Abstract
Purpose of Review
To outline intervention efforts focused on reducing hypertension disparities in immigrant communities in the U.S. and to identify areas in the design, implementation, and evaluation of these interventions that warrant further exploration guided by an implementation science framework.
Recent Findings
Studies examined (n = 11) included immigrant populations of African, Hispanic, and Asian origin. Men were underrepresented in most studies. Culturally tailored group-based educational sessions in religious or community spaces were common. Intervention agents included research assistants, registered nurses, community health workers, and faith-based organization volunteers. Community stakeholders were engaged in most studies, although most commonly for recruitment efforts. Surveys/interviews were used for intervention evaluation, and documentation of intervention activities and trainings was used to assess fidelity.
Summary
Identified pathways for further intervention innovation included gender or migration-status–based targeting, diversifying intervention agents, enhancing mixed-method process evaluations, and tailoring to emerging needs during the COVID-19 pandemic.
Similar content being viewed by others
Introduction
Hypertension affects more than 108 million adults in the United States (U.S.) and is considered a major risk factor for various non-communicable diseases and a significant contributor to morbidity and mortality in the country, including among immigrants [1•, 2,3,4]. In recent years, immigrants have been a significant driver of population growth in the U.S. [5]; however, there are also significant socio-economic disparities both between and within immigrant groups of certain national origins [6]. Likewise, representation of diverse immigrants in the U.S. across research intervention efforts has been limited [7]. Importantly, certain immigrant communities have higher prevalence of hypertension, including undocumented immigrants [8], and immigrants originating from South, Southeast, Central and East Asia, Russia and/or Eastern Europe, the Dominican Republic, and the Caribbean [1, 9,10,11]. Higher levels of acculturation [12•], including increased length of time in the U.S. [10], has similarly been associated with greater prevalence of hypertension among immigrants, although this association has not been consistent in all immigrant communities [13]. These mixed findings may be attributed to the fact that prevalence of chronic conditions in immigrants in the U.S. is likely reflective of disease burden in sending countries and point to the importance of considering such conditions rather than applying a uniform “healthy immigrant effect” assumption.
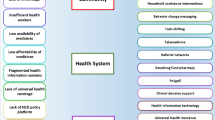
In understanding these hypertension disparities among U.S. immigrants, it is important to identify and intervene on factors related to hypertension incidence, progression, and management faced by these communities. Access to healthcare remains a major obstacle across immigrant communities [14, 15]. Factors attributed to these barriers in healthcare access include interconnected structural and individual-level barriers, including ineligibility for certain healthcare programs [16], limited in-language support for culturally appropriate healthcare services [17], lack of knowledge of the healthcare system [18], distrust of the U.S. healthcare system [19] and, particularly among undocumented immigrants, fears related to deportation due to policies linking documentation status with use of public services [15, 20]. Access-related issues often intersect with other barriers to healthcare utilization and health behaviors among immigrants, including specific customs or unique cultural or religious understandings of health and disease [19, 21]. These various influences also underpin hypertension outcomes among immigrants; U.S. immigrants are more likely to be unaware of their hypertension [22], have undiagnosed or uncontrolled hypertension [23], and display lower treatment rates of hypertension, particularly among those without a usual source of care or health insurance [3].
Given the distinct factors driving hypertension disparities among immigrants in the U.S., intervention and programmatic efforts to address this burden must meet the unique needs of these diverse communities. Modifiable lifestyle behavioral risk factors of hypertension (including diet, physical activity, and stress) have been the common targets of hypertension reduction interventions [24, 25]. However, intervention research must consider many of the upstream and cultural factors driving hypertension in immigrant communities, including certain gender roles [26], perceptions about physical activity [26], demanding work schedules [27], neighborhood environment barriers to healthy living [27], and limited physical and financial accessibility to appropriate spaces for healthy activities [28]. To appropriately design, implement, and evaluate lifestyle behavior interventions in immigrant settings, community-engaged approaches [29,30,31], health behavior theories [32, 33], and implementation science frameworks [34] that contextualize behaviors and advocate for engaging with communities throughout different stages of the intervention are necessary.
Given the common lifestyle–related drivers of non-communicable diseases (NCDs), many lifestyle intervention studies among U.S. immigrant populations focused on other NCDs such as obesity [30] and diabetes [31]. These studies have assessed reductions in blood pressure as one part of a broader set of study outcomes; however, given that disparities in hypertension may not directly align with those of other NCDs in immigrant populations [1•] and the unique role that specific lifestyle behaviors (e.g., dietary salt intake) have in hypertension incidence [25], the need for tailored hypertension interventions in immigrant settings has become apparent. Likewise, aligning with community-based participatory research (CBPR) principles, it is vital to examine how the current and changing drivers of hypertension in immigrant communities can be addressed through innovative intervention strategies, particularly given the significant social, economic, and health disruptions that have occurred globally since the COVID-19 pandemic in 2020. These concerns are particularly heightened given the connection between hypertension and severe illness or mortality resulting from COVID-19 [35, 36].
