Abstract
Purpose of Review
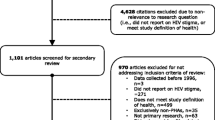
HIV-related stigma remains a significant barrier to engagement in care for persons living with HIV (PLWH) worldwide. This review examines the use of eHealth technologies for reducing stigma as a pathway toward improved engagement in care for PLWH. We provide a brief overview of effective stigma reduction interventions for PLWH, both eHealth and others; identify gaps in the research on use of eHealth technologies for stigma reduction; and suggest potential research avenues moving forward.
Recent Findings
The majority of HIV-related eHealth studies use technology to improve ART adherence. To date, few HIV-related eHealth studies have included any measurement of stigma.
Summary
Given the current narrow evidence base, further research is needed to determine whether eHealth technologies can help to reduce stigma and improve engagement in care for PLWH.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Joint United Nations Programme on HIV/AIDS. 90–90-90: An ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS. 2014.
Link BG. Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. Am Sociol Rev. 1987;52:96–112.
Knettel BA, Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, et al. Retention in HIV care during pregnancy and the postpartum period in the option B+ era: a systematic review and meta-analysis of studies in Africa. J Acquir Immune Defic Syndr. 2017;77:427–38. https://doi.org/10.1097/qai.0000000000001616.
Kempf MC, McLeod J, Boehme AK, Walcott MW, Wright L, Seal P, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: implications for targeted interventions. AIDS Patient Care STDs. 2010;24(8):515–20. https://doi.org/10.1089/apc.2010.0065.
Rao D, Feldman B, Fredericksen R, Crane P, Simoni J, Kitahata M et al. A Structural Equation Model of HIV-Related Stigma, Depressive Symptoms, and Medication Adherence. AIDS and Behavior. 2011;epub ahead of print.
Grossman CI, Stangl AL. Editorial: global action to reduce HIV stigma and discrimination. J Int AIDS Soc. 2013;16(3 Suppl 2):18881. https://doi.org/10.7448/ias.16.3.18881.
Eng TR. The eHealth landscape: a terrain map of emerging information and communication technologies in health and health care. 2001.
Waters AJ, Miller EK, Li Y. Administering the implicit association test in an ecological momentary assessment study. Psychol Rep. 2010;106(1):31–43. https://doi.org/10.2466/pr0.106.1.31-43.
• Rao D, Molina Y, Lambert N, Cohn SE. Assessing stigma among African Americans living with HIV. Stigma and Health. 2016;1(3):146–55. https://doi.org/10.1037/sah0000027. Though stigma has been identified as a barrier to treatment engagement in African American PLWH, few studies have sought to develop or adapt culturally relevant measures of stigma for this high-risk and understudied group. This study is among the first to culturally adapt and validate a brief measure of internalized and enacted stigma in African American PLWH, with the goal of informing future interventions in this population.
Yah CS, Tambo E, Khayeka-Wandabwa C, Ngogang JY. Impact of telemonitoring approaches on integrated HIV and TB diagnosis and treatment interventions in sub-Saharan Africa: a scoping review. Health Promotion Perspect. 2017;7(2):60–5. https://doi.org/10.15171/hpp.2017.12.
Mboya B, Temu F, Awadhi B, Ngware Z, Ndyetabura E, Kiondo G et al. Access to HIV prevention services among gender based violence survivors in Tanzania. Pan Afr Med J. 2012;13 Suppl 1:5.
Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69.
Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. Mental health-related stigma in health care and mental health-care settings. The Lancet Psychiatry. 2014;1(6):467–82.
•• Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet. 2016;387(10023):1123–32. This narrative review provides a crucial window into interventions targeting reduction in mental-illness-related stigma and discrimination worldwide. Key findings include (1) clear short-term benefits of contact-based interventions; (2) weak evidence for longer-term benefits of stigma reduction initatives; and (3) few studies on intervention development and evaluation in low resource settings.
Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv. 2012;63(10):963–73.
