Abstract
Purpose
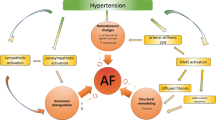
Atrial fibrillation is the most common sustained arrhythmia, with a prevalence of 1–2% in the general population and over 15% in people older than 80 years. Due to aging of the population it imposes an increasing burden on the healthcare system because of the need for life-long pharmacological treatment and the associated increased risk of heart failure and hospitalization. Hence, identification of the factors that predispose to atrial fibrillation it is of utmost relevance.
Recent Findings
Several conditions exist that are characterized by inappropriately high levels of aldosterone, mostly primary aldosteronism and the severe or drug-resistant forms of arterial hypertension. In these forms, aldosterone can cause prominent target organ damage, mostly in the heart, vasculature, and kidney.
Summary
This review examines the experimental data and clinical evidences that support a link between hyperaldosteronism and atrial fibrillation, and how this knowledge should lead to a change in our management of the hypertensive patients presenting with atrial fibrillation.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Seccia TM, Caroccia B, Gomez-Sanchez EP, Gomez-Sanchez CE, Rossi GP. The biology of normal zona glomerulosa and aldosterone-producing adenoma: pathological implications. Endocr Rev. 2018;39:1029–56. This review examines pathophysiology of aldosterone synthesis and deleterious effects of excess aldosterone levels.
Rossi GP, Sechi LA, Giacchetti G, Ronconi V, Strazzullo P, Funder JW. Primary aldosteronism: cardiovascular, renal and metabolic implications. Trends Endocrinol Metab. 2008;19:88–90.
Rossi GP, Belfiore A, Bernini G, Fabris B, Caridi G, Ferri C, et al. Body mass index predicts plasma aldosterone concentrations in overweight-obese primary hypertensive patients. J Clin Endocrinol Metab. 2008;93:2566–71.
Seccia TM, Caroccia B, Muiesan ML, Rossi GP. Atrial fibrillation and arterial hypertension: a common duet with dangerous consequences where the renin angiotensin-aldosterone system plays an important role. Int J Cardiol. 2016;206:71–6.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962.
Post WS, Larson MG, Levy D. Hemodynamic predictors of incident hypertension. The Framingham Heart Study. Hypertension. 1994;24:585–90.
Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82:2N–9N.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Rossi GP, Seccia TM, Pessina AC. Clinical use of laboratory tests for the identification of secondary forms of arterial hypertension. Crit Rev Clin Lab Sci. 2007;44:1–85.
Seccia TM, Caroccia B, Gomez-Sanchez EP, Vanderriele PE, Gomez-Sanchez CE, Rossi GP. Review of markers of zona glomerulosa and aldosterone-producing adenoma cells. Hypertension. 2017;70:867–74.
Bénitah JP, Perrier E, Gómez AM, Vassort G. Effects of aldosterone on transient outward K+ current density in rat ventricular myocytes. J Physiol. 2001;537:151–60.
Gómez AM, Rueda A, Sainte-Marie Y, Pereira L, Zissimopoulos S, Zhu X, et al. Mineralocorticoid modulation of cardiac ryanodine receptor activity is associated with downregulation of FK506-binding proteins. Circulation. 2009;119:2179–87.
Ouvrard-Pascaud A, Sainte-Marie Y, Bénitah J-P, Perrier R, Soukaseum C, Nguyen Dinh Cat A, et al. Conditional mineralocorticoid receptor expression in the heart leads to life-threatening arrhythmias. Circulation. 2005;111:3025–33.
•• Reil J-CC, Hohl M, Selejan S, Lipp P, Drautz F, Kazakow A, et al. Aldosterone promotes atrial fibrillation. Eur Heart J. 2012;33:2098–108. This study first provided in vivo evidence that aldosterone can cause atrial fibrillation. Seccia.
Lammers C, Dartsch T, Brandt MC, Rottländer D, Halbach M, Peinkofer G, et al. Spironolactone prevents aldosterone induced increased duration of atrial fibrillation in rat. Cell Physiol Biochem. 2012;29:833–40.
Rossi GP, Sacchetto A, Visentin P, Canali C, Graniero GR, Palatini P, et al. Changes in left ventricular anatomy and function in hypertension and primary aldosteronism. Hypertension. 1996;27:1039–45.
Rossi GP, Bolognesi M, Rizzoni D, Seccia TM, Piva A, Porteri E, et al. Vascular remodeling and duration of hypertension predict outcome of adrenalectomy in primary aldosteronism patients. Hypertension. 2008;51:1366–71.
Muiesan ML, Rizzoni D, Salvetti M, Porteri E, Monteduro C, Guelfi D, et al. Structural changes in small resistance arteries and left ventricular geometry in patients with primary and secondary hypertension. J Hypertens. 2002;20:1439–44.
Gaddam K, Corros C, Pimenta E, Ahmed M, Denney T, Aban I, et al. Rapid reversal of left ventricular hypertrophy and intracardiac volume overload in patients with resistant hypertension and hyperaldosteronism: a prospective clinical study. Hypertension. 2010;55:1137–42.
Rossi GP, Di Bello V, Ganzaroli C, Sacchetto A, Cesari M, Bertini A, et al. Excess aldosterone is associated with alterations of myocardial texture in primary aldosteronism. Hypertension. 2002;40:23–7.
Rocha R, Stier CT Jr, Kifor I, Ochoa-Maya MR, Rennke HG, Williams GH, et al. Aldosterone: a mediator of myocardial necrosis and renal arteriopathy. Endocrinology. 2000;141:3871–8.
