Abstract
Purpose of Review
We aim to systematically review the literature on the effectiveness of pediatric antimicrobial stewardship programs (ASPs) and antimicrobial stewardship (AS) strategies in the United States (US) inpatient setting. Furthermore, we review current gaps and challenges for unique pediatric populations and those in ambulatory settings.
Recent Findings
Misuse and overuse of antimicrobials have been identified as key factors for antimicrobial resistance (AR). Multiple professional organizations support the implementation of hospital-based ASPs to decrease antimicrobial consumption, improve patient outcomes, and reduce healthcare costs. There is limited data on the effectiveness of inpatient pediatric ASPs and AS strategies in unique populations. Furthermore, there is a paucity of evidence on ASPs in ambulatory settings.
Summary
This review contributes to the growing body of evidence that supports the use of pediatric ASPs to optimize antimicrobial therapy in the inpatient setting as well as in unique patient populations and ambulatory settings. Active stewardship is critical and antimicrobial consumption is a key outcome metric for programs.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, Pediatric Infectious Diseases Society. Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol. 2012;33(4):322–327.
Antimicrobial resistance: global report on surveillance 2014 [Internet]. World Health Organization [cited 2018 April 10]. Available from: http://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf?sequence=1
• Logan LK, Gandra S, Mandal S, Klein EY, Levinson J, Weinstein RA, et al. Multidrug- and carbapenem-resistant Pseudomonas aeruginosa in children, United States, 1999–2012. J Pediatric Infect Dis Soc 2016 Nov 16. These authors highlight the increasing rate of multidrug-resistant Pseudomonas aeruginosa isolates in US children between 1999 and 2012.
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007 Jan 15;44(2):159–77.
•• Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–77. This article provides evidence-based guidelines and expert guidance from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America on antimicrobial stewardship program approaches for optimization of antimicrobial use in the inpatient setting.
Gerber JS, Newland JG, Coffin SE, Hall M, Thurm C, Prasad PA, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010 Dec;126(6):1067–73.
Pakyz AL, MacDougall C, Oinonen M, Polk RE. Trends in antibacterial use in US academic health centers: 2002 to 2006. Arch Intern Med. 2008 Nov 10;168(20):2254–60.
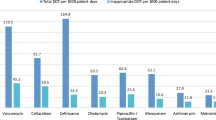
Gerber JS, Kronman MP, Ross RK, Hersh AL, Newland JG, Metjian TA, et al. Identifying targets for antimicrobial stewardship in children’s hospitals. Infect Control Hosp Epidemiol. 2013 Dec;34(12):1252–8.
Antibiotic prescribing and use in hospitals and long-term care [Internet]. Atlanta (GA): Centers for Disease Control and Prevention. 2017 [cited 2017 Jan 8]. Available from: http://www.cdc.gov/getsmart/healthcare/.
Newland JG, Gerber JS, Weissman SJ, Shah SS, Turgeon C, Hedican EB, et al. Prevalence and characteristics of antimicrobial stewardship programs at freestanding children’s hospitals in the United States. Infect Control Hosp Epidemiol. 2014 Mar;35(3):265–71.
• Hersh AL, De Lurgio SA, Thurm C, Lee BR, Weissman SJ, Courter JD, et al. Antimicrobial stewardship programs in freestanding children's hospitals. Pediatrics. 2015;135(1):33–9. This is a multicenter study across freestanding children’s hospitals. Authors observed an overall decrease in antimicrobial use in DOT per 1000 PD across freestanding children’s hospitals with or without ASP. The rate of decline was highest in those with a formalized ASP. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption
• Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core elements of outpatient antibiotic stewardship. MMWR Recomm Rep. 2016;65(6):1–12. These authors provide guidance for antimicrobial stewardship in the outpatient setting based on existing evidence-based guidelines and expert opinion from other clinical settings.
• Smith MJ, Gerber JS, Hersh AL. Inpatient antimicrobial stewardship in pediatrics: a systematic review. J Pediatric Infect Dis Soc. 2015;4(4):e127–35. This is a systematic review of studies published through March 2014 that evaluated the effectiveness of inpatient pediatric ASPs and other supplemental AS interventions. These data suggest that pediatric ASPs can be effective at decreasing antimicrobial consumption without short-term adverse events.
