Abstract
Purpose of Review
We review emerging evidence regarding the impact of gut microbes on antitumor immunity, and ongoing efforts to translate this in clinical trials.
Recent Findings
Pre-clinical models and human cohort studies support a role for gut microbes in modulating overall immunity and immunotherapy response, and numerous trials are now underway exploring strategies to modulate gut microbes to enhance responses to cancer therapy. This includes the use of fecal microbiota transplant (FMT), which is being used to treat patients with Clostridium difficile infection among other non-cancer indications. The use of FMT is now being extended to modulate gut microbes in patients being treated with cancer immunotherapy, with the goal of enhancing responses and/or to ameliorate toxicity. However, significant complexities exist with such an approach and will be discussed herein.
Summary
Data from ongoing studies of FMT in cancer will provide critical insights for optimization of this approach.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. American Association for the Advancement of Science; 2018 [cited 2020 Feb 17];359:1350–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29567705.
Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease. Nature. 2016 [cited 2020 Jan 8];535:75–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27383982.
Carding S, Verbeke K, Vipond DT, Corfe BM, Owen LJ. Dysbiosis of the gut microbiota in disease. Microb Ecol Heal Dis Co-Action Publishing. 2015;26.
Garrett WS. Cancer and the microbiota. Science. 2015. p. 80–6.
Pushalkar S, Hundeyin M, Daley D, Zambirinis CP, Kurz E, Mishra A, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018 [cited 2019 Nov 26];8:403–16. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29567829.
Schwabe RF, Jobin C. The microbiome and cancer. Nat Rev Cancer. 2013 [cited 2020 Feb 17];13:800–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24132111.
Jenq RR, Taur Y, Devlin SM, Ponce DM, Goldberg JD, Ahr KF, et al. Intestinal blautia is associated with reduced death from graft-versus-host disease. Biol Blood Marrow Transplant. Elsevier Inc. 2015;21:1373–83.
Shono Y, Docampo MD, Peled JU, Perobelli SM, Velardi E, Tsai JJ, et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci Transl Med. 2016 [cited 2020 Jan 8];8:339ra71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27194729.
• Taur Y, Jenq RR, Perales MA, Littmann ER, Morjaria S, Ling L, et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. American Society of Hematology; 2014;124:1174–82. This paper was the first to demonstrate a potential role of the gut microbiome in cancer outcomes in a human cohort.
Viaud S, Saccheri F, Mignot G, Yamazaki T, Daillère R, Hannani D, et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science (80- ). 2013;342:971–6.
•• Vétizou M, Pitt JM, Daillère R, Lepage P, Waldschmitt N, Flament C, et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015 [cited 2020 Jan 8];350:1079–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26541610. These papers were the first.
•• Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science (80- ). American Association for the Advancement of Science; 2015;350:1084–9. These papers were the first.
•• Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets T V, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018 [cited 2019 Sep 17];359:97–103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29097493. These papers were the first.
•• Matson V, Fessler J, Bao R, Chongsuwat T, Zha Y, Alegre ML, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science (80- ). American Association for the Advancement of Science; 2018;359:104–8. These papers were the first.
•• Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science (80- ). American Association for the Advancement of Science; 2018;359:91–7. These papers were the first.
Chaput N, Lepage P, Coutzac C, Soularue E, Le Roux K, Monot C, et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann Oncol Off J Eur Soc Med Oncol. 2017 [cited 2020 Jan 8];28:1368–79. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28368458.
Frankel AE, Coughlin LA, Kim J, Froehlich TW, Xie Y, Frenkel EP, et al. Metagenomic shotgun sequencing and unbiased metabolomic profiling identify specific human gut microbiota and metabolites associated with immune checkpoint therapy efficacy in melanoma patients. Neoplasia (US). Neoplasia Press, Inc. 2017;19:848–55.
McQuade JL, Daniel CR, Helmink BA, Wargo JA. Modulating the microbiome to improve therapeutic response in cancer. Lancet Oncol. Lancet Publishing Group; 2019. p. e77–91.
Van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, De Vos WM, et al. Duodenal infusion of donor feces for recurrent clostridium difficile. N Engl J Med Massachussetts Medical Society. 2013;368:407–15.
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. Oxford University Press. 2018:e1–48.
Faecal microbiota transplant for recurrent Clostridium difficile infection | Guidance | NICE [Internet]. NICE; [cited 2019 Oct 17]. Available from: https://www.nice.org.uk/guidance/ipg485
Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell. 2018 [cited 2020 Jan 8];174:1388-1405.e21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30193112.
Abt MC, McKenney PT, Pamer EG. Clostridium difficile colitis: pathogenesis and host defence. Nat Rev Microbiol. Nature Publishing Group; 2016 [cited 2020 Feb 17];14:609–20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27573580.
