Abstract
Purpose of Review
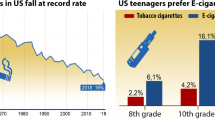
Tobacco smoking is the most significant modifiable risk factor in the development of cardiovascular disease (CVD). Exposure to mainstream cigarette smoke (MCS) is associated with CVD through the development of endothelial dysfunction, a condition characterized by an imbalance of vasoactive factors in the vasculature. This dysfunction is thought to be induced in part by aldehydes generated at high levels in MCS.
Recent Findings
Electronic cigarettes (e-cigs) may also pose CVD risk. Although the health effects of e-cigs are still largely unknown, the presence of aldehydes in e-cig aerosol suggests that e-cigs may induce adverse cardiovascular outcomes similar to those seen with MCS exposure.
Summary
Herein, we review studies of traditional and emerging tobacco product use, shared harmful and potentially harmful constituents, and measures of biomarkers of harm (endothelial dysfunction) to examine a potential and distinct role of aldehydes in cardiovascular harm associated with cigarette and e-cig use.

Similar content being viewed by others
Abbreviations
- CAC:
-
Circulating angiogenic cell
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- E-cig:
-
Electronic cigarette
- ENDS:
-
Electronic nicotine delivery systems
- FMD:
-
Flow-mediated dilation
- GRAS:
-
Generally regarded as safe
- HPHCs:
-
Harmful or potentially harmful constituents
- MCS:
-
Mainstream cigarette smoke
- NO:
-
Nitric oxide
- OS:
-
Oxidative stress
- PG:
-
Propylene glycol
- PM:
-
Particulate matter
- ROS:
-
Reactive oxygen species
- SHS:
-
Secondhand smoke
- sICAM-1:
-
Soluble intercellular adhesion molecule 1
- sVCAM-1:
-
Soluble vascular adhesion molecule 1
- US FDA:
-
US Food and Drug Administration
- VG:
-
Vegetable glycerin
- WBCs:
-
White blood cells
- WHO:
-
World Health Organization
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bhatnagar A. Environmental cardiology: studying mechanistic links between pollution and heart disease. Circ Res. 2006;99(7):692–705. https://doi.org/10.1161/01.RES.0000243586.99701.cf.
U.S. Food & Drug Administration. Harmful and potentially harmful constituents in tobacco products and tobacco smoke: Established List. 2012. www.fda.gov. Accessed November 6, 2017.
Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. https://doi.org/10.1161/CIR.0b013e3181dbece1.
Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: testing and clinical relevance. Circulation. 2007;115(10):1285–95. https://doi.org/10.1161/circulationaha.106.652859.
Marchio P, Guerra-Ojeda S, Vila JM, Aldasoro M, Victor VM, Mauricio MD. Targeting early atherosclerosis: a focus on oxidative stress and inflammation. Oxidative Med Cell Longev. 2019;2019:8563845–32. https://doi.org/10.1155/2019/8563845.
Cui M, Cui R, Liu K, Dong J-Y, Imano H, Hayama-Terada M, et al. Associations of tobacco smoking with impaired endothelial function: the Circulatory Risk in Communities Study (CIRCS). J Atheroscler Thromb. 2018;25(9):836–45. https://doi.org/10.5551/jat.42150.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150(3):606–12. https://doi.org/10.1016/j.chest.2016.04.012.
Pedersen KM, Çolak Y, Ellervik C, Hasselbalch HC, Bojesen SE, Nordestgaard BG. Smoking and increased white and red blood cells. Arterioscl Throm Vas. 2019;39(5):965–77. https://doi.org/10.1161/ATVBAHA.118.312338.
Higuchi T, Omata F, Tsuchihashi K, Higashioka K, Koyamada R, Okada S. Current cigarette smoking is a reversible cause of elevated white blood cell count: cross-sectional and longitudinal studies. Prev Med Rep. 2016;4:417–22. https://doi.org/10.1016/j.pmedr.2016.08.009.