Therefore, the aim of this narrative review is to summarize recent developments in hypertension intervention research among U.S. immigrant population to identify (1) key areas of recent innovation in the design, implementation, and evaluation of hypertension interventions to meet the unique needs of this community and (2) identify areas that warrant further exploration to enhance intervention research that meets current and future needs of the rapidly growing immigrant population in the U.S.
Methods
Scope and Definitions
Based on the aims of this review, articles included in final analysis were any intervention studies with a primary aim of reducing hypertension through individual behavior change in a study population that was either majority or exclusively composed of immigrants living in the U.S. The scope thus included intervention studies aimed at modifiable behavioral risk factors of hypertension (e.g., diet, exercise, alcohol consumption, or tobacco consumption) in which blood pressure control or reduction was an explicit study aim.
Search Strategy
A search was conducted on PubMed, Google Scholar, and Scopus for peer-reviewed studies and gray-literature published in English between 1 January 2017 and 1 November 2020. A search strategy was developed with combinations of keywords related to the three dimensions of the study aims: immigrants in the U.S. (e.g., migrant, immigrant, minorities, United States, American), hypertension (e.g., blood pressure, hypertension, diastolic, systolic), and interventions (e.g., program, trial, intervention, pre-post, quasi-experimental). The database search was supplemented by employing snowballing methodology to identify further studies by using reference lists of studies and past reviews identified in the database search. Titles and abstracts of studies identified through the search strategy were then screened; reviews and most observational studies were excluded, as well as studies focusing on non-U.S. populations. Observational studies that described the characteristics or processes of an intervention, or other themes relevant to program implementation were included. Full-text reviews were conducted on studies that passed preliminary screening; intervention studies involving a U.S.-based sample population that was majority immigrant in which change in blood pressure as an explicit primary or secondary goal of the study were included. Information from relevant observational studies was also extracted to provide supplemental analysis on intervention implementation and characteristics.
Synthesis of Literature
The information identified from included studies was informed by principles of the Consolidated Framework for Implementation Research (CFIR), developed by Damschroder et al. to guide the systematic assessment of interventions and identify different factors influencing intervention design, implementation, and evaluation [34]. These factors include (1) characteristics of individuals (e.g., sample size, sex/age, country of origins, migration, and socio-economic status), (2) intervention characteristics (e.g., setting, recruitment, components, development, and adaptations), (3) inner setting (e.g., types of program staff, training), (4) outer setting (e.g., community collaborations), and (5) process (e.g., planning process and formative research, evaluation procedures, and intervention fidelity). Additional information relevant to the characteristics, barriers, and facilitators of the included interventions was also reviewed and compiled.
Results
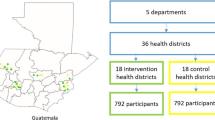
Overall, 11 studies representing 10 distinct hypertension interventions were identified (Table 1). Populations of focus included immigrants of African [37••, 38], Filipino [39••, 40], Hispanic or Latino (unspecified nationalities) [41, 42••, 43], Chinese [44], South Asian [45••, 46], and multiple Asian [47••] descents. Most studies (n = 6) did not involve a control group and employed a pre-post-quasi experimental study design [37, 38, 42••, 43, 44, 47], including one stepped-wedge quasi-experimental intervention [45••, 46] and two randomized controlled trials [39••, 41]. Diverse regions of the U.S. with large populations of immigrants were represented, including California [37••, 44], Texas [38, 42••], Pennsylvania [39••], South Carolina [41], Florida [43], and New York [40, 45••, 46, 47••]. One protocol for a hypertension intervention in immigrant adults during the COVID-19 pandemic was also identified [37••].
With respect to characteristics of individuals, most studies had a majority female study sample (n = 8) with an average age of above 40 years (n = 6). Although migration or citizenship status of participants was rarely reported, three studies which reported length of time in the U.S. had an average of 10 years or longer [39••, 40, 44]. Common intervention settings including religious (n = 4) and community spaces (n = 5), using word-of-mouth or event-based venues for recruitment. Other common intervention characteristics included group educational sessions focused on hypertension-related lifestyle behaviors (notably diet and exercise) and the cultural adaptation of evidence-based curricula developed in largely non-immigrant communities; intervention length varied significantly from a 30-min intervention [37••] to one spanning 5 years [45••]. Program staff who delivered the interventions included registered nurses, students, community-health workers (CHWs), health department consultants, and certified fitness instructors. Most of these intervention agents received training on program logistics, responsibilities, and use of technology. Outer setting engagement, informed by principles of CBPR, was also common; community-based organization (CBO), faith-based organization (FBO), and other community stakeholders largely engaged in either recruitment or some aspects of the intervention development (n = 6), although some interventions directly involved community leaders in intervention implementation [38, 39••]. With respect to the CFIR process construct, fidelity assessments were identified in multiple interventions and conducted through training checklists, participant tracking cards, and participant-CHW interaction evaluations. Intervention evaluations largely occurred at the end of interventions and included mixed-method process evaluations (e.g., semi-structured interviews or clinical and participant survey data).