Leask A. Getting to the heart of the matter: new insights into cardiac fibrosis. Circ Res. 2015;116:1269–76.
Yamazaki T, Yazaki Y. Role of tissue angiotensin II in myocardial remodelling induced by mechanical stress. J Hum Hypertens. 1999;13(Suppl 1):S43–7.
Rocha R, Rudolph AE, Frierdich GE, Nachowiak DA, Kekec BK, Blomme EA, et al. Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am J Physiol Heart Circ Physiol. 2002;283:H1802–10.
Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT. Aldosterone-induced inflammation in the rat heart: role of oxidative stress. Am J Pathol. 2002;161:1773–81.
•• Heijman J, Voigt N, Nattel S, Dobrev D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res. 2014;114:1483–99. This comprehensive review examines the molecular mechanisms underlying development and persistence of atrial fibrillation.
Tanaka K, Ashizawa N, Kawano H, Sato O, Seto S, Nishihara E, et al. Aldosterone induces circadian gene expression of clock genes in H9c2 cardiomyoblasts. Heart Vessel. 2007;22:254–60.
Tsai C-F, Yang S-F, Chu H-J, Ueng K-C. Cross-talk between mineralocorticoid receptor/angiotensin II type 1 receptor and mitogen-activated protein kinase pathways underlies aldosterone-induced atrial fibrotic responses in HL-1 cardiomyocytes. Int J Cardiol. 2013;169:17–28.
Lavall D, Selzer C, Schuster P, Lenski M, Adam O, Schäfers H-J, et al. The mineralocorticoid receptor promotes fibrotic remodeling in atrial fibrillation. J Biol Chem. 2014;289:6656–68.
Takemoto Y, Ramirez RJ, Kaur K, Salvador-Montañés O, Ponce-Balbuena D, Ramos-Mondragón R, et al. Eplerenone reduces atrial fibrillation burden without preventing atrial electrical remodeling. J Am Coll Cardiol. 2017;70:2893–905.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. randomized aldactone evaluation study investigators. N Engl J Med. 1999;341:709–17.
Pitt B, White H, Nicolau J, Martinez F, Gheorghiade M, Aschermann M, et al. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46:425–31.
Swedberg K, Zannad F, McMurray JJV, Krum H, Van Veldhuisen DJ, Shi H, et al. Eplerenone and atrial fibrillation in mild systolic heart failure: results from the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure) study. J Am Coll Cardiol. 2012;59:1598–603.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart R. Circulation. 2019;140:e125–51.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension. 2013;62:62–9.
Neefs J, van den Berg NWE, Limpens J, Berger WR, Boekholdt SM, Sanders P, et al. Aldosterone pathway blockade to prevent atrial fibrillation: a systematic review and meta-analysis. Int J Cardiol. 2017;231:155–61.
Liu T, Korantzopoulos P, Shao Q, Zhang Z, Letsas KP, Li G. Mineralocorticoid receptor antagonists and atrial fibrillation: a meta-analysis. Europace. 2016;18:672–8.
Rossi GP, Maiolino G, Flego A, Belfiore A, Bernini G, Fabris B, et al. Adrenalectomy lowers incident atrial fibrillation in primary aldosteronism patients at long term. Hypertension. 2018;71:585–91.This is the largest prospective study with the longest follow-up showing a decrease of incident AF with adrenalectomy.
Seccia TM, Letizia C, Muiesan ML, Lerco S, Cesari M, Bisogni V, et al. Atrial fiibrillation as presenting sign of primary aldosteronism: results of the PAPPHY Study. J Hypertens. 2020;in press.
Rossi GP, Seccia TM, Gallina V, Muiesan ML, Leoni L, Pengo M, et al. Prospective appraisal of the prevalence of primary aldosteronism in hypertensive patients presenting with atrial flutter or fibrillation (PAPPHY study): rationale and study design. J Hum Hypertens. 2013;27:158–63.
Seccia TM, Caroccia B, Adler GK, Maiolino G, Cesari M, Rossi GP. Arterial hypertension, atrial fibrillation, and hyperaldosteronism: the triple trouble. Hypertension. 2017;69:545–50.
Goette A, Hoffmanns P, Enayati W, Meltendorf U, Geller JC, Klein HU. Effect of successful electrical cardioversion on serum aldosterone in patients with persistent atrial fibrillation. Am J Cardiol. 2001;88:906–9.
Dixen U, Ravn L, Soeby-Rasmussen C, Paulsen AW, Parner J, Frandsen E, et al. Raised plasma aldosterone and natriuretic peptides in atrial fibrillation. Cardiology. 2007;108:35–9.
Wozakowska-Kaplon B, Bartkowiak R, Janiszewska G. A decrease in serum aldosterone level is associated with maintenance of sinus rhythm after successful cardioversion of atrial fibrillation. Pacing Clin Electrophysiol. 2010;33:561–5.
Funding
The work was supported by grants from the University of Padova (BIRD163255/16; DOR1842303/18; DOR1743424/17; DOR1625891/16) and grant RF2011-02352318 from the Italian Ministry of Health to TMS and GPR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mechanisms of Hypertension and Target-Organ Damage
Rights and permissions
About this article
Cite this article
Seccia, T.M., Caroccia, B., Maiolino, G. et al. Arterial Hypertension, Aldosterone, and Atrial Fibrillation. Curr Hypertens Rep 21, 94 (2019). https://doi.org/10.1007/s11906-019-1001-4
Published:
DOI: https://doi.org/10.1007/s11906-019-1001-4