Kondo T, Hayashi M, Takeshita K, Numaguchi Y, Kobayashi K, Iino S, et al. Smoking cessation rapidly increases circulating progenitor cells in peripheral blood in chronic smokers. Arterioscler Thromb Vasc Biol. 2004;24(8):1442–7. https://doi.org/10.1161/01.ATV.0000135655.52088.c5.
•• Conklin DJ, Schick S, Blaha MJ, Carll A, DeFilippis A, Ganz P, et al. Cardiovascular injury induced by tobacco products: assessment of risk factors and biomarkers of harm. A Tobacco Centers of Regulatory Science compilation. Am J Phys Heart Circ Phys. 2019;316(4):H801–H27. https://doi.org/10.1152/ajpheart.00591.2018This review evaluates the effects of traditional tobacco products on cardiovascular disease risk and related biomarkers of harm as well as the risk imposed by emerging tobacco products. .
Scott DA, Palmer RM. The influence of tobacco smoking on adhesion molecule profiles. Tob Induc Dis. 2002;1(1):3. https://doi.org/10.1186/1617-9625-1-3.
Delgado GE, Krämer BK, Siekmeier R, Yazdani B, März W, Leipe J, et al. Influence of smoking and smoking cessation on biomarkers of endothelial function and their association with mortality. Atherosclerosis. 2020;292:52–9. https://doi.org/10.1016/j.atherosclerosis.2019.11.017.
Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34(3):509–15. https://doi.org/10.1161/atvbaha.113.300156.
• Fetterman JL, Weisbrod RM, Feng B, Bastin R, Tuttle ST, Holbrook M, et al. Flavorings in tobacco products induce endothelial cell dysfunction. Arterioscler Thromb Vasc Biol. 2018. https://doi.org/10.1161/atvbaha.118.311156This study demonstrates that short-term exposure to select flavorings used in electronic cigarettes can impair nitric oxide production in endothelial cells.
Morris PB, Ference BA, Jahangir E, Feldman DN, Ryan JJ, Bahrami H, et al. Cardiovascular effects of exposure to cigarette smoke and electronic cigarettes: clinical perspectives from the Prevention of Cardiovascular Disease Section Leadership Council and Early Career Councils of the American College of Cardiology. J Am Coll Cardiol. 2015;66(12):1378–91. https://doi.org/10.1016/j.jacc.2015.07.037.
Nocella C, Biondi-Zoccai G, Sciarretta S, Peruzzi M, Pagano F, Loffredo L, et al. Impact of tobacco versus electronic cigarette smoking on platelet function. Am J Cardiol. 2018;122(9):1477–81. https://doi.org/10.1016/j.amjcard.2018.07.029.
Kuntic M, Oelze M, Steven S, Kroller-Schon S, Stamm P, Kalinovic S, et al. Short-term e-cigarette vapour exposure causes vascular oxidative stress and dysfunction: evidence for a close connection to brain damage and a key role of the phagocytic NADPH oxidase (NOX-2). Eur Heart J. 2019;41:2472–83. https://doi.org/10.1093/eurheartj/ehz772.
Moheimani RS, Bhetraratana M, Yin F, Peters KM, Gornbein J, Araujo JA, et al. Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: implications for cardiovascular risk. JAMA Cardiol. 2017;2(3):278–84. https://doi.org/10.1001/jamacardio.2016.5303.
Qasim H, Karim ZA, Silva-Espinoza JC, Khasawneh FT, Rivera JO, Ellis CC, et al. Short-term E-cigarette exposure increases the risk of thrombogenesis and enhances platelet function in mice. J Am Heart Assoc. 2018;7(15):e009264. https://doi.org/10.1161/JAHA.118.009264.
Hom S, Chen L, Wang T, Ghebrehiwet B, Yin W, Rubenstein DA. Platelet activation, adhesion, inflammation, and aggregation potential are altered in the presence of electronic cigarette extracts of variable nicotine concentrations. Platelets. 2016;27(7):694–702. https://doi.org/10.3109/09537104.2016.1158403.
Kim M, Han C-H, Lee M-Y. NADPH oxidase and the cardiovascular toxicity associated with smoking. Toxicol Res. 2014;30(3):149–57. https://doi.org/10.5487/TR.2014.30.3.149.