Discussion
Based on the key findings observed across research interventional studies, a number of key suggestions for future programmatic efforts (including those related to new considerations regarding the COVID-19 pandemic) are summarized in Table 2.
Innovating to Meet the Unique and Diverse Hypertension-Related Needs of Immigrants
The unique and constantly changing social-, cultural-, economic-, and health-related needs of immigrants in the U.S. requires that researchers innovate to enhance the efficacy and sustainability of health programs [7, 26,27,28]. Among recent efforts, much of this innovation has centered around cultural adaptations of existing health promotion curricula, involving community members in various ways to tailor intervention experiences, or adapting interventions to the unique context of the lives of immigrants in the U.S. For example, many immigrants in the U.S. face long working hours, poor job security, limited vacation or sick days, and other significant economic and job-related restrictions, many of which have directly been cited as reasons which limited their participation in hypertension interventions [7, 48]. With these constraints in mind, exploring shorter interventions aimed at intensively providing these communities with the knowledge and resource capacity in a self-sufficient manner to meet their hypertension needs has been considered a strategy. Erskine et al. explored this through their 30-min brief hypertension educational session among African immigrants in which they evaluated change in hypertension knowledge both pre- and post-session as well as after a 30-day follow-up [38]. Although statistically significant increases in hypertension knowledge were only observed post-session, further research is warranted to assess whether such short, intensive formats of interventions can be designed in a way to foster more sustainable improvements in hypertension related outcomes [38].
Disaggregation of race and ethnicity data across immigrant study populations may also help to better tailor hypertension interventions. While tailoring interventions to immigrants of certain national origins or self-identified ethnicities was common, acknowledging and integrating the intersectional influences of gender and migration status in the context of the immigrant experience of hypertension could be further explored. While none of the studies included in this review focused on exclusively men or women (although most had a majority female study population), a number of gender-based disparities have been observed in health behaviors, healthcare utilization, and various other social and economic factors relevant to lifestyle contributors of hypertension among immigrants [26, 49]. Indeed, one study found that women were more likely to complete follow-up assessment than men, and gender-based disparities in hypertension outcome trends was observed in some [43] but not all [42••] studies. Targeted interventions for both men and women in immigrant communities respectively may be warranted, a strategy commonly employed in diabetes prevention interventions among U.S. immigrant communities [50]. Similarly, outside of length of time in the U.S. or foreign-born status, specific migration status indictors (notably citizenship status) were not examined in any of the included studies. While it is likely that such information is not collected or reported due to participant hesitancy in disclosing immigration status, migration-related indicators have a direct influence on both an individual’s actual capacity as well as perceived trust to engage with many aspects of the healthcare system [15, 51]. Thus, considering the hypertension disparities faced by communities such as undocumented immigrants [15], hypertension interventions that consider additional dimensions of gender or immigration status in how an intervention is designed, implemented, and evaluated have the potential to reduce health disparities. Moreover, interventions should aim to be cost-neutral for these communities (particularly undocumented immigrants) and should not require additional financial resources given the community’s already existent financial strains and high out-of-pocket expenses.
Finally, while a range of intervention agents (e.g., CHWs, registered nurses, FBO volunteers, health department consultants, etc.) were explored across research intervention efforts, there were some notable gaps. Interpersonal (i.e., family-level) interventions have been explored in immigrant settings [33, 52] in part driven by the strong role family members have been observed to play in impacting socio-cultural and economic factors relevant to immigrant health and behavior change [53, 54]. However, few interventions utilized family members as change agents themselves. For example, U.S.-born children of certain immigrant communities, who also display significant and disproportionate lifestyle and health-related disparities compared to both their first-generation parents and the wider U.S. population, may also represent important intervention agents in their household with respect to health outcomes [55]. One approach to family-level lifestyle interventions relevant to hypertension reduction has been engaging with different family members in a single intervention [33]. However, another area worthy of exploration includes interventions aimed at either the health needs of one family member (e.g., children) as a means of indirectly fostering wider family-level health improvements, which has been explored in the context of hypertension prevention in China [56], or potentially training select family members as intervention agents themselves to foster family-wide improvements. Given the unique social, cultural, linguistic, and often trust barriers associated with interventions conducted in immigrant communities [7], innovation in the context of intervention agents has a particular potential to meet the hypertension needs of this population.
