Abstract
Purpose of Review
Decompensated cirrhosis and liver failure result in high mortality risk. Identifying the severity of illness and risk of poor outcomes is important for improved clinical decision making. This review serves to examine the currently in practice and developing tools for prognosticating patients with cirrhosis.
Recent Findings
The Child–Turcotte–Pugh (CTP) score and Model for End-Stage Liver Disease (MELD) score are the most used prognostic tools for cirrhotic patients. More recently, however, are newly developing biochemical models and imaging tools that strive to improve upon the MELD score.
Summary
Significant effort has been dedicated to revising, complementing, or replacing the MELD score for prognostication and for transplant allocation. Ongoing adjustment to current prognostication methods and the search for new paradigms promises improved ability to predict outcomes and determine the best management in the future.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• McPherson S, Lucey MR, Moriarty KJ. Decompensated alcohol related liver disease: acute management. BMJ. 2016;352:i124. https://doi.org/10.1136/bmj.i124 Management of patients with alcohol cirrhosis and acute liver failure.
Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1–85.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–9.
Brown RS Jr, Kumar KS, Russo MW, Kinkhabwala M, Rudow DL, Harren P, et al. Model for end-stage liver disease and Child-Turcotte-Pugh score as predictors of pretransplantation disease severity, posttransplantation outcome, and resource utilization in United Network for Organ Sharing status 2A patients. Liver Transpl. 2002;8(3):278–84. https://doi.org/10.1053/jlts.2002.31340.
Kim HJ, Lee HW. Important predictor of mortality in patients with end-stage liver disease. Clin Mol Hepatol. 2013;19(2):105–15. https://doi.org/10.3350/cmh.2013.19.2.105.
Robert A, Chazouilleres O. Prothrombin time in liver failure: time, ratio, activity percentage, or international normalized ratio? Hepatology. 1996;24(6):1392–4. https://doi.org/10.1053/jhep.1996.v24.pm0008938167.
Abad-Lacruz A, Cabre E, Gonzalez-Huix F, Fernandez-Banares F, Esteve M, Planas R, et al. Routine tests of renal function, alcoholism, and nutrition improve the prognostic accuracy of Child-Pugh score in nonbleeding advanced cirrhotics. Am J Gastroenterol. 1993;88(3):382–7.
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31(4):864–71. https://doi.org/10.1053/he.2000.5852.
Singal AK, Kamath PS. Model for end-stage liver disease. J Clin Exp Hepatol. 2013;3(1):50–60. https://doi.org/10.1016/j.jceh.2012.11.002.
• Ascha M, Hanouneh MSA, Zein NN, Sands M, Lopez R, et al. Transjugular intrahepatic porto-systemic shunt in patients with liver cirrhosis and model for end-stage liver disease >/=15. Dig dis Sci. 2017;62(2):534–42. https://doi.org/10.1007/s10620-016-4185-3 Addresses safety of TIPS in high MELD patients.
Kim SH, Han YD, Lee JG, Kim DY, Choi SB, Choi GH, et al. MELD-based indices as predictors of mortality in chronic liver disease patients who undergo emergency surgery with general anesthesia. J Gastrointest Surg. 2011;15(11):2029–35. https://doi.org/10.1007/s11605-011-1669-5.
Gish RG. Do we need to MEND the MELD? Liver Transpl. 2007;13(4):486–7. https://doi.org/10.1002/lt.21040.
Asrani SK, Kim WR. Model for end-stage liver disease: end of the first decade. Clin Liver Dis. 2011;15(4):685–98. https://doi.org/10.1016/j.cld.2011.08.009.
Cholongitas E, Marelli L, Kerry A, Senzolo M, Goodier DW, Nair D, et al. Different methods of creatinine measurement significantly affect MELD scores. Liver Transpl. 2007;13(4):523–9. https://doi.org/10.1002/lt.20994.
Cirillo M, Anastasio P, De Santo NG. Relationship of gender, age, and body mass index to errors in predicted kidney function. Nephrol Dial Transplant. 2005;20(9):1791–8. https://doi.org/10.1093/ndt/gfh962.
Trotter JF, Olson J, Lefkowitz J, Smith AD, Arjal R, Kenison J. Changes in international normalized ratio (INR) and model for endstage liver disease (MELD) based on selection of clinical laboratory. Am J Transplant. 2007;7(6):1624–8. https://doi.org/10.1111/j.1600-6143.2007.01822.x.
•• Joel P, Wedd AK, Biggins SW. Predictors of clinical complications in cirrhosis. In: springer, editor. Complications of Cirrhosis: Switzerland Springer International; 2015. Critical review of existing prognostic paradigms that predict mortality in cirrhosis.