Lewis BB, Buffie CG, Carter RA, Leiner I, Toussaint NC, Miller LC, et al. Loss of microbiota-mediated colonization resistance to Clostridium difficile infection with oral vancomycin compared with metronidazole. J Infect Dis. Oxford University Press; 2015 [cited 2020 Feb 17];212:1656–65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25920320.
Grehan MJ, Borody TJ, Leis SM, Campbell J, Mitchell H, Wettstein A. Durable alteration of the colonic microbiota by the administration of donor fecal flora. J Clin Gastroenterol. 2010 [cited 2020 Feb 17];44:551–61. Available from: https://insights.ovid.com/crossref?an=00004836-201009000-00013.
Kao D, Roach B, Silva M, Beck P, Rioux K, Kaplan GG, et al. Effect of oral capsule– vs colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: a randomized clinical trial. JAMA. American Medical Association. 2017;318:1985–93.
Ooijevaar RE, Terveer EM, Verspaget HW, Kuijper EJ, Keller JJ. Clinical application and potential of fecal microbiota transplantation. Annu Rev Med. Annual Reviews; 2019 [cited 2020 Feb 17];70:335–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30403550.
Yalchin M, Segal JP, Mullish BH, Quraishi MN, Iqbal TH, Marchesi JR, et al. Gaps in knowledge and future directions for the use of faecal microbiota transplant in the treatment of inflammatory bowel disease. Therap Adv Gastroenterol. SAGE Publications Ltd; 2019 [cited 2020 Feb 17];12:1756284819891038. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31803254.
Shanahan F, Quigley EMM. Manipulation of the microbiota for treatment of IBS and IBD—challenges and controversies. Gastroenterology WB Saunders. 2014;146:1554–63.
Paramsothy S, Kamm MA, Kaakoush NO, Walsh AJ, van den Bogaerde J, Samuel D, et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet Lancet Publishing Group. 2017;389:1218–28.
Siegmund B. Is intensity the solution for FMT in ulcerative colitis? Lancet (London, England). Lancet Publishing Group; 2017 [cited 2020 Feb 17];389:1170–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28214090.
Wilson BC, Vatanen T, Cutfield WS, O’Sullivan JM. The super-donor phenomenon in fecal microbiota transplantation. Front Cell Infect Microbiol. 2019 [cited 2019 Oct 8];9:2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30719428.
Kump P, Wurm P, Gröchenig HP, Wenzl H, Petritsch W, Halwachs B, et al. The taxonomic composition of the donor intestinal microbiota is a major factor influencing the efficacy of faecal microbiota transplantation in therapy refractory ulcerative colitis. Aliment Pharmacol Ther. Blackwell Publishing Ltd; 2018 [cited 2020 Feb 17];47:67–77. Available from: http://doi.wiley.com/10.1111/apt.14387
Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology. W.B. Saunders. 2015;149:102–109.e6.
Vermeire S, Joossens M, Verbeke K, Wang J, Machiels K, Sabino J, et al. Donor species richness determines faecal microbiota transplantation success in inflammatory bowel disease. J Crohns Colitis. Oxford University Press; 2016 [cited 2020 Feb 17];10:387–94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26519463.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JFWM, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. W.B. Saunders. 2012;143.
Kootte RS, Levin E, Salojärvi J, Smits LP, Hartstra AV, Udayappan SD, et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab. Cell Press. 2017;26:611–619.e6.
DeFilipp Z, Bloom PP, Torres Soto M, Mansour MK, Sater MRA, Huntley MH, et al. Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med. 2019 [cited 2019 Nov 19];NEJMoa1910437. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1910437
Cammarota G, Ianiro G, Tilg H, Rajilić-Stojanović M, Kump P, Satokari R, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017 [cited 2019 Oct 8];66:569–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28087657.
Important safety alert regarding use of fecal microbiota for transplantation and risk of serious adverse reactions due to transmission of multi-drug resistant organisms | FDA. [cited 2019 Nov 19]. Available from: https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse.
Huang X-Z, Gao P, Song Y-X, Xu Y, Sun J-X, Chen X-W, et al. Antibiotic use and the efficacy of immune checkpoint inhibitors in cancer patients: a pooled analysis of 2740 cancer patients. Oncoimmunology. 2019 [cited 2020 Jan 8];8:e1665973. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31741763.
Freitag TL, Hartikainen A, Jouhten H, Sahl C, Meri S, Anttila V-J, et al. Minor effect of antibiotic pre-treatment on the engraftment of donor microbiota in fecal transplantation in mice. Front Microbiol. 2019;10:2685.