Enhancing the Design, Adaptability, and Evaluation of Immigrant Hypertension Interventions
In examining recent developments in immigrant hypertension interventions through the CFIR framework, a number of future considerations with respect to design, implementation, and evaluation of these programs were identified. At the design level, the role of outer-setting stakeholders (such as community or organizational partners) was most commonly centered around participant recruitment efforts, although multiple interventions (informed by principles of CBPR) also engaged with these stakeholders throughout the intervention development and implementation process. Importantly, efforts to both maintain these collaborations after the intervention period and foster long-term community collaborations are pivotal to not only sustaining blood pressure control, but also enhancing efficacy and reach of future intervention efforts. For example, pre-existing community-coalitions from past research intervention efforts were used by Yi et al. in identifying study sites [47••], with the design of the intervention itself also tailored to align with the organizational structure and priorities of community partners. Indeed, the health needs of immigrants are diverse and interconnected [57], thus collaborating with community stakeholders across multiple integration efforts and designing hypertension interventions to both build upon past coalitions as well as set up the framework for future sustained partnerships can be instrumental in demonstrating that the broader wellbeing of immigrant communities is at the core of research.
Likewise, enhancing the evaluation of hypertension intervention implementation in immigrant contexts is an area for future research, particularly with respect to allowing for adaptations during an intervention to meet evolving participant needs or circumstances. While multiple interventions were observed to assess general participant feedback regarding intervention implementation and components following their completion, establishing protocols for feedback from both participants and community members throughout an intervention can significantly enhance efforts to refine and adapt. Ursua et al., for example, met with a community coalition monthly and used these meetings to constantly refine recruitment, outreach, and intervention procedures [40]; these evaluations resulted in identifying new study sites and partners (e.g., engaging Filipino chess groups for recruitment), as well as neighborhood and organizational level changes to support CHW health promotion efforts for participants (e.g., church-based line dancing and yoga classes for participants to attend). Thus, allowing for adaptability in intervention approach through feedback loops and evaluation procedures may not only help identify new ways of enhancing intervention efficacy but also ensure the evolving and complex socio-ecological factors involved in immigrant hypertension disparities are appropriately addressed.
COVID-19 and New Challenges and Opportunities in Immigrant Hypertension Interventions
Finally, the COVID-19 pandemic of 2020 has evolved into one of the most disruptive global health crises in modern history, placing a significant health, economic, and social burden on immigrant communities (such as those in the U.S.), and exacerbating many health disparities [58, 59]. The disproportionate impact of the COVID-19 pandemic on immigrants has been understood through medical (e.g., lack of insurance, higher prevalence of co-morbidities), economic (e.g., more likely to have jobs with higher risk of the SARS-CoV-2 virus exposure), legal (e.g., fears regarding healthcare system), and social (e.g., crowded, multigenerational households, limited Internet or English proficiency, anti-immigrant rhetoric/xenophobia) factors [58]. Lifestyle behavioral changes have also been observed across the U.S. and globally [60], which has contributed to growing concerns on the rise of NCDs, including hypertension [61]. Importantly, COVID-19 patients with hypertension are also at an increased likelihood of severe symptoms [35] and death [36], adding an additional burden to hypertensive immigrants.
Thus, the COVID-19 pandemic has not only shed a greater light on the health disparities faced by immigrants in the U.S. (particularly those with NCDs such as hypertension) but creates a new set of considerations vital in the design, implementation, and evaluation of hypertension interventions in these communities. These considerations will not only need to consider the changing social, economic, and health needs of immigrants during and after the COVID-19 pandemic but also simply how to safely and appropriately engage with these communities in the pandemic context (as well as adapt to future, post-COVID-19–related fears and concerns). Early evidence of this was observed in the intervention designed by Oshunluyi et al. occurring during the COVID-19 pandemic [37••]. The intervention involved 20 participants and four volunteers sitting 6 ft apart (to maintain social distancing) with everyone being provided masks, hand washing supplies, and hand sanitizer [37••]. Importantly, in their protocol, researchers also planned for an alternative virtual format of the intervention (as well as data collection) in case local or state restrictions were placed during the study period for in-person gatherings [37••]. Indeed, the future of immigrant hypertension interventions both during and post-COVID-19 may necessitate new degrees of flexibility with respect to intervention format; not only will greater scrutiny be needed on the immediate safety concerns of participants but also greater unpredictability with respect to policy and funding environments, and new, evolving, and potentially lingering concerns related to in-person contact. Likewise, the dramatic social and financial impact that has been observed among U.S. immigrant communities during COVID-19 [58] may present important new barriers to recruitment in hypertension interventions; interventionists may need to consider new ways of connecting hypertension reduction aims with other community needs or concerns (e.g., awareness regarding the link between hypertension and COVID-19 morbidity and mortality).