•• Rao P, Liu J, Springer ML. JUUL and combusted cigarettes comparably impair endothelial function. Tob Regul Sci. 2020;6(1):30–7. https://doi.org/10.18001/trs.6.1.4This study demonstrates that rats exposed to aerosol from a JUUL device containing Virginia Tobacco flavoring had impaired flow-mediated dilation, indicating impaired endothelial function, which is one of the earliest changes in the development of cardiovascular disease.
• Caporale A, Langham MC, Guo W, Johncola A, Chatterjee S, Wehrli FW. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology. 2019;293(1):97–106. https://doi.org/10.1148/radiol.2019190562This study is one of the first to indicate that the adverse cardiovascular effects induced by e-cigarette use may not be solely related to nicotine.
Sussan TE, Gajghate S, Thimmulappa RK, Ma J, Kim J-H, Sudini K, et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PLoS One. 2015;10(2):e0116861. https://doi.org/10.1371/journal.pone.0116861.
Espinoza-Derout J, Hasan KM, Shao XM, Jordan MC, Sims C, Lee DL, et al. Chronic intermittent electronic cigarette exposure induces cardiac dysfunction and atherosclerosis in apolipoprotein-E knockout mice. Am J Physiol Heart Circ Physiol. 2019;317(2):H445–H59. https://doi.org/10.1152/ajpheart.00738.2018.
Zhao J, Hopke PK. Concentration of reactive oxygen species (ROS) in mainstream and sidestream cigarette smoke. Aerosol Sci Technol. 2012;46(2):191–7. https://doi.org/10.1080/02786826.2011.617795.
Valavanidis A, Vlachogianni T, Fiotakis K. Tobacco smoke: involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int J Environ Res Public Health. 2009;6(2):445–62. https://doi.org/10.3390/ijerph6020445.
Lerner CA, Sundar IK, Watson RM, Elder A, Jones R, Done D, et al. Environmental health hazards of e-cigarettes and their components: oxidants and copper in e-cigarette aerosols. Environ Pollut (Barking, Essex : 1987). 2015;198:100–7. https://doi.org/10.1016/j.envpol.2014.12.033.
Zuo L, Zhou T, Pannell BK, Ziegler AC, Best TM. Biological and physiological role of reactive oxygen species--the good, the bad and the ugly. Acta Physiol (Oxford, England). 2015;214(3):329–48. https://doi.org/10.1111/apha.12515.
Yang W, Omaye ST. Air pollutants, oxidative stress and human health. Mutat Res/Genet Toxicol Environ Mutagen. 2009;674(1):45–54. https://doi.org/10.1016/j.mrgentox.2008.10.005.
Betteridge DJ. What is oxidative stress? Metabolism. 2000;49(2 Suppl 1):3–8.
Brieger K, Schiavone S, Miller FJ Jr, Krause KH. Reactive oxygen species: from health to disease. Swiss Med Wkly. 2012;142:w13659. https://doi.org/10.4414/smw.2012.13659.
Huang MF, Lin WL, Ma YC. A study of reactive oxygen species in mainstream of cigarette. Indoor Air. 2005;15(2):135–40. https://doi.org/10.1111/j.1600-0668.2005.00330.x.
Ghiadoni L, Salvetti M, Muiesan ML, Taddei S. Evaluation of endothelial function by flow mediated dilation: methodological issues and clinical importance. High Blood Press Cardiovascul Prevent. 2015;22(1):17–22. https://doi.org/10.1007/s40292-014-0047-2.
Mazzone A, Cusa C, Mazzucchelli I, Vezzoli M, Ottini E, Ghio S, et al. Cigarette smoking and hypertension influence nitric oxide release and plasma levels of adhesion molecules. Clin Chem Lab Med. 2001;39(9):822–6. https://doi.org/10.1515/cclm.2001.136.
Conklin DJ, Ogunwale MA, Chen Y, Theis WS, Nantz MH, Fu X-A, et al. Electronic cigarette-generated aldehydes: the contribution of e-liquid components to their formation and the use of urinary aldehyde metabolites as biomarkers of exposure. Aerosol Sci Technol. 2018;52(11):1219–32. https://doi.org/10.1080/02786826.2018.1500013.