Corrigan P. Best practices: strategic stigma change (SSC): five principles for social marketing campaigns to reduce stigma. Psychiatr Serv. 2011;62(8):824–6.
Rao D, Desmond M, Andrasik M, Rasberry T, Lambert N, Cohn S, et al. Feasibility, acceptability, and preliminary efficacy of the ‘Unity workshop’: an internalized stigma reduction intervention for African-American women living with HIV. AIDS Patient Care & STDs. 2012;26(10):614–20.
Kemp C, Simoni J, Turan J, Cohn S, Nevin P, Lipira L et al., Editors. Social support and HIV stigma are associated with subsequent viral load and viral suppression among African American women living with HIV: an exploratory longitudinal analysis. 13th international AIDS impact conference; 2017; Cape Town, South Africa.
•• Rao D, Kemp C, Huh D, Nevin P, Turan J, Cohn S et al. (In Press). Stigma Reduction Among African American Women with HIV: UNITY Health Study. JAIDS; 2017. This study presents the primary outcome findings of the UNITY health study, which investigated stigma reduction among African American women with HIV. Findings suggested that social support and contact were a key mechanisms for reduction of stigma in this population.
Aronson E, Wilson T, Akert R. Social psychology. Pearson Education: Upper Saddle River, NJ; 2005.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. https://doi.org/10.7448/ias.16.3.18640.
McDoom MM, Bokhour B, Sullivan M, Drainoni ML. How older black women perceive the effects of stigma and social support on engagement in HIV care. AIDS Patient Care STDs. 2015;29(2):95–101. https://doi.org/10.1089/apc.2014.0184.
Churcher S. Stigma related to HIV and AIDS as a barrier to accessing health care in Thailand: a review of recent literature. WHO South-East Asia J Public Health. 2013;2(1):12–22. https://doi.org/10.4103/2224-3151.115829.
Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, et al. Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. J Int AIDS Soc. 2014;17(4 Suppl 3):19618. https://doi.org/10.7448/ias.17.4.19618.
• Treves-Kagan S, Steward WT, Ntswane L, Haller R, Gilvydis JM, Gulati H, et al. Why increasing availability of ART is not enough: a rapid, community-based study on how HIV-related stigma impacts engagement to care in rural South Africa. BMC Public Health. 2016;16:87. https://doi.org/10.1186/s12889-016-2753-2. South Africa provides a unique context to examine efforts to reduce HIV-related morbidity and mortality in LMICs. Though the country boasts the world’s largest antiretroviral program and has successfully integrated HIV testing and treatment into primary care settings, less than half of PLWH remain unaware of their status, and only half of eligible clients are on ART. This key study uses qualitative methods with a robust sample size (N = 684) to directly assess stigma’s role in maintaining the HIV epidemic throughout the country.
• Lyons CE, Ketende S, Diouf D, Drame FM, Liestman B, Coly K, et al. Potential Impact of Integrated Stigma Mitigation Interventions in Improving HIV/AIDS Service Delivery and Uptake for Key Populations in Senegal. J Acquir Immune Defic Syndr. 2017;74(Suppl 1):S52–s9. https://doi.org/10.1097/qai.0000000000001209. This study represents one of few efforts to design and deploy stigma reduction interventions for PLWH in resource-constrained LMICs. This pilot evaluation trial is especially notable due to its tailoring of a stigma reduction intervention for key populations (i.e., men who have sex with men and female sex workers) with comparatively high HIV burdens.
White M, Dorman SM. Receiving social support online: implications for health education. Health Educ Res. 2001;16(6):693–707.
Bartolo A, Pacheco E, Rodrigues F, Pereira A, Monteiro S, Santos IM. Effectiveness of psycho-educational interventions with telecommunication technologies on emotional distress and quality of life of adult cancer patients: a systematic review. Disabil Rehabil. 2017:1–9. https://doi.org/10.1080/09638288.2017.1411534.
Andersson G, Carlbring P. Internet-assisted cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):689–700. https://doi.org/10.1016/j.psc.2017.08.004.