However, while virtual public health interventions aimed at specific drivers of hypertension disparities, such as mobile health (mHealth) approaches to salt consumption reduction [62•] and home blood pressure monitoring [63], had become more common even before the COVID-19 pandemic, their application has been limited in immigrant communities due to the unique socio-economic barriers faced by immigrants (e.g., limited Internet access and ownership of electronic devices to allow for video-based interfaces). However, these limitations may also pave the way for new, innovative, tailored approaches to engage with immigrants in virtual settings. For example, though Hispanic adults in the U.S. remain much less likely than White adults to own a computer or have high-speed Internet, a rise in smartphone usage among Hispanic Americans has significantly helped bridge the digital divide they face in the U.S. [64]. Indeed, increased use of mHealth technologies in immigrant interventions has been observed in recent years [65], and coupled with the fact that many video-conferencing software such as Zoom and Webex are being explored in research interventions during the COVID-19 to allow for smartphone-based or phone-based interfaces as well [66], mHealth-based hypertension interventions (particularly during the era of COVID-19) have a strong potential in immigrant settings. WhatsApp is another mobile-based platform which has been increasingly explored in U.S. immigrant health intervention design due to its particular popularity among immigrant communities compared to other populations [67, 68]; the important potential of exploring WhatsApp-based hypertension intervention designs may be particularly heightened during and after the COVID-19 pandemic.
Conclusion
To meet the complex and emerging hypertension-related burden faced by immigrants in the U.S., researchers and public health professionals face a unique set of challenges in the design, implementation, and evaluation of community-based public health interventions to address these needs. Recent efforts in immigrant hypertension interventions have shed light on new and multi-faceted ways of addressing this hypertension burden, as well as pin-point areas of further consideration. The CFIR framework provided a useful lens to examine these developments and explore the need for innovation across different stages of intervention research, including characteristics of participants (disaggregating immigrant health needs and adapting to the unique socio-demographic circumstances faced by communities), intervention characteristics (exploring new intervention designs and sources, as well as enhancing recruitment methods), inner setting (engaging with different types of intervention agents), outer setting (collaborating with a diverse set of stakeholders throughout multiple stages of the research process, including in intervention implementation and evaluation), and process (enhancing mixed-method assessments of an intervention throughout its implementation to allow for efficient adaptability). The need for this innovation is further compounded by the emerging challenges that the COVID-19 pandemic places on both immigrant communities and research intervention efforts. Indeed, through intervention development efforts that are reflective of both these immigrant needs and the various key components of intervention design outlined, addressing hypertension disparities faced immigrants both during and after the COVID-19 pandemic can be more effectively conducted.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Commodore-Mensah Y, Selvin E, Aboagye J, Turkson-Ocran R-A, Li X, Himmelfarb CD, et al. Hypertension, overweight/obesity, and diabetes among immigrants in the United States: an analysis of the 2010–2016 National Health Interview Survey. BMC Public Health. 2018;18(1):773 This study is among the few disagregated analyses (using representative data) of hypertension prevelence across specific dissagregated immigrant populations by national or regional origin (including disagregating participants by those originating from South America with those originating from Mexico, Central America, and the Caribbean).
Chen M-L, Hu J. Health disparities in Chinese Americans with hypertension: a review. Int J Nurs Sci. 2014;1(3):318–22.
Guadamuz Jenny S, Durazo-Arvizu Ramon A, Daviglus Martha L, Calip Gregory S, Nutescu Edith A, Qato Dima M. Citizenship status and the prevalence, treatment, and control of cardiovascular disease risk factors among adults in the United States, 2011–2016. Circ Cardiovasc Qual Outcomes. 2020;13(3):e006215.
Million Hearts. Estimated hypertension prevalence, treatment, and control among U.S. adults. 2020. Accessed 12 Nov 2020. Available from: https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html.
Camorata SA, Zeigler K. Projecting the Impact of Immigration on the U.S. Population: a look at size and age structure through 2060. 2019. Accessed 5 Nov 2020. Available from: https://cis.org/Report/Projecting-Impact-Immigration-US-Population.
Kochhar R, Cilluffo A. Income inequality in the U.S. is rising most rapidly among Asians. 2018. Accessed 5 Nov. Available from: https://www.pewsocialtrends.org/2018/07/12/income-inequality-in-the-u-s-is-rising-most-rapidly-among-asians/.
Diaz E, Ortiz-Barreda G, Ben-Shlomo Y, Holdsworth M, Salami B, Rammohan A, et al. Interventions to improve immigrant health. A scoping review. Eur J Pub Health. 2017;27(3):433–9.