Hutzler C, Paschke M, Kruschinski S, Henkler F, Hahn J, Luch A. Chemical hazards present in liquids and vapors of electronic cigarettes. Arch Toxicol. 2014;88(7):1295–308. https://doi.org/10.1007/s00204-014-1294-7.
Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine Tobacco Res. 2013;15(1):158–66. https://doi.org/10.1093/ntr/nts103.
Bertholon JF, Becquemin MH, Annesi-Maesano I, Dautzenberg B. Electronic cigarettes: a short review. Respiration. 2013;86(5):433–8. https://doi.org/10.1159/000353253.
•• Ogunwale MA, Li M, Ramakrishnam Raju MV, Chen Y, Nantz MH, Conklin DJ, et al. Aldehyde detection in electronic cigarette aerosols. ACS Omega. 2017;2(3):1207–14. https://doi.org/10.1021/acsomega.6b00489This study measures levels of aldehydes (formaldehyde, acetaldehyde, and acrolein) in e-cigarette aerosols. These aldehydes are known to contribute significantly to the adverse cardiovascular effects related to the use of traditional cigarettes and thus indicate the risk of using e-cigarettes.
Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Therapeut Adv Drug Safety. 2014;5(2):67–86. https://doi.org/10.1177/2042098614524430.
Korzun T, Lazurko M, Munhenzva I, Barsanti KC, Huang Y, Jensen RP, et al. E-cigarette airflow rate modulates toxicant profiles and can Lead to concerning levels of solvent consumption. ACS Omega. 2018;3(1):30–6. https://doi.org/10.1021/acsomega.7b01521.
Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults-United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68:1013–9 https://doi.org/10.15585/mmwr.mm6845a2.
Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P, et al. Reasons for current E-cigarette use among U.S. adults. Prev Med. 2016;93:14–20. https://doi.org/10.1016/j.ypmed.2016.09.011.
Gentzke AS, Creamer M, Cullen KA, Ambrose BK, Willis G, Jamal A, et al. Vital signs: tobacco product use among middle and high school students - United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2019;68(6):157–64. https://doi.org/10.15585/mmwr.mm6806e1.
•• National Academies of Sciences E, Medicine. Public health consequences of E-cigarettes. Washington, DC: The National Academies Press; 2018. This comprehensive report presents a critical assessment of the current studies examining the health effects of e-cigarettes and highlights gaps in the data that present opportunities for future research.
Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2013;23:133–9. https://doi.org/10.1136/tobaccocontrol-2012-050859.
Cho JH. The association between electronic-cigarette use and self-reported oral symptoms including cracked or broken teeth and tongue and/or inside-cheek pain among adolescents: a cross-sectional study. PLoS One. 2017;12(7):e0180506. https://doi.org/10.1371/journal.pone.0180506.
Palamidas A, Tsikrika S, Katsaounou PA, Vakali S, Gennimata S-A, Kaltsakas G, et al. Acute effects of short term use of e-cigarettes on airways physiology and respiratory symptoms in smokers with and without airways obstructive diseases and in healthy non smokers. Tob Prev Cessat. 2017;3(March). https://doi.org/10.18332/tpc/67799.
Gennimata S-A, Palamidas A, Kaltsakas G, Tsikrika S, Vakali S, Gratziou C, et al. Acute effect of e-cigarette on pulmonary function in healthy subjects and smokers. Eur Respir J. 2012;40:P1053.
Vardavas CI, Anagnostopoulos N, Kougias M, Evangelopoulou V, Connolly GN, Behrakis PK. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141(6):1400–6. https://doi.org/10.1378/chest.11-2443.
Shaito A, Saliba J, Husari A, El-Harakeh M, Chhouri H, Hashem Y, et al. Electronic cigarette smoke impairs normal mesenchymal stem cell differentiation. Sci Rep. 2017;7:14281. https://doi.org/10.1038/s41598-017-14634-z.