• Turner RB, Valcarlos E, Loeffler AM, Gilbert M, Chan D. Impact of an Antimicrobial Stewardship Program on Antibiotic Use at a Nonfreestanding Children's Hospital. J Pediatric Infect Dis Soc. 2017;6(3):e36–40. This is a single-center study in a non-freestanding children’s hospital that reported on the impact of PAF on antimicrobial consumption. Authors found an overall reduction of antimicrobial use and vancomycin use in DOT per 1000 PD without a difference in hospital LOS or in-hospital mortality. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption without affecting patient safety
• Lighter-Fisher J, Desai S, Stachel A, Pham VP, Klejmont L, Dubrovskaya Y. Implementing an inpatient pediatric prospective audit and feedback antimicrobial stewardship program within a larger medical center. Hosp Pediatr. 2017;7(9):516–22. This is a single-center study in a non-freestanding children’s hospital. Authors implemented a formal ASP with CPG, PAF, and restriction and found an overall reduction in antimicrobial use in DOT per 1000 PD. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Hurst AL, Child J, Pearce K, Palmer C, Todd JK, Parker SK. Handshake stewardship: a highly effective rounding-based antimicrobial optimization service. Pediatr Infect Dis J. 2016;35(10):1104–10. This is a single-center study in a freestanding children’s hospital. Authors implemented a “handshake stewardship” program defined by lack of restriction and preauthorization, review of all prescribed antimicrobials, and rounding-based feedback by a pharmacist-physician team. This approach reduced hospital-wide antimicrobial consumption and reduced meropenem and vancomycin use as well. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Willis ZI, Gillon J, Xu M, Slaughter JC, Di Pentima MC. Reducing antimicrobial use in an academic pediatric institution: evaluation of the effectiveness of a prospective audit with real-time feedback. J Pediatric Infect Dis Soc. 2017;6(4):339–45. This is a single-center center that implemented an ASP primarily focused on PAF, but that also included elements of prior authorization and CPG development, which led to an overall reduction of antimicrobial DOT per 1000 PD. Using a comparator group, authors concluded that the ASPs impact was greater than would have been expected based on secular trends.
• Gillon J, Xu M, Slaughter J, Di Pentima MC. Vancomycin use: room for improvement among hospitalized children. J Pharm Pract. 2017;30(3):296–9. This is a single-center center that implemented an ASP primarily focused on PAF which led to a reduction in vancomycin DOT per 1000 PD. Using a comparator group, authors concluded that vancomycin use was lower compared to hospitals without an ASP. This study adds to the growing body of evidence that suggests pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Chan S, Hossain J, Di Pentima MC. Implications and impact of prior authorization policy on vancomycin use at a tertiary pediatric teaching hospital. Pediatr Infect Dis J. 2015;34(5):506–8. This is a single-center center that implemented an ASP primarily focused on PAF which led to a reduction in vancomycin DOT per 1000 PD. This study adds to the growing body of evidence that suggests pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Nguyen-Ha PT, Howrie D, Crowley K, Vetterly CG, McGhee W, Berry D, et al. A quality assessment of a collaborative model of a pediatric antimicrobial stewardship program. Pediatrics 2016;137(5):https://doi.org/10.1542/peds.2015-0316. Epub 2016 Apr 6. This is a single-center center that implemented an ASP focused on PAF, restriction, and CPGs and found a reduction in vancomycin and meropenem DOT per 1000 PD. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Molloy L, McGrath E, Thomas R, Kaye KS, Rybak MJ. Acceptance of pharmacist-driven antimicrobial stewardship recommendations with differing levels of physician involvement in a children’s hospital. Clin Pediatr (Phila). 2017;56(8):744–51. This is a single-center center that implemented a pharmacist-driven ASP and found no difference in hospital LOS, in-hospital mortality, or all-cause readmission after implementation. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be effective at decreasing antimicrobial consumption.
• Ross RK, Beus JM, Metjian TA, Localio AR, Shelov ED, Desai BR, et al. Safety of automatic end dates for antimicrobial orders to facilitate stewardship. Infect Control Hosp Epidemiol. 2016;37(8):974–8. This is a single-center center that implemented an ASP focused on restriction with an automated EMR stop order and found no difference in hospital LOS, in-hospital mortality, or readmission rates during the study period. This study adds to the growing body of evidence that suggests inpatient pediatric ASPs can be implemented without affecting patient safety.
• Rutman L, Wright DR, O'Callaghan J, Spencer S, Lion KC, Kronman MP, et al. A comprehensive approach to pediatric pneumonia: relationship between standardization, antimicrobial stewardship, clinical testing, and cost. J Healthc Qual. 2017;39(4):e59–69. This is a single-center center that implemented a CAP CPG at an institution without a formal ASP, which led to increased consumption of a more narrow empiric antimicrobial agent. This study adds to the growing body of evidence that suggests pediatric AS interventions can be effective at decreasing antimicrobial consumption.