Young M-EDT, Pebley AR. Legal status, time in the USA, and the well-being of Latinos in Los Angeles. J Urban Health. 2017;94(6):764–75.
Fei K, Rodriguez-Lopez JS, Ramos M, Islam N, Trinh-Shevrin C, Yi SS, et al. Racial and ethnic subgroup disparities in hypertension prevalence, New York City health and nutrition examination survey, 2013-2014. Prev Chronic Dis. 2017;14:E33.
Yi S, Elfassy T, Gupta L, Myers C, Kerker B. Nativity, language spoken at home, length of time in the United States, and race/ethnicity: associations with self-reported hypertension. Am J Hypertens. 2014;27(2):237–44.
Russo R, Foster V, Kwon SC, Kranick J, Chebli P, Trinh-Shevrin C, et al. Hidden in plain sight: health disparities among foreign-born whites in New York City. Ethn Dis. Under review.
• Divney AA, Echeverria SE, Thorpe LE, Trinh-Shevrin C, Islam NS. Hypertension prevalence jointly influenced by acculturation and gender in US immigrant groups. Am J Hypertens. 2019;32(1):104–11 This study provided some of the first comprehensive insights into the the interaction between gender and accultration in the prevalence of hypertension among both Latino and Asian American populations.
Brown AGM, Houser RF, Mattei J, Mozaffarian D, Lichtenstein AH, Folta SC. Hypertension among US-born and foreign-born non-Hispanic blacks: National Health and nutrition examination survey 2003-2014 data. J Hypertens. 2017;35(12):2380–7.
Lee S, Martinez G, Ma GX, Hsu CE, Robinson ES, Bawa J, et al. Barriers to health care access in 13 Asian American communities. Am J Health Behav. 2010;34(1):21–30.
Hacker K, Anies M, Folb BL, Zallman L. Barriers to health care for undocumented immigrants: a literature review. Risk Manag Healthc Policy. 2015;8:175–83.
Salami A. Immigrant eligibility for health care programs in the United States. 2017. Accessed 27 Oct 2020. Available from: https://www.ncsl.org/research/immigration/immigrant-eligibility-for-health-care-programs-in-the-united-states.aspx.
O’Fallon A. Culture within a culture: US immigrants confront a health system that many citizens can’t manage. AMA J Ethics. 2005;7(7):509–13.
Perreira KM, Crosnoe R, Fortuny K, Pedroza J, Ulvestad K, Weiland C, et al. Barriers to immigrants’ access to health and human services programs. ASPE Issue Brief Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. 2012.
Omenka OI, Watson DP, Hendrie HC. Understanding the healthcare experiences and needs of African immigrants in the United States: a scoping review. BMC Public Health. 2020;20(1):27.
Kaiser Family Foundation. Changes to “public charge” inadmissibility rule: implications for health and health coverage. 2019. Accessed 5 Nov 2020. Available from: https://www.kff.org/racial-equity-and-health-policy/fact-sheet/public-charge-policies-for-immigrants-implications-for-health-coverage/.
Agency for Healthcare Research and Quality. Consider culture, customs, and beliefs: Tool #10. 2020. Accessed 27 Oct 2020. Available from: https://www.ahrq.gov/health-literacy/improve/precautions/tool10.html.
Langellier BA, Garza JR, Glik D, Prelip ML, Brookmeyer R, Roberts CK, et al. Immigration disparities in cardiovascular disease risk factor awareness. J Immigr Minor Health. 2012;14(6):918–25.
Zallman L, Himmelstein DH, Woolhandler S, Bor DH, Ayanian JZ, Wilper AP, et al. Undiagnosed and uncontrolled hypertension and hyperlipidemia among immigrants in the US. J Immigr Minor Health. 2013;15(5):858–65.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24(2).
Beilin LJ, Puddey IB, Burke V. Lifestyle and hypertension. Am J Hypertens. 1999;12(9):934–45.
Patel M, Phillips-Caesar E, Boutin-Foster C. Barriers to lifestyle behavioral change in migrant south Asian populations. J Immigr Minor Health. 2012;14(5):774–85.
Martinez J, Powell J, Agne A, Scarinci I, Cherrington A. A focus group study of Mexican immigrant Men's perceptions of weight and lifestyle. Public Health Nurs. 2012;29(6):490–8.
Wieland ML, Tiedje K, Meiers SJ, Mohamed AA, Formea CM, Ridgeway JL, et al. Perspectives on physical activity among immigrants and refugees to a small urban community in Minnesota. J Immigr Minor Health. 2015;17(1):263–75.