Somsouk M, Kornfield R, Vittinghoff E, Inadomi JM, Biggins SW. Moderate ascites identifies patients with low model for end-stage liver disease scores awaiting liver transplantation who have a high mortality risk. Liver Transpl. 2011;17(2):129–36. https://doi.org/10.1002/lt.22218.
Heuman DM, Abou-Assi SG, Habib A, Williams LM, Stravitz RT, Sanyal AJ, et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology. 2004;40(4):802–10. https://doi.org/10.1002/hep.20405.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–6. https://doi.org/10.1053/gast.2003.50016.
Cholongitas E, Papatheodoridis GV, Vangeli M, Terreni N, Patch D, Burroughs AK. Systematic review: the model for end-stage liver disease--should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22(11–12):1079–89. https://doi.org/10.1111/j.1365-2036.2005.02691.x.
•• Roth JA, Chrobak C, Schadelin S, Hug BL. MELD score as a predictor of mortality, length of hospital stay, and disease burden: a single-center retrospective study in 39,323 inpatients. Medicine (Baltimore). 2017;96(24):e7155. https://doi.org/10.1097/MD.0000000000007155 Large retrospective analysis of MELD as a predictor of outcomes in patients with cirrhosis.
Zhang M, Yin F, Chen B, Li YP, Yan LN, Wen TF, et al. Pretransplant prediction of posttransplant survival for liver recipients with benign end-stage liver diseases: a nonlinear model. PLoS One. 2012;7(3):e31256. https://doi.org/10.1371/journal.pone.0031256.
Serste T, Gustot T, Rautou PE, Francoz C, Njimi H, Durand F, et al. Severe hyponatremia is a better predictor of mortality than MELDNa in patients with cirrhosis and refractory ascites. J Hepatol. 2012;57(2):274–80. https://doi.org/10.1016/j.jhep.2012.03.018.
Moini M, Hoseini-Asl MK, Taghavi SA, Sagheb MM, Nikeghbalian S, Salahi H, et al. Hyponatremia a valuable predictor of early mortality in patients with cirrhosis listed for liver transplantation. Clin Transpl. 2011;25(4):638–45. https://doi.org/10.1111/j.1399-0012.2010.01350.x.
Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018–26. https://doi.org/10.1056/NEJMoa0801209.
Barber K, Madden S, Allen J, Collett D, Neuberger J, Gimson A, et al. Elective liver transplant list mortality: development of a United Kingdom end-stage liver disease score. Transplantation. 2011;92(4):469–76. https://doi.org/10.1097/TP.0b013e318225db4d.
Leise MD, Kim WR, Kremers WK, Larson JJ, Benson JT, Therneau TM. A revised model for end-stage liver disease optimizes prediction of mortality among patients awaiting liver transplantation. Gastroenterology. 2011;140(7):1952–60. https://doi.org/10.1053/j.gastro.2011.02.017.
Sharma P, Schaubel DE, Sima CS, Merion RM, Lok AS. Re-weighting the model for end-stage liver disease score components. Gastroenterology. 2008;135(5):1575–81. https://doi.org/10.1053/j.gastro.2008.08.004.
•• Organ Procurement and Transplantation Network. 2018. Existing guidelines and regulations for organ procurement and transplant.
Huo TI, Wang YW, Yang YY, Lin HC, Lee PC, Hou MC, et al. Model for end-stage liver disease score to serum sodium ratio index as a prognostic predictor and its correlation with portal pressure in patients with liver cirrhosis. Liver Int. 2007;27(4):498–506. https://doi.org/10.1111/j.1478-3231.2007.01445.x.
Heuman DM, Mihas AA, Habib A, Gilles HS, Stravitz RT, Sanyal AJ, et al. MELD-XI: a rational approach to “sickest first” liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liver Transpl. 2007;13(1):30–7. https://doi.org/10.1002/lt.20906.
Magder LS, Regev A, Mindikoglu AL. Comparison of seven liver allocation models with respect to lives saved among patients on the liver transplant waiting list. Transpl Int. 2012;25(4):409–15. https://doi.org/10.1111/j.1432-2277.2012.01431.x.
Albilllos A, Garcia-Tsao G. Classification of cirrhosis: the clinical use of HVPG measurements. Dis Markers. 2011;31(3):121–8. https://doi.org/10.3233/DMA-2011-0834.
Suk KT, Kim CH, Park SH, Sung HT, Choi JY, Han KH, et al. Comparison of hepatic venous pressure gradient and two models of end-stage liver disease for predicting the survival in patients with decompensated liver cirrhosis. J Clin Gastroenterol. 2012;46(10):880–6. https://doi.org/10.1097/MCG.0b013e31825f2622.