• Lee KR, Bagga B, Arnold SR. Reduction of broad-spectrum antimicrobial use in a tertiary children’s hospital post antimicrobial stewardship program guideline implementation. Pediatr Crit Care Med. 2016;17(3):187–93. This is a single-center center that implemented multiple CPGS for patients in their institution’s pediatric, NICU, and cardiac ICU. Authors found a reduction in overall and targeted antimicrobial consumption across studied units.
Hurst AL, Olson D, Somme S, Child J, Pyle L, Ranade D, et al. Once-daily ceftriaxone plus metronidazole versus ertapenem and/or cefoxitin for pediatric appendicitis. J Pediatric Infect Dis Soc. 2017 Mar 1;6(1):57–64.
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR. Reported medication use in the neonatal intensive care unit: data from a large national data set. Pediatrics. 2006 Jun;117(6):1979–87.
Cantey JB, Wozniak PS, Sanchez PJ. Prospective surveillance of antibiotic use in the neonatal intensive care unit: results from the SCOUT study. Pediatr Infect Dis J. 2015 Mar;34(3):267–72.
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK Jr, et al. The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics. 2006 Aug;118(2):717–22.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sanchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009 Jan;123(1):58–66.
Tsai MH, Chu SM, Hsu JF, Lien R, Huang HR, Chiang MC, et al. Risk factors and outcomes for multidrug-resistant Gram-negative bacteremia in the NICU. Pediatrics. 2014 Feb;133(2):e322–9.
Patel SJ, Saiman L. Principles and strategies of antimicrobial stewardship in the neonatal intensive care unit. Semin Perinatol. 2012 Dec;36(6):431–6.
iNICQ 2017: choosing antibiotics wisely [Internet]. Vermont Oxford Network; 2018. [cited 2018 Jan 8]. Available from: http://public.vtoxford.org/quality-education/inicq-2017-choosing-antibiotics-wisely/.
Schulman J, Dimand RJ, Lee HC, Duenas GV, Bennett MV, Gould JB. Neonatal intensive care unit antibiotic use. Pediatrics. 2015 May;135(5):826–33.
Cantey JB, Patel SJ. Antimicrobial stewardship in the NICU. Infect Dis Clin N Am. 2014 Jun;28(2):247–61.
• Nzegwu NI, Rychalsky MR, Nallu LA, Song X, Deng Y, Natusch AM, et al. Implementation of an antimicrobial stewardship program in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2017;38(10):1137–43. This is a single-center study that created a formal NICU ASP using PF and CPGs, which was led by a multidisciplinary team. Authors found a reduction in ampicillin DOT per 1000 PD. This study adds to the growing body of evidence that suggests ASPs in NICU can be effective at decreasing antimicrobial consumption.
• Cantey JB, Wozniak PS, Pruszynski JE, Sanchez PJ. Reducing unnecessary antibiotic use in the neonatal intensive care unit (SCOUT): a prospective interrupted time-series study. Lancet Infect Dis. 2016;16(10):1178–84. This is a single-center study that implemented AS interventions targeting areas of high proportion antimicrobial use at their institution. After implementation, authors found a reduction of overall antimicrobial utilization without any short-term adverse outcomes. This study adds to the growing body of evidence that suggests AS interventions in NICU can be effective at decreasing antimicrobial consumption without affecting patient safety.
Holzmann-Pazgal G, Khan AM, Northrup TF, Domonoske C, Eichenwald EC. Decreasing vancomycin utilization in a neonatal intensive care unit. Am J Infect Control. 2015 Nov;43(11):1255–7.
Chiu CH, Michelow IC, Cronin J, Ringer SA, Ferris TG, Puopolo KM. Effectiveness of a guideline to reduce vancomycin use in the neonatal intensive care unit. Pediatr Infect Dis J. 2011 Apr;30(4):273–8.
• Goldman JL, Ross RK, Lee BR, Newland JG, Hersh AL, Kronman MP, et al. Variability in antifungal and antiviral use in hospitalized children. Infect Control Hosp Epidemiol. 2017;38(6):743–6. Authors found significant variability in antifungal and antiviral therapy prescribing in high-risk children among freestanding children’s hospitals. This study highlights the importance of an inpatient ASP targeting these agents.
Wolf J, Sun Y, Tang L, Newland JG, Gerber JS, Van Dyke CJ, et al. Antimicrobial stewardship barriers and goals in pediatric oncology and bone marrow transplantation: a survey of antimicrobial stewardship practitioners. Infect Control Hosp Epidemiol. 2016 Mar;37(3):343–7.