Vlachopoulos C, Ioakeimidis N, Abdelrasoul M, Terentes-Printzios D, Georgakopoulos C, Pietri P, et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in Young smokers. J Am Coll Cardiol. 2016;67(23):2802–3. https://doi.org/10.1016/j.jacc.2016.03.569.
Antoniewicz L, Bosson JA, Kuhl J, Abdel-Halim SM, Kiessling A, Mobarrez F, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85. https://doi.org/10.1016/j.atherosclerosis.2016.09.064.
Oliveri D, Liang Q, Sarkar M. Real-world evidence of differences in biomarkers of exposure to select harmful and potentially harmful constituents and biomarkers of potential harm between adult E-vapor users and adult cigarette smokers. Nicotine Tob Res. 2019;22:1114–22. https://doi.org/10.1093/ntr/ntz185.
Olfert IM, DeVallance E, Hoskinson H, Branyan KW, Clayton S, Pitzer CR, et al. Chronic exposure to electronic cigarettes results in impaired cardiovascular function in mice. J Appl Physiol (Bethesda, Md : 1985). 2018;124(3):573–82. https://doi.org/10.1152/japplphysiol.00713.2017.
Orzabal MR, Lunde-Young ER, Ramirez JI, Howe SYF, Naik VD, Lee J, et al. Chronic exposure to e-cig aerosols during early development causes vascular dysfunction and offspring growth deficits. Translat Res. 2019;207:70–82. https://doi.org/10.1016/j.trsl.2019.01.001.
Hallagan J. The safety assessment and regulatory authority to use flavors: focus on E-cigarettes. 2014. www.femaflavor.org. Accessed October 10 2019.
Kreiss K. Work-related spirometric restriction in flavoring manufacturing workers. Am J Ind Med. 2014;57(2):129–37. https://doi.org/10.1002/ajim.22282.
Barrington-Trimis JL, Samet JM, McConnell R. Flavorings in electronic cigarettes: an unrecognized respiratory health hazard? JAMA. 2014;312(23):2493–4. https://doi.org/10.1001/jama.2014.14830.
Kaden DA, Mandin C, Nielsen GD, Wolkoff P. Formaldehyde. WHO guidelines for indoor air quality: selected pollutants. Geneva: World Health Organization; 2010.
Baker RR. The generation of formaldehyde in cigarettes--overview and recent experiments. Food Chem Toxicol. 2006;44(11):1799–822. https://doi.org/10.1016/j.fct.2006.05.017.
World Health Organization IPoCS. Acetaldehyde: health and safety guide. In: Organization WH, editor. . Geneva: World Health Organization; 1994.
van Andel I, Sleijffers A, Schenk E, Rambali B, Wolterink G, van de Werken G et al. Adverse health effects of cigarette smoke: aldehydes; crotonaldehyde, butyraldehyde, hexanal, and malonaldehyde. Nutrition, health protection and prevention department, ministry of health, welfare and sports (VWS) and of the food and consumer product safety authority (VWA), editor. Bilthoven, The Netherlands: National Institute for Public Health and the Environment; 2006.
Alwis KU, de Castro BR, Morrow JC, Blount BC. Acrolein exposure in U.S. tobacco smokers and non-tobacco users: NHANES 2005-2006. Environ Health Perspect. 2015;123(12):1302–8. https://doi.org/10.1289/ehp.1409251.
Rubinstein ML, Delucchi K, Benowitz NL, Ramo DE. Adolescent exposure to toxic volatile organic chemicals from E-cigarettes. Pediatrics. 2018;141:e20173557. https://doi.org/10.1542/peds.2017-3557.
Goniewicz ML, Gawron M, Smith DM, Peng M, Jacob P 3rd, Benowitz NL. Exposure to nicotine and selected toxicants in cigarette smokers who switched to electronic cigarettes: a longitudinal within-subjects observational study. Nicotine Tob Res. 2017;19(2):160–7. https://doi.org/10.1093/ntr/ntw160.
Mobarrez F, Antoniewicz L, Hedman L, Bosson JA, Lundback M. Electronic cigarettes containing nicotine increase endothelial and platelet derived extracellular vesicles in healthy volunteers. Atherosclerosis. 2020;301:93–100. https://doi.org/10.1016/j.atherosclerosis.2020.02.010.