•• Amico KR. Evidence for Technology Interventions to Promote ART Adherence in Adult Populations: a Review of the Literature 2012–2015. Curr HIV/AIDS Rep. 2015;12(4):441–50. https://doi.org/10.1007/s11904-015-0286-4. This brief and important summary synthesizes a large body of recent research (i.e., between 2013 and 2015) on technology-assisted ART promotion interventions for adult PLWH.
• Radhakrishna K, Dass D, Raj T, Rakesh D, Kishore R, Srinivasan K, et al. Development of a novel tablet-based approach to reduce HIV stigma among healthcare staff in India. Perspect Health Inf Manag. 2017;14(spring):1b. This India-based study highlights the development of a tablet-based stigma reduction intervention for improving provider attitudes towards PLWH. It is one of few documented interventions that include stigma as a primary target and outcome.
Lipira L, Nevin P, Frey S, Velonjara J, Endeshaw M, Kumar S et al. The Positive Living Program: Development and pilot evaluation of a multimedia behavioral intervention to address HIV-related stigma and depression among African-immigrant PLWH in King County, WA. . Under Review. 2017.
Simoni JM, Kutner BA, Horvath KJ, Yang JP, Chen WT, Shiu CS, et al. A computer-based program to promote art adherence, mental health, and treatment engagement among PLWHA in China: development and initial acceptability. In: Poster (#49) presented at the 11th international conference on HIV treatment and prevention adherence. Fort: Lauderdale, FL; 2016.
Anand T, Nitpolprasert C, Kerr SJ, Muessig KE, Promthong S, Chomchey N, et al. A qualitative study of Thai HIV-positive young men who have sex with men and transgender women demonstrates the need for eHealth interventions to optimize the HIV care continuum. AIDS Care. 2017;29(7):870–5. https://doi.org/10.1080/09540121.2017.1286288.
Schnall R, Bakken S, Rojas M, Travers J, Carballo-Dieguez A. mHealth Technology as a Persuasive Tool for Treatment, Care and Management of Persons Living with HIV. AIDS and Behavior. 2015;19(Supplement 2):81–9. https://doi.org/10.1007/s10461-014-0984-8.
Schnall R, Cho H, Webel A. Predictors of willingness to use a smartphone for research in underserved persons living with HIV. Int J Med Inform. 2017;99:53–9. https://doi.org/10.1016/j.ijmedinf.2017.01.002.
• Reynolds NR, Satyanarayana V, Duggal M, Varghese M, Liberti L, Singh P, et al. MAHILA: a protocol for evaluating a nurse-delivered mHealth intervention for women with HIV and psychosocial risk factors in India. BMC Health Serv Res. 2016;16(a):352. https://doi.org/10.1186/s12913-016-1605-1. This study is novel in its (1) use of lay or non-specialist providers (in this instance, nurses) to deliver a mobile phone-based adherence intervention for PLWH in India; and (2) measurement of stigma as a secondary analytic outcome.
Mao L, Buchanan A, Wong HTH, Persson A. Beyond mere pill taking: SMS reminders for HIV treatment adherence delivered to mobile phones of clients in a community support network in Australia. Health Soc Care Community. 2018;26:486–94. https://doi.org/10.1111/hsc.12544.
Turkle S. Alone together: why we expect more from technology and less from each other. New York: Basic Books; 2011.
•• Turkle S. Reclaiming Conversation: The Power of Talk in a Digital Age. New York: Penguin; 2015. Turkle, a leading psychologist directing current discourse on technology, provides a critical reflection on the intersections of technology, identity, and human empathy in her latest book.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on HIV and Technology
Rights and permissions
About this article
Cite this article
Rao, D., Frey, S. & Ramaiya, M. eHealth for Stigma Reduction Efforts Designed to Improve Engagement in Care for People Living with HIV. Curr HIV/AIDS Rep 15, 397–402 (2018). https://doi.org/10.1007/s11904-018-0414-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-018-0414-z