is required for Wnt/beta-catenin signaling. Cell Signal. 2008;20(5):949–57.
Pandruvada SN, Beauregard J, Benjannet S, Pata M, Lazure C, Seidah NG, et al. Role of Ostm1 cytosolic complex with kinesin 5B in intracellular dispersion and trafficking. Mol Cell Biol. 2015;36(3):507–21.
Chalhoub N, Benachenhou N, Rajapurohitam V, Pata M, Ferron M, Frattini A, et al. Grey-lethal mutation induces severe malignant autosomal recessive osteopetrosis in mouse and human. Nat Med. 2003;9(4):399–406.
Pangrazio A, Poliani PL, Megarbane A, Lefranc G, Lanino E, Di Rocco M, et al. Mutations in OSTM1 (grey lethal) define a particularly severe form of autosomal recessive osteopetrosis with neural involvement. J Bone Miner Res. 2006;21(7):1098–105.
• Shin B, Yu J, Park ES, Choi S, Yu J, Hwang JM, et al. Secretion of a truncated osteopetrosis-associated transmembrane protein 1 (OSTM1) mutant inhibits osteoclastogenesis through down-regulation of the B lymphocyte-induced maturation protein 1 (BLIMP1)-nuclear factor of activated T cells c1 (NFATc1) axis. J Biol Chem. 2014;289(52):35868–81. This work described a possible mechanism elicited by OSTM1 truncated protein products in the pathogenesis of osteopetrosis.
Ott CE, Fischer B, Schröter P, Richter R, Gupta N, Verma N, et al. Severe neuronopathic autosomal recessive osteopetrosis due to homozygous deletions affecting OSTM1. Bone. 2013;55(2):292–7.
Herebian D, Alhaddad B, Seibt A, Schwarzmayr T, Danhauser K, Klee D, et al. Coexisting variants in OSTM1 and MANEAL cause a complex neurodegenerative disorder with NBIA-like brain abnormalities. Eur J Hum Genet. 2017;25(9):1092–5.
Fujiwara T, Ye S, Castro-Gomes T, Winchell CG, Andrews NW, Voth DE, et al. PLEKHM1/DEF8/RAB7 complex regulates lysosome positioning and bone homeostasis. JCI Insight. 2016;1(17):e86330.
Marwaha R, Arya SB, Jagga D, Kaur H, Tuli A, Sharma M. The Rab7 effector PLEKHM1 binds Arl8b to promote cargo traffic to lysosomes. J Cell Biol. 2017;216(4):1051–70.
McEwan DG, Popovic D, Gubas A, Terawaki S, Suzuki H, Stadel D, et al. PLEKHM1 regulates autophagosome-lysosome fusion through HOPS complex and LC3/GABARAP proteins. Mol Cell. 2015;57(1):39–54.
Witwicka H, Jia H, Kutikov A, Reyes-Gutierrez P, Li X, Odgren PR. TRAFD1 (FLN29) interacts with Plekhm1 and regulates osteoclast acidification and resorption. PLoS One. 2015;10(5):e0127537.
Van Wesenbeeck L, Odgren PR, Coxon FP, Frattini A, Moens P, Perdu B, et al. Involvement of PLEKHM1 in osteoclastic vesicular transport and osteopetrosis in incisors absent rats and humans. J Clin Invest. 2007;117(4):919–30.
Del Fattore A, Fornari R, Van Wesenbeeck L, de Freitas F, Timmermans JP, Peruzzi B, et al. A new heterozygous mutation (R714C) of the osteopetrosis gene, pleckstrin homolog domain containing family M (with run domain) member 1 (PLEKHM1), impairs vesicular acidification and increases TRACP secretion in osteoclasts. J Bone Miner Res. 2008;23(3):380–91.
Bo T, Yan F, Guo J, Lin X, Zhang H, Guan Q, et al. Characterization of a relatively malignant form of osteopetrosis caused by a novel mutation in the PLEKHM1 gene. J Bone Miner Res. 2016;31(11):1979–87.