Hess CA, Olmedo P, Navas-Acien A, Goessler W, Cohen JE, Rule AM. E-cigarettes as a source of toxic and potentially carcinogenic metals. Environ Res. 2017;152:221–5. https://doi.org/10.1016/j.envres.2016.09.026.
Olmedo P, Goessler W, Tanda S, Grau-Perez M, Jarmul S, Aherrera A, et al. Metal concentrations in e-cigarette liquid and aerosol samples: the contribution of metallic coils. Environ Health Perspect. 2018;126(2):027010. https://doi.org/10.1289/ehp2175.
Lee M-S, LeBouf RF, Son Y-S, Koutrakis P, Christiani DC. Nicotine, aerosol particles, carbonyls and volatile organic compounds in tobacco- and menthol-flavored e-cigarettes. Environ Health. 2017;16(1):42. https://doi.org/10.1186/s12940-017-0249-x.
Vindhyal MR, Ndunda P, Munguti C, Vindhyal S, Okut H. Impact on cardiovascular outcomes among E-cigarette users: a review from National Health Interview Surveys. J Am Coll Cardiol. 2019;73(9 Supplement 2):11. https://doi.org/10.1016/s0735-1097(19)33773-8.
Banks E, Joshy G, Korda RJ, Stavreski B, Soga K, Egger S, et al. Tobacco smoking and risk of 36 cardiovascular disease subtypes: fatal and non-fatal outcomes in a large prospective Australian study. BMC Med. 2019;17(1):128. https://doi.org/10.1186/s12916-019-1351-4.
Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of sudden cardiac death: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2018;33(6):509–21. https://doi.org/10.1007/s10654-017-0351-y.
U.S. Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the surgeon general, 2014. In: USDoHaH, editor. Services. Rockville: Office of the Surgeon General; 2014.
Fernández JAF, Prats JM, Artero JVM, Mora AC, Fariñas AV, Espinal A, et al. Systemic inflammation in 222.841 healthy employed smokers and nonsmokers: white blood cell count and relationship to spirometry. Tob Induc Dis. 2012;10(1):7. https://doi.org/10.1186/1617-9625-10-7.
Mobarrez F, Antoniewicz L, Bosson JA, Kuhl J, Pisetsky DS, Lundback M. The effects of smoking on levels of endothelial progenitor cells and microparticles in the blood of healthy volunteers. PLoS One. 2014;9(2):e90314. https://doi.org/10.1371/journal.pone.0090314.
Kosmider L, Sobczak A, Fik M, Knysak J, Zaciera M, Kurek J, et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16(10):1319–26. https://doi.org/10.1093/ntr/ntu078.
Brown WH, March J. Aldehyde. Encyclopædia Britannica, inc. 2018. www.birtannica.com. Accessed January 2 2020.
Conklin DJ, Haberzettl P, Lee J, Srivastava S. Environmental aldehydes and cardiovascular disease. In: Bhatnagar, A, editor. Environmental cardiology: pollution and heart disease. London: The Royal Society of Chemistry; 2011. pp. 301–70.
Agency for Toxic Substances & Disease Registry. Toxicological profile for acrolein. 2007. www.atsdr.cdc.gov. Accessed November 8, 2018.
Agency for Toxic Substances & Disease Registry. Medical management guidelines for crotonaldehyde. www.atsdr.cdc.gov. Accessed January 30 2020.
Jaccard G, Djoko DT, Korneliou A, Stabbert R, Belushkin M, Esposito M. Mainstream smoke constituents and in vitro toxicity comparative analysis of 3R4F and 1R6F reference cigarettes. Toxicol Rep. 2019;6:222–31. https://doi.org/10.1016/j.toxrep.2019.02.009.
Bagchi P, Geldner N, de Castro BR, De Jesús VR, Park SK, Blount BC. Crotonaldehyde exposure in U.S. tobacco smokers and nonsmokers: NHANES 2005–2006 and 2011–2012. Environ Res. 2018;163:1–9. https://doi.org/10.1016/j.envres.2018.01.033.