Pachta E, Hucke F, Weiss S, Popp S, Haupt L, Peck-Radosavljevic M, et al. Prognostic impact of the BAVENO IV staging system of portal hypertension in patients with cirrhosis and hepatocellular carcinoma. Gastroenterology. 2014;2014:52–P72.
D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–31. https://doi.org/10.1016/j.jhep.2005.10.013.
D'Amico G, Pasta L, Morabito A, D'Amico M, Caltagirone M, Malizia G, et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39(10):1180–93. https://doi.org/10.1111/apt.12721.
Wedd J, Bambha KM, Stotts M, Laskey H, Colmenero J, Gralla J, et al. Stage of cirrhosis predicts the risk of liver-related death in patients with low model for end-stage liver disease scores and cirrhosis awaiting liver transplantation. Liver Transpl. 2014;20(10):1193–201. https://doi.org/10.1002/lt.23929.
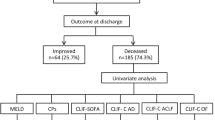
•• Piton G, Chaignat C, Giabicani M, Cervoni JP, Tamion F, Weiss E, et al. Prognosis of cirrhotic patients admitted to the general ICU. Ann Intensive Care. 2016;6(1):94. https://doi.org/10.1186/s13613-016-0194-9 Use of existing predictors for patients with cirrhosis in intensive care units.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Pan HC, Jenq CC, Tsai MH, Fan PC, Chang CH, Chang MY, et al. Scoring systems for 6-month mortality in critically ill cirrhotic patients: a prospective analysis of chronic liver failure - sequential organ failure assessment score (CLIF-SOFA). Aliment Pharmacol Ther. 2014;40(9):1056–65. https://doi.org/10.1111/apt.12953.
•• Sy E, Ronco JJ, Searle R, Karvellas CJ. Prognostication of critically ill patients with acute-on-chronic liver failure using the chronic liver failure-sequential organ failure assessment: a Canadian retrospective study. J Crit Care. 2016;36:234–9. https://doi.org/10.1016/j.jcrc.2016.08.003 Clarification of an existing predictor in critically ill intensive care unit patients.
Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–37, 37 e1–9. https://doi.org/10.1053/j.gastro.2013.02.042.
Jalan R, Saliba F, Pavesi M, Amoros A, Moreau R, Gines P, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol. 2014;61(5):1038–47. https://doi.org/10.1016/j.jhep.2014.06.012.
•• Hernaez R, Sola E, Moreau R, Gines P. Acute-on-chronic liver failure: an update. Gut. 2017;66(3):541–53. https://doi.org/10.1136/gutjnl-2016-312670 Acute-on-chronic liver failure in cirrhotic patients in intensive care units.
• Patil AG, Bihari C, Shewade HD, Nigam N, Sarin SK. Decreased protein C function predicts mortality in patients with cirrhosis. Int J Lab Hematol. 2018;40(4):466–72. https://doi.org/10.1111/ijlh.12836 Use of protein C as a developing prognotic test for patients with cirrhosis.
Tripodi A, Anstee QM, Sogaard KK, Primignani M, Valla DC. Hypercoagulability in cirrhosis: causes and consequences. J Thromb Haemost. 2011;9(9):1713–23. https://doi.org/10.1111/j.1538-7836.2011.04429.x.
Adachi M, Tanaka A, Aiso M, Takamori Y, Takikawa H. Benefit of cystatin C in evaluation of renal function and prediction of survival in patients with cirrhosis. Hepatol Res. 2015;45(13):1299–306. https://doi.org/10.1111/hepr.12508.
• Maiwall R, Kumar A, Bhardwaj A, Kumar G, Bhadoria AS, Sarin SK. Cystatin C predicts acute kidney injury and mortality in cirrhotics: a prospective cohort study. Liver Int. 2018;38(4):654–64. https://doi.org/10.1111/liv.13600 Use of cytostatin C as a developing prognostic test in patients with cirrhosis.
• Elalfy H, Besheer T, El-Maksoud MA, Farid K, Elegezy M, El Nakib AM, et al. Monocyte/granulocyte to lymphocyte ratio and the MELD score as prognostic predictors for early recurrence of hepatocellular carcinoma after trans-arterial chemoembolization. Br J Biomed Sci. 2018; Use of monocyte/granulocyte to lymphocyte ratio as a developing prognostic test in patients with cirrhosis as compared to MELD.
Biyik M, Ucar R, Solak Y, Gungor G, Polat I, Gaipov A, et al. Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2013;25(4):435–41. https://doi.org/10.1097/MEG.0b013e32835c2af3.