Vaughn LM, Jacquez F, Lindquist-Grantz R, Parsons A, Melink K. Immigrants as research partners: a review of immigrants in community-based participatory research (CBPR). J Immigr Minor Health. 2017;19(6):1457–68.
Renzaho AMN, Mellor D, Boulton K, Swinburn B. Effectiveness of prevention programmes for obesity and chronic diseases among immigrants to developed countries – a systematic review. Public Health Nutr. 2010;13(3):438–50.
Joo JY, Liu MF. Experience of culturally-tailored diabetes interventions for ethnic minorities: a qualitative systematic review. Clin Nurs Res. 2019:1054773819885952.
Hyman I, Guruge S. A review of theory and health promotion strategies for new immigrant. Can J Public Health. 2002;93(3):183–7.
Wieland ML, Weis JA, Hanza MMK, Meiers SJ, Patten CA, Clark MM, et al. Healthy immigrant families: participatory development and baseline characteristics of a community-based physical activity and nutrition intervention. Contemp Clin Trials. 2016;47:22–31.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50.
Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21–e.
Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M, et al. Age and multimorbidity predict death among COVID-19 patients. Hypertension. 2020;76(2):366–72.
•• Oshunluyi E. Providing hypertension education to African immigrants at a Southern California Congregation during the COVID-19 pandemic. 2020. Accessed 28 Oct 2020. Available from: https://repository.usfca.edu/cgi/viewcontent.cgi?article=1250&context=dnp. This study is among the first known immigrant hypertension interventions during the COVID-19 pandemic and sheds light onto the challenges and opportunities in COVID-19 related innovations.
Erskine S. The impact of culturally-tailored education on knowledge and behavior related to screening and lifestyle management of blood pressure in African immigrants. 2020. Accessed 28 Oct 2020. Available from: https://digitalscholarship.unlv.edu/cgi/viewcontent.cgi?article=4895&context=thesesdissertations.
•• Ma GX, Bhimla A, Zhu L, Beeber M, Aczon F, Tan Y, et al. Development of an intervention to promote physical activity and reduce dietary sodium intake for preventing hypertension and chronic disease in Filipino Americans. J Racial Ethn Health Disparities. 2020. This intervention used interactive mobile phone technologies to measure or monitor physical activity and salt intake among participants, and coupled the use of these mobile technologies with physical activities sessions.
Ursua RA, Aguilar DE, Wyatt LC, Trinh-Shevrin C, Gamboa L, Valdellon P, et al. A community health worker intervention to improve blood pressure among Filipino Americans with hypertension: a randomized controlled trial. Prev Med Rep. 2018;11:42–8.
Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health. 2019;16(7).
•• Langabeer JR 2nd, Henry TD, Perez Aldana C, DeLuna L, Silva N, Champagne-Langabeer T. Effects of a Community Population Health Initiative on Blood Pressure Control in Latinos. J Am Heart Assoc. 2018;7(21):e010282 This study specifically targeted Latinos in the U.S. and included personalized intervention components along with providing many participants blood pressure cuffs.
Kling HE, D'Agostino EM, Booth JV, Patel H, Hansen E, Mathew MS, et al. The effect of a park-based physical activity program on cardiovascular, strength, and mobility outcomes among a sample of racially/ethnically diverse adults aged 55 or older. Prev Chronic Dis. 2018;15:E166.
Li W-W, Lu T-L, Huang D. Development and pilot test of a Chinese medicine as longevity modality (CALM) videos in improving hypertension management in Chinese immigrants: feasibility of educational and storytelling video. GSTF J Nurs Health Care (JNHC). 2020;5(2).
•• Lopez PM, Zanowiak J, Goldfeld K, Wyka K, Masoud A, Beane S, et al. Protocol for project IMPACT (improving millions hearts for provider and community transformation): a quasi-experimental evaluation of an integrated electronic health record and community health worker intervention study to improve hypertension management among South Asian patients. BMC Health Serv Res. 2017;17(1):810 This intervention utilized the stepped-wedged quasi-exerminetal study design, a novel design which involves the sequetional cross-over of clusters of participants in the intervention and control group untill all clusters are exposed to an intervention.
Lopez PM, Divney A, Goldfeld K, Zanowiak J, Gore R, Kumar R, et al. Feasibility and outcomes of an electronic health record intervention to improve hypertension management in immigrant-serving primary care practices. Med Care. 2019;57(Suppl 6 Suppl 2):S164–s71.
•• Yi SS, Wyatt LC, Patel S, Choy C, Dhar R, Zanowiak JM, et al. A faith-based intervention to reduce blood pressure in underserved Metropolitan New York immigrant communities. Prev Chronic Dis. 2019;16:E106 This intervention uniquely focused on the faith-based setting for distinct Asian American subgroups (Korean, Bangladeshi, Filipino, Sikh Asian Indian) and sought to build the capacity of participants learning from a practice-based model developed by the local city health department.