Tolar J, Teitelbaum SL, Orchard PJ. Osteopetrosis. N Engl J Med. 2004;351:2839–49.
Shah GN, Bonapace G, Hu PY, Strisciuglio P, Sly WS. Carbonic anhydrase II deficiency syndrome (osteopetrosis with renal tubular acidosis and brain calcification): novel mutations in CA2 identified by direct sequencing expand the opportunity for genotype-phenotype correlation. Hum Mutat. 2004;24(3):272.
Alhuzaim ON, Almohareb OM. Sherbeeni SM carbonic anhydrase II deficiency in a Saudi woman. Clin Med Insights Case Rep. 2015;8:7–10.
Pang Q, Qi X, Jiang Y, Wang O, Li M, Xing X, et al. Two novel CAII mutations causing carbonic anhydrase II deficiency syndrome in two unrelated Chinese families. Metab Brain Dis. 2015;30(4):989–97.
Alsharidi A, Al-Hamed M, Alsuwaida A. Carbonic anhydrase II deficiency: report of a novel mutation. CEN Case Rep. 2016;5:108–12.
Rognoni E, Ruppert R, Fässler R. The kindlin family: functions, signaling properties and implications for human disease. J Cell Sci. 2016;129(1):17–27.
Schmidt S, Nakchbandi I, Ruppert R, Kawelke N, Hess MW, Pfaller K, et al. Kindlin-3-mediated signaling from multiple integrin classes is required for osteoclast-mediated bone resorption. J Cell Biol. 2011;192(5):883–97.
Crazzolara R, Maurer K, Schulze H, Zieger B, Zustin J, Schulz AS. A new mutation in the KINDLIN-3 gene ablates integrin-dependent leukocyte, platelet, and osteoclast function in a patient with leukocyte adhesion deficiency-III. Pediatr Blood Cancer. 2015;62(9):1677–9.
Palagano E, Slatter MA, Uva P, Menale C, Villa A, Abinun M, et al. Hematopoietic stem cell transplantation corrects osteopetrosis in a child carrying a novel homozygous mutation in the FERMT3 gene. Bone. 2017;97:126–9.
Liu W, Zhang X. Receptor activator of nuclear factor-κB ligand (RANKL)/RANK/osteoprotegerin system in bone and other tissues (review). Mol Med Rep. 2015;11(5):3212–8.
•• Luo J, Yang Z, Ma Y, Yue Z, Lin H, Qu G, et al. LGR4 is a receptor for RANKL and negatively regulates osteoclast differentiation and bone resorption. Nat Med. 2016;22(5):539–46. This work identified LGR4 as an additional receptor for the essential osteoclastogenic cytokine RANKL; the implications of these data in bone pathophysiology still have to be completely understood.
• Schena F, Menale C, Caci E, Diomede L, Palagano E, Recordati C, et al. Murine Rankl-/- Mesenchymal Stromal Cells display an osteogenic differentiation defect improved by a RANKL-expressing lentiviral vector. Stem Cells. 2017;35(5):1365–77. This work first described a defect in the osteoblast lineage due to RANKL absence; the implications of these data in bone pathophysiology still have to be clarified and might extend well beyond RANKL-deficient ARO.
Sobacchi C, Frattini A, Guerrini MM, Abinun M, Pangrazio A, Susani L, et al. Osteoclast-poor human osteopetrosis due to mutations in the gene encoding RANKL. Nat Genet. 2007;39(8):960–2.
• Lo Iacono N, Pangrazio A, Abinun M, Bredius R, Zecca M, Blair HC, et al. RANKL cytokine: from pioneer of the osteoimmunology era to cure for a rare disease. Clin Dev Immunol. 2013;2013:412768. This work described RANKL-deficient ARO patients; to the best of our knowledge, this remains the only subgroup of ARO in which the bone defect is not corrected by HSCT.