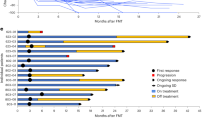
Baruch E, Youngester Y OR. Fecal microbiota transplantation (FMT) and re-induction of anti-PD-1 therapy in refractory metastatic melanoma patients—preliminary results from a phase I clinical trial (NCT 03353402) AACR Annual Meeting. Atlanta, Georgia; 2019.
Maleki S, Lenehan J BJ. Combination of fecal microbiota transplantation from healthy donors with anti-PD1 immunotherapy in treatment-naïve advanced or metastatic melanoma patients. National Harbor, MD; 2019.
Wang Y, Wiesnoski DH, Helmink BA, Gopalakrishnan V, Choi K, DuPont HL, et al. Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nat Med Nature Publishing Group. 2018;24:1804–8.
Geller LT, Barzily-Rokni M, Danino T, Jonas OH, Shental N, Nejman D, et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science (80- ). American Association for the Advancement of Science. 2017;357:1156–60.
Riquelme E, Zhang Y, Zhang L, Montiel M, Zoltan M, Dong W, et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell. Cell Press. 2019;178:795–806.e12.
Ma C, Han M, Heinrich B, Fu Q, Zhang Q, Sandhu M, et al. Gut microbiome–mediated bile acid metabolism regulates liver cancer via NKT cells. Science (80- ). American Association for the Advancement of Science. 2018:360.
Philips CA, Pande A, Shasthry SM, Jamwal KD, Khillan V, Chandel SS, et al. Healthy donor fecal microbiota transplantation in steroid-ineligible severe alcoholic hepatitis: a pilot study. Clin Gastroenterol Hepatol. 2017 [cited 2019 Nov 26];15:600–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27816755.
Bajaj JS, Kassam Z, Fagan A, Gavis EA, Liu E, Cox IJ, et al. Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: a randomized clinical trial. Hepatology. John Wiley and Sons Inc. 2017;66:1727–38.
Ren Y-D, Ye Z-S, Yang L-Z, Jin L-X, Wei W-J, Deng Y-Y, et al. Fecal microbiota transplantation induces hepatitis B virus e-antigen (HBeAg) clearance in patients with positive HBeAg after long-term antiviral therapy. Hepatology. 2017 [cited 2019 Nov 26];65:1765–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28027582.
Helmink B, Gopalakrishnan V, Khan A et al. Variation of the gut microbiome of complete responders to immune checkpoint blockade and healthy individuals—implications for clinical trial design. SITC. 2018; National H:115.
Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature Nature Publishing Group. 2018;555:623–8.
Cho I, Blaser MJ. The human microbiome: AT the interface of health and disease. Nat Rev Genet. 2012:260–70.
McDonald D, Hyde E, Debelius JW, Morton JT, Gonzalez A, Ackermann G, et al. American gut: an open platform for citizen science microbiome research. mSystems. American Society for Microbiology; 2018;3.
Thompson S, Guetterman H, Taylor A, Bogner A, Martin D, Farrell JJ, et al. Dietary predictors of fecal microbiota transplantation success. J Acad Nutr Diet. Elsevier BV. 2016;116:A76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jennifer L. McQuade has received compensation from Bristol-Myers Squibb and Merck for service as a consultant.
Gabriel O. Ologun receives funding from the National Institutes of Health (NIH) grant T32 CA 09599 and the M.D. Anderson Cancer Center support grant P30 CA016672.
Reetakshi Arora declares that she has no conflict of interest.
Jennifer A. Wargo receives research funding through grants from the American Association for Cancer Research Stand Up To Cancer, the NIH, and the Melanoma Research Alliance; has received clinical trial support from Bristol-Myers Squibb, GlaxoSmithKline, Roche/Genentech, and Novartis; has received speaker’s honoraria from Bristol-Myers Squibb, Illumina, Imedex, Omniprex, Gilead, PeerView, Physician Education Resource, Medimmune, and Exelixis; has received compensation for service as a consultant/clinical scientific advisor from Bristol-Myers Squibb, Microbiome DX, Biothera Pharma, Merck, and Dhome; has received compensation for participation on advisory boards from GlaxoSmithKline, Roche/Genentech, Novartis, and AstraZeneca; and has a patent application pending submitted by the University of Texas M.D. Anderson Cancer Center that covers methods to enhance immune checkpoint blockade responses by modulating the microbiome.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Melanoma
Rights and permissions
About this article
Cite this article
McQuade, J.L., Ologun, G.O., Arora, R. et al. Gut Microbiome Modulation Via Fecal Microbiota Transplant to Augment Immunotherapy in Patients with Melanoma or Other Cancers. Curr Oncol Rep 22, 74 (2020). https://doi.org/10.1007/s11912-020-00913-y
Published:
DOI: https://doi.org/10.1007/s11912-020-00913-y