Enchautegui ME. The job quality of U.S. immigrants. Ind Relat J Econ Soc. 2008;47(1):108–13.
Read JG, Smith PB. Gender and national origin differences in healthcare utilization among U.S. Immigrants from Mexico, China, and India. Ethn Health. 2018;23(8):867–83.
Ali SH, Misra S, Parekh N, Murphy B, DiClemente RJ. Preventing type 2 diabetes among South Asian Americans through community-based lifestyle interventions: a systematic review. Prev Med Rep. 2020;20:101182.
Ku L, Matani S. Left out: immigrants’ access to health care and insurance. Health Aff. 2001;20(1):247–56.
Tovar A, Renzaho AMN, Guerrero AD, Mena N, Ayala GX. A systematic review of obesity prevention intervention studies among immigrant populations in the US. Curr Obes Rep. 2014;3(2):206–22.
Chiswick BR, Lee YL, Miller PW. Family matters: the role of the family in immigrants’ destination language acquisition. J Popul Econ. 2005;18(4):631–47.
Blumenberg E, Smart M. Getting by with a little help from my friends…and family: immigrants and carpooling. Transportation. 2010;37(3):429–46.
Ali SH, DiClemente RJ, Parekh N. Changing the landscape of South Asian migrant health research by advancing second-generation immigrant health needs. Transl Behav Med. 2020;ibaa084.
He FJ, Wu Y, Ma J, Feng X, Wang H, Zhang J, et al. A school-based education programme to reduce salt intake in children and their families (school-EduSalt): protocol of a cluster randomised controlled trial. BMJ Open. 2013;3(7):e003388.
World Health Organization. Noncommunicable diseases and migrant health. 2019. Accessed 18 Nov 2020. Available from: https://www.euro.who.int/__data/assets/pdf_file/0005/399065/NCDs-and-migrant-health-ENG.PDF.
Clark E, Fredricks K, Woc-Colburn L, Bottazzi ME, Weatherhead J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl Trop Dis. 2020;14(7):e0008484.
Greenaway C, Hargreaves S, Barkati S, Coyle CM, Gobbi F, Veizis A, et al. COVID-19: exposing and addressing health disparities among ethnic minorities and migrants. J Travel Med. 2020:taaa113.
Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol. 2020;25(9):1155–63.
Shah B. Tracking COVID-19’s effect on the nation’s high blood pressure. 2020. Accessed 5 Nov 2020. Available from: https://www.livongo.com/covid-blood-pressure/.
• Ali SH, Luo R, Li Y, Liu X, Tang C, Zhang P. Application of mobile health technologies aimed at salt reduction: systematic review. JMIR Mhealth Uhealth. 2019;7(4):e13250 This review analyzed innovative uses of mobile health technologies aimed at salt consumption reduction, higlighting the need for further rigorous large-scale interventions using new and interactive mHealth technologies aimed at changing dietary salt intake.
Shimbo D, Artinian Nancy T, Basile Jan N, Krakoff Lawrence R, Margolis Karen L, Rakotz Michael K, et al. Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation. 2020;142(4):e42–63.
Perrin A, Turner E. Smartphones help blacks, Hispanics bridge some – but not all – digital gaps with whites. 2019. Accessed 5 Nov 2020. Available from: https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/.
Lin Y-H, Lou M-F. Effects of mHealth-based interventions on health literacy and related factors: a systematic review. J Nurs Manag. 2020; Online ahead of print.
Stiles-Shields C, Plevinsky JM, Psihogios AM, Holmbeck GN. Considerations and future directions for conducting clinical research with pediatric populations during the COVID-19 pandemic. J Pediatr Psychol. 2020;45(7):720–4.
Castellano S, Loker K. How documented uses WhatsApp to reach local immigrant communities. 2020. Accessed 5 Nov 2020. Available from: https://www.americanpressinstitute.org/publications/how-documented-uses-whatsapp-to-reach-local-immigrant-communities/.
Manjoo F. For millions of immigrants, a common language: WhatsApp. 2016. Accessed 5 Nov 2020 November. Available from: https://www.nytimes.com/2016/12/21/technology/for-millions-of-immigrants-a-common-language-whatsapp.html.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Blood Pressure Monitoring and Management
Rights and permissions
About this article
Cite this article
Ali, S.H., Islam, N.S., Commodore-Mensah, Y. et al. Implementing Hypertension Management Interventions in Immigrant Communities in the U.S.: a Narrative Review of Recent Developments and Suggestions for Programmatic Efforts. Curr Hypertens Rep 23, 5 (2021). https://doi.org/10.1007/s11906-020-01121-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11906-020-01121-6