Guerrini MM, Sobacchi C, Cassani B, Abinun M, Kilic SS, Pangrazio A, et al. Human osteoclast-poor osteopetrosis with hypogammaglobulinemia due to TNFRSF11A (RANK) mutations. Am J Hum Genet. 2008 Jul;83(1):64–76.
• Pangrazio A, Cassani B, Guerrini MM, Crockett JC, Marrella V, Zammataro L, et al. RANK-dependent autosomal recessive osteopetrosis: characterization of five new cases with novel mutations. J Bone Miner Res. 2012;27(2):342–51. This work described RANK-deficient ARO patients and clearly highlighted the differences with the RANKL-dependent subgroup of osteoclast-poor ARO patients.
Porta F, Cavagnini S, Imberti L, Sottini A, Bolda F, Beghin A, et al. Partial depletion of TCR alpha/beta+/CD19+ cells in matched unrelated transplantation of three patients with osteopetrosis. Bone Marrow Transplant. 2015;50(12):1583–5.
Natsheh J, Drozdinsky G, Simanovsky N, Lamdan R, Erlich O, Gorelik N, et al. Improved outcomes of hematopoietic stem cell transplantation in patients with infantile malignant osteopetrosis using fludarabine-based conditioning. Pediatr Blood Cancer. 2016;63(3):535–40.
Simanovsky N, Rozovsky K, Hiller N, Weintraub M, Stepensky P. Extending the spectrum of radiological findings in patients with severe osteopetrosis and different genetic backgrounds. Pediatr Blood Cancer. 2016;63(7):1222–6.
Shamriz O, Shaag A, Yaacov B, NaserEddin A, Weintraub M, Elpeleg O, et al. The use of whole exome sequencing for the diagnosis of autosomal recessive malignant infantile osteopetrosis. Clin Genet. 2017;92(1):80–5.
Campeau PM, Lu JT, Sule G, Jiang MM, Bae Y, Madan S, et al. Whole-exome sequencing identifies mutations in the nucleoside transporter gene SLC29A3 in dysosteosclerosis, a form of osteopetrosis. Hum Mol Genet. 2012;21(22):4904–9.
Turan S, Mumm S, Gottesman GS, Abali S, Baş S, Atay Z, et al. Dysosteosclerosis from a unique mutation in SLC29A3. Presented at the 7th International Conference on Children’s Bone Health 2015, Salzburg, Austria. Bone Abstracts 4:97.
Gelb BD, Shi GP, Chapman HA, Desnick RJ. Pycnodysostosis, a lysosomal disease caused by cathepsin K deficiency. Science. 1996;273(5279):1236–8.
Novinec M, Lenarčič B. Cathepsin K: a unique collagenolytic cysteine peptidase. Biol Chem. 2013;394(9):1163–79.
Christensen J, Shastri VP. Matrix-metalloproteinase-9 is cleaved and activated by cathepsin K. BMC Res Notes. 2015;8:322.
Bonnet N, Brun J, Rousseau JC, Duong LT, Ferrari SL. Cathepsin K controls cortical bone formation by degrading periostin. J Bone Miner Res. 2017;32(7):1432–41.
Xue Y, Cai T, Shi S, Wang W, Zhang Y, Mao T, et al. Clinical and animal research findings in pycnodysostosis and gene mutations of cathepsin K from 1996 to 2011. Orphanet J Rare Dis. 2011;6:20.
Xue Y, Wang L, Xia D, Li Q, Gao S, Dong M, et al. Dental abnormalities caused by novel compound heterozygous CTSK mutations. J Dent Res. 2015;94(5):674–81.
Singh A, Cuevas-Covarrubias S, Pradhan G, Gautam VK, Messina-Baas O, Gonzalez-Huerta LM, et al. Novel mutation and white matter involvement in an Indian child with pycnodysostosis. Indian J Pediatr. 2015;82(5):471–3.