Wattier RL, Levy ER, Sabnis AJ, Dvorak CC, Auerbach AD. Reducing second gram-negative antibiotic therapy on pediatric oncology and hematopoietic stem cell transplantation services. Infect Control Hosp Epidemiol. 2017 Sep;38(9):1039–47.
Chai G, Governale L, McMahon AW, Trinidad JP, Staffa J, Murphy D. Trends of outpatient prescription drug utilization in US children, 2002–2010. Pediatrics. 2012 Jul;130(1):23–31.
Saleh EA, Schroeder DR, Hanson AC, Banerjee R. Guideline-concordant antibiotic prescribing for pediatric outpatients with otitis media, community-acquired pneumonia, and skin and soft tissue infections in a large multispecialty healthcare system. Clin Res Infect Dis 2015;2(1).
Gerber JS, Prasad PA, Russell Localio A, Fiks AG, Grundmeier RW, Bell LM, et al. Variation in antibiotic prescribing across a pediatric primary care network. J Pediatric Infect Dis Soc. 2015 Dec;4(4):297–304.
Hersh AL, Jackson MA, Hicks LA, American Academy of Pediatrics Committee on Infectious Diseases. Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics. 2013;132(6):1146–54.
Kronman MP, Zhou C, Mangione-Smith R. Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics. 2014 Oct;134(4):e956–65.
Bradley JS, Byington CL, Shah SS, Azlverson B, Carter ER, Harrison C, et al. Executive summary: the management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011 Oct;53(7):617–30.
• Handy LK, Bryan M, Gerber JS, Zaoutis T, Feemster KA. Variability in antibiotic prescribing for community-acquired pneumonia. Pediatrics. 2017;139(4):https://doi.org/10.1542/peds.2016-2331. Epub 2017 Mar 7. Authors found significant variability in antimicrobial prescribing for CAP across multiple, pediatric outpatient practices independent of microbiologic etiology. This article highlights the need for AS intervention or a formalized ASP in the outpatient setting to optimize antimicrobial prescribing for this patient population.
Gerber JS, Prasad PA, Fiks AG, Localio AR, Grundmeier RW, Bell LM, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: a randomized trial. JAMA. 2013 Jun 12;309(22):2345–52.
Szymczak JE, Feemster KA, Zaoutis TE, Gerber JS. Pediatrician perceptions of an outpatient antimicrobial stewardship intervention. Infect Control Hosp Epidemiol. 2014 Oct;35(Suppl 3):S69–78.
Gerber JS, Prasad PA, Fiks AG, Localio AR, Bell LM, Keren R, et al. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA. 2014 Dec 17;312(23):2569–70.
May L, Cosgrove S, L'Archeveque M, Talan DA, Payne P, Jordan J, et al. A call to action for antimicrobial stewardship in the emergency department: approaches and strategies. Ann Emerg Med 2013 Jul;62(1):69–77.e2.
Watson JR, Sanchez PJ, Spencer JD, Cohen DM, Hains DS. Urinary tract infection and antimicrobial stewardship in the emergency department. Pediatr Emerg Care. 2016.
• Mistry RD, Newland JG, Gerber JS, Hersh AL, May L, Perman SM, et al. Current state of antimicrobial stewardship in children’s hospital emergency departments. Infect Control Hosp Epidemiol. 2017;38(4):469–75. This multicenter study highlights current AS activities reported in emergency departments in children’s hospitals participating in the Sharing Antimicrobial Resistance Practices (SHARPs) collaboration. This is an important descriptive study addressing current AS practices in this ambulatory setting.
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014 Aug;42(8):1749–55.
Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010 Apr;38(4):1045–53.
•• Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77. This is an important article highlighting the consensus statements of the surviving sepsis guideline panel on the best care for patients with sepsis using evidence-based recommendations.
Sepsis Bundle Project (SEP) Specifications Manual for National Hospital Inpatient Quality Measures Discharges [Internet]. Centers for Medicare and Medicaid Services [cited 2018 March 3]. Available from: http://www.Nhfca.org/psf/resources/updates/SEP-1%20measure%20information%20form%20(MIF).pdf.
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe Sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med. 2015 Sep;43(9):1907–15.
Minderhoud TC, Spruyt C, Huisman S, Oskam E, Schuit SCE, Levin MD. Microbiological outcomes and antibiotic overuse in emergency department patients with suspected sepsis. Neth J Med. 2017 Jun;75(5):196–203.
Banerjee R, Beekmann SE, Doby EH, Polgreen PM, Rathore MH, Hersh AL. Outpatient parenteral antimicrobial therapy practices among pediatric infectious diseases consultants: results of an emerging infections network survey. J Pediatric Infect Dis Soc. 2014 Mar;3(1):85–8.