Haussmann HJ. Use of hazard indices for a theoretical evaluation of cigarette smoke composition. Chem Res Toxicol. 2012;25(4):794–810. https://doi.org/10.1021/tx200536w.
Stabbert R, Dempsey R, Diekmann J, Euchenhofer C, Hagemeister T, Haussmann H-J, et al. Studies on the contributions of smoke constituents, individually and in mixtures, in a range of in vitro bioactivity assays. Toxicol in Vitro. 2017;42:222–46. https://doi.org/10.1016/j.tiv.2017.04.003.
Wheat LA, Haberzettl P, Hellmann J, Baba SP, Bertke M, Lee J, et al. Acrolein inhalation prevents vascular endothelial growth factor–induced mobilization of Flk-1+/Sca-1+ cells in mice. Arterioscl Throm Vas. 2011;31(7):1598–606. https://doi.org/10.1161/atvbaha.111.227124.
Conklin DJ, Barski OA, Lesgards J-F, Juvan P, Rezen T, Rozman D, et al. Acrolein consumption induces systemic dyslipidemia and lipoprotein modification. Toxicol Appl Pharmacol. 2010;243(1):1–12. https://doi.org/10.1016/j.taap.2009.12.010.
Srivastava S, Sithu SD, Vladykovskaya E, Haberzettl P, Hoetker DJ, Siddiqui MA, et al. Oral exposure to acrolein exacerbates atherosclerosis in apoE-null mice. Atherosclerosis. 2011;215(2):301–8. https://doi.org/10.1016/j.atherosclerosis.2011.01.001.
Sithu SD, Srivastava S, Siddiqui MA, Vladykovskaya E, Riggs DW, Conklin DJ, et al. Exposure to acrolein by inhalation causes platelet activation. Toxicol Appl Pharmacol. 2010;248(2):100–10. https://doi.org/10.1016/j.taap.2010.07.013.
DeJarnett N, Conklin DJ, Riggs DW, Myers JA, O'Toole TE, Hamzeh I, et al. Acrolein exposure is associated with increased cardiovascular disease risk. J Am Heart Assoc. 2014;3(4):e000934. https://doi.org/10.1161/jaha.114.000934.
Geiss O, Bianchi I, Barrero-Moreno J. Correlation of volatile carbonyl yields emitted by e-cigarettes with the temperature of the heating coil and the perceived sensorial quality of the generated vapours. Int J Hyg Environ Health. 2016;219(3):268–77. https://doi.org/10.1016/j.ijheh.2016.01.004.
Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130(16):1418–36. https://doi.org/10.1161/CIR.0000000000000107.
Antoniewicz L, Brynedal A, Hedman L, Lundbäck M, Bosson JA. Acute effects of electronic cigarette inhalation on the vasculature and the conducting airways. Cardiovasc Toxicol. 2019;19(5):441–50. https://doi.org/10.1007/s12012-019-09516-x.
Espinoza-Derout J, Hasan KM, Shao XM, Jordan MC, Sims C, Lee DL, et al. Chronic intermittent electronic cigarette exposure induces cardiac dysfunction and atherosclerosis in apolipoprotein-E knockout mice. Am J Physiol Heart Circ Physiol. 2019;317(2):H445–h59. https://doi.org/10.1152/ajpheart.00738.2018.
Acknowledgments
The authors thank the University of Louisville Diabetes and Obesity Center for support.
Funding
This work was supported by the National Institutes of Health (ES019217, GM127607, HL122676, HL149351, U54HL120163, T32ES011564) and the University of Louisville School of Medicine Integrated Programs in Biomedical Sciences (IPIBS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflicts of interest in this paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Food and Drug Administration, or the American Heart Association.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mechanisms of Hypertension and Target-Organ Damage
Rights and permissions
About this article
Cite this article
Lynch, J., Jin, L., Richardson, A. et al. Tobacco Smoke and Endothelial Dysfunction: Role of Aldehydes?. Curr Hypertens Rep 22, 73 (2020). https://doi.org/10.1007/s11906-020-01085-7
Published:
DOI: https://doi.org/10.1007/s11906-020-01085-7