Huang X, Qi X, Li M, Wang O, Jiang Y, Xing X, et al. A mutation in CTSK gene in an autosomal recessive pycnodysostosis family of Chinese origin. Calcif Tissue Int. 2015;96(5):373–8.
Araujo TF, Ribeiro EM, Arruda AP, Moreno CA, de Medeiros PF, Minillo RM, et al. Molecular analysis of the CTSK gene in a cohort of 33 Brazilian families with pycnodysostosis from a cluster in a Brazilian northeast region. Eur J Med Res. 2016;21(1):33.
Mandal K, Ray S, Saxena D, Srivastava P, Moirangthem A, Ranganath P, et al. Pycnodysostosis: mutation spectrum in five unrelated Indian children. Clin Dysmorphol. 2016;25(3):113–20.
Rovira Martí P, Ullot FR. Orthopaedic disorders of pycnodysostosis: a report of five clinical cases. Int Orthop. 2016;40(11):2221–31.
Song HK, Sohn YB, Choi YJ, Chung YS, Jang JH. A case report of pycnodysostosis with atypical femur fracture diagnosed by next-generation sequencing of candidate genes. Medicine (Baltimore). 2017;96(12):e6367.
Lomaga MA, Yeh WC, Sarosi I, Duncan GS, Furlonger C, Ho A, et al. TRAF6 deficiency results in osteopetrosis and defective interleukin-1, CD40, and LPS signaling. Genes Dev. 1999;13(8):1015–24.
• Weisz Hubshman M, Basel-Vanagaite L, Krauss A, Konen O, Levy Y, Garty BZ, et al. Homozygous deletion of RAG1, RAG2 and 5′ region TRAF6 causes severe immune suppression and atypical osteopetrosis. Clin Genet. 2017;91(6):902–7. This work suggested a role for TRAF6 in the pathogenesis of human osteopetrosis.
• Iida A, Xing W, Docx MFK, Nakashima T, Wang Z, Kimizuka M, et al. Identification of biallelic LRRK1 mutations in osteosclerotic metaphyseal dysplasia and evidence for locus heterogeneity. J Med Genet. 2016;53:568–74. This work suggested a possible pathogenetic role of LRRK1 recessive mutations in a peculiar form of osteopetrosis.
Xing WR, Goodluck H, Zeng C, Mohan S. Role and mechanism of action of leucine-rich repeat kinase 1 in bone. Bone Res. 2017;5:17003.
Lu SY, Li M, Lin YL. Mitf regulates osteoclastogenesis by modulating NFATc1 activity. Exp Cell Res. 2014;328(1):32–43.
Steingrímsson E, Moore KJ, Lamoreux ML, Ferré-D'Amaré AR, Burley SK, Zimring DC, et al. Molecular basis of mouse microphthalmia (mi) mutations helps explain their developmental and phenotypic consequences. Nat Genet. 1994;8(3):256–63.
• George A, Zand DJ, Hufnagel RB, Sharma R, Sergeev YV, Legare JM, et al. Biallelic mutations in MITF cause coloboma, osteopetrosis, microphthalmia, macrocephaly, albinism, and deafness. Am J Hum Genet. 2016;99(6):1388–94. This work suggested a possible pathogenetic role of MITF recessive mutations in a peculiar form of osteopetrosis.
• Frederiksen AL, Larsen MJ, Brusgaard K, Novack DV, Thii Knudsen PJ, Daa Schroder H, et al. Neonatal high bone mass with first mutation of the NF-kB complex: heterozygous de novo missense (p.Asp512Ser) RELA (Rela/p65). J Bone Miner Res. 2016;31(1):163–72. This work suggested a possible pathogenetic role of a RELA mutation in a form of neonatal High Bone Mass.
Dai XM, Ryan GR, Hapel AJ, Dominguez MG, Russell RG, Kapp S, et al. Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood. 2002;99(1):111–20.
• Monies D, Maddirevula S, Kurdi W, Alanazy MH, Alkhalidi H, Al-Owain M, et al. Autozygosity reveals recessive mutations and novel mechanisms in dominant genes: implications in variant interpretation. Genet Med. 2017. This work suggested a possible pathogenetic role of CSF1R mutations in two ARO patients.