Barrier A, Williams DJ, Connelly M, Creech CB. Frequency of peripherally inserted central catheter complications in children. Pediatr Infect Dis J. 2012 May;31(5):519–21.
Knackstedt ED, Stockmann C, Davis CR, Thorell EA, Pavia AT, Hersh AL. Outpatient parenteral antimicrobial therapy in pediatrics: an opportunity to expand antimicrobial stewardship. Infect Control Hosp Epidemiol. 2015 Feb;36(2):222–4.
• Goldman JL, Richardson T, Newland JG, Lee B, Gerber JS, Hall M, et al. Outpatient parenteral antimicrobial therapy in pediatric Medicaid enrollees. J Pediatric Infect Dis Soc. 2017;6(1):65–71. Authors studied outpatient parenteral antibiotic therapy (OPAT) in a large population of US children enrolled in Medicaid and found a high rate of adverse events coupled with administration of systemic agents that are highly bioavailable that could be given orally. OPAT may be a suitable target for an outpatient-based ASP.
• Hersh AL, Olson J, Stockmann C, Thorell EA, Knackstedt ED, Esquibel L, et al. Impact of antimicrobial stewardship for pediatric outpatient parenteral antibiotic therapy. J Pediatric Infect Dis Soc 2017. This is a single-center study where authors incorporated outpatient parenteral antibiotic therapy into their established ASP. This study demonstrates that traditional ASPs can be extended and incorporated in the outpatient setting.
•• Moehring RW, Anderson DJ, Cochran RL, Hicks LA, Srinivasan A, Dodds Ashley ES, et al. Expert consensus on metrics to assess the impact of patient-level antimicrobial stewardship interventions in acute-care settings. Clin Infect Dis. 2017;64(3):377–83. This article provides expert consensus on appropriate metrics to assess ASP interventions in inpatient settings.
• Gerber JS, Hersh AL, Kronman MP, Newland JG, Ross RK, Metjian TA. Development and application of an antibiotic spectrum index for benchmarking antibiotic selection patterns across hospitals. Infect Control Hosp Epidemiol. 2017;38(8):993–7. Authors created an antibiotic spectrum index to measure and compare the broad spectrum of antimicrobial use across US children’s hospitals. This metric, based on spectrum of activity against clinically relevant pathogens, provides a new opportunity to assess ASPs along with the standard metric of DOT per 1000 PD. This metric may be helpful in evaluating the effectiveness of ASP at decreasing the utilization of broad-spectrum antimicrobials.
Pollack LA, Srinivasan A. Core elements of hospital antibiotic stewardship programs from the Centers for Disease Control and Prevention. Clin Infect Dis. 2014;59(Suppl 3):S97–100.
•• Joint Commission on Hospital Accreditation. APPROVED: new antimicrobial stewardship standard. Jt Comm Perspect. 2016;36(7):1, 3–4, 8. This statement from the Joint Commission requires that all hospitals implement an ASP based on current scientific literature, which was effective on January 1, 2017.
Centers for Medicare and Medicaid Services. CMS issues proposed rule that prohibits discrimination, reduces hospital-acquired conditions, and promotes antibiotic stewardship in hospitals [Internet]. 2016 June [cited 2018 March 3]. Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-06-13.html
Wagner B, Filice GA, Drekonja D, Greer N, MacDonald R, Rutks I, et al. Antimicrobial stewardship programs in inpatient hospital settings: a systematic review. Infect Control Hosp Epidemiol. 2014 Oct;35(10):1209–28.
Federal Register: The Daily Journal of the United States Government. Medicare and Medicaid programs; reform of requirements for long-term-care facilities [Internet]. 2016 September [cited 2018 Jan 8]. Available from: https://www.federalregister.gov/documents/2016/10/04/2016-23503/medicare-and-medicaid-programs-reform-of-requirements-for-long-term-care-facilities
• Feldstein D, Sloane PD, Feltner C. Antibiotic stewardship programs in nursing homes: a systematic review. J Am Med Dir Assoc 2017. This is a systematic review of studies published on the effectiveness of ASPs in nursing homes. Authors concluded that ASPs in this unique patient population can reduce antimicrobial prescriptions and improve provider adherence to proposed AS guidelines. This study adds to the growing body of evidence that ASPs can be effectively used in unique patient populations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
About this article
Cite this article
Godbout, E.J., Pakyz, A.L., Markley, J.D. et al. Pediatric Antimicrobial Stewardship: State of the Art. Curr Infect Dis Rep 20, 39 (2018). https://doi.org/10.1007/s11908-018-0644-7
Published:
DOI: https://doi.org/10.1007/s11908-018-0644-7