Migliaccio S, Luciani M, Taranta A, De Rossi G, Minisola S, El Hachem M, et al. Association of intermediate osteopetrosis with poikiloderma. J Bone Miner Res. 1999;14(5):834–6.
Mroczek S, Krwawicz J, Kutner J, Lazniewski M, Kuciński I, Ginalski K, et al. C16orf57, a gene mutated in poikiloderma with neutropenia, encodes a putative phosphodiesterase responsible for the U6 snRNA 3′ end modification. Genes Dev. 2012;26(17):1911–25.
• Colombo EA, Bazan JF, Negri G, Gervasini C, Elcioglu NH, Yucelten D, et al. Novel C16orf57 mutations in patients with Poikiloderma with Neutropenia: bioinformatic analysis of the protein and predicted effects of all reported mutations. Orphanet J Rare Dis. 2012;7:7. This work identified C16orf57 as the gene mutated in a patient displaying osteopetrosis, poikiloderma and neutropenia.
Colombo EA, Carra S, Fontana L, Bresciani E, Cotelli F, Larizza L. A zebrafish model of Poikiloderma with neutropenia recapitulates the human syndrome hallmarks and traces back neutropenia to the myeloid progenitor. Sci Rep. 2015;5:15814.
Patil P, Uechi T, Kenmochi N. Incomplete splicing of neutrophil-specific genes affects neutrophil development in a zebrafish model of poikiloderma with neutropenia. RNA Biol. 2015;12(4):426–34.
Schulz AS, Moshous D, Steward CG, Villa A, Sobacchi C. Osteopetrosis–Consensus Guidelines of the ESID and the EBMT Working Party Inborn Errors [online], https://esid.org/layout/set/print/content/view/full/14267.
Orchard PJ, Fasth AL, Le Rademacher J, He W, Boelens JJ, Horwitz EM, et al. Hematopoietic stem cell transplantation for infantile osteopetrosis. Blood. 2015;126(2):270–6.
Chiesa R, Ruggeri A, Paviglianiti A, Zecca M, Gónzalez-Vicent M, Bordon V, et al. Outcomes after unrelated umbilical cord blood transplantation for children with Osteopetrosis. Biol Blood Marrow Transpl. 2016;22(11):1997–2002.
Wu CC, Econs MJ, DiMeglio LA, Insogna KL, Levine MA, Orchard PJ, et al. Diagnosis and management of osteopetrosis: consensus guidelines from the Osteopetrosis Working Group. J Clin Endocrinol Metab. 2017;102(9):3111–23.
Jamuar SS, Tan EC. Clinical application of next-generation sequencing for Mendelian diseases. Hum Genomics. 2015;9:10.
Frebourg T. The challenge for the next generation of medical geneticists. Hum Mutat. 2014;35(8):909–11.
Acknowledgements
We acknowledge the many authors whose original contribution in the field could not be cited in this minireview for the sake of brevity.
Funding
This work was partially supported by the European Community’s Seventh Framework Program (FP7/2007–2013, SYBIL Project), by PRIN Projects (20102M7T8X_003 and 2015F3JHMB_004) to AV and by Programma Nazionale per la Ricerca-Consiglio Nazionale delle Ricerche Aging Project to AV, and by Ministero della Salute - Giovani Ricercatori (grant GR-2011-02348266) to CS.
Author information
Authors and Affiliations
Contributions
All the authors contributed to organize, draft, and revise the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Eleonora Palagano, Cristina Sobacchi, Anna Villa, and Ciro Menale declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetics
Rights and permissions
About this article
Cite this article
Palagano, E., Menale, C., Sobacchi, C. et al. Genetics of Osteopetrosis. Curr Osteoporos Rep 16, 13–25 (2018). https://doi.org/10.1007/s11914-018-0415-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-018-0415-2