•• Kalra A, Wedd JP, Bambha KM, Gralla J, Golden-Mason L, Collins C, et al. Neutrophil-to-lymphocyte ratio correlates with proinflammatory neutrophils and predicts death in low model for end-stage liver disease patients with cirrhosis. Liver Transpl. 2017;23(2):155–65. https://doi.org/10.1002/lt.24702 Neutrophil-to-lymphocyte ratio predicts mortality in low MELD patients.
• Leithead JA, Rajoriya N, Gunson BK, Ferguson JW. Neutrophil-to-lymphocyte ratio predicts mortality in patients listed for liver transplantation. Liver Int. 2015;35(2):502–9. https://doi.org/10.1111/liv.12688 Neutrophil-to-lymphocyte ratio as a prognostic indicator in patients awaiting liver transplant.
Picard D, Infante-Rivard C, Villeneuve JP, Chartrand R, Picard M, Carrier L. Extrahepatic uptake of technetium-99m-phytate: a prognostic index in patients with cirrhosis. J Nucl Med. 1990;31(4):436–40.
Horisawa M, Goldstein G, Waxman A, Reynolds T. The abnormal hepatic scan of chronic liver disease: its relationship to hepatic hemodynamics and colloid extraction. Gastroenterology. 1976;71(2):210–3.
Merle U, Sieg O, Stremmel W, Encke J, Eisenbach C. Sensitivity and specificity of plasma disappearance rate of indocyanine green as a prognostic indicator in acute liver failure. BMC Gastroenterol. 2009;9:91. https://doi.org/10.1186/1471-230X-9-91.
Gupta S, Chawla Y, Kaur J, Saxena R, Duseja A, Dhiman RK, et al. Indocyanine green clearance test (using spectrophotometry) and its correlation with model for end stage liver disease (MELD) score in Indian patients with cirrhosis of liver. Trop Gastroenterol. 2012;33(2):129–34.
Zipprich A, Kuss O, Rogowski S, Kleber G, Lotterer E, Seufferlein T, et al. Incorporating indocyanin green clearance into the model for end stage liver disease (MELD-ICG) improves prognostic accuracy in intermediate to advanced cirrhosis. Gut. 2010;59(7):963–8. https://doi.org/10.1136/gut.2010.208595.
Stauber RE, Wagner D, Stadlbauer V, Palma S, Gurakuqi G, Kniepeiss D, et al. Evaluation of indocyanine green clearance and model for end-stage liver disease for estimation of short-term prognosis in decompensated cirrhosis. Liver Int. 2009;29(10):1516–20. https://doi.org/10.1111/j.1478-3231.2009.02104.x.
Helmke S, Colmenero J, Everson GT. Noninvasive assessment of liver function. Curr Opin Gastroenterol. 2015;31(3):199–208. https://doi.org/10.1097/MOG.0000000000000167.
Everson GT, Shiffman ML, Hoefs JC, Morgan TR, Sterling RK, Wagner DA, et al. Quantitative liver function tests improve the prediction of clinical outcomes in chronic hepatitis C: results from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology. 2012;55(4):1019–29. https://doi.org/10.1002/hep.24752.
Hanai T, Shiraki M, Nishimura K, Ohnishi S, Imai K, Suetsugu A, et al. Sarcopenia impairs prognosis of patients with liver cirrhosis. Nutrition. 2015;31(1):193–9. https://doi.org/10.1016/j.nut.2014.07.005.
•• Gu DH, Kim MY, Seo YS, Kim SG, Lee HA, Kim TH, et al. Clinical usefulness of psoas muscle thickness for the diagnosis of sarcopenia in patients with liver cirrhosis. Clin Mol Hepatol. 2018. https://doi.org/10.3350/cmh.2017.0077 Sarcopenia to predict outcomes in patients with cirrhosis.
•• Dunn MA, Josbeno DA, Tevar AD, Rachakonda V, Ganesh SR, Schmotzer AR, et al. Frailty as tested by gait speed is an independent risk factor for cirrhosis complications that require hospitalization. Am J Gastroenterol. 2016;111(12):1768–75. https://doi.org/10.1038/ajg.2016.336 Gait speed as a clinical prognostic indicator of outcomes in cirrhosis.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–63.
•• Laube R, Wang H, Park L, Heyman JK, Vidot H, Majumdar A, et al. Frailty in advanced liver disease. Liver Int. 2018. https://doi.org/10.1111/liv.13917 Frailty as an outcome predictor in patients with cirrhosis.
•• Tandon P, Tangri N, Thomas L, Zenith L, Shaikh T, Carbonneau M, et al. A rapid bedside screen to predict unplanned hospitalization and death in outpatients with cirrhosis: a prospective evaluation of the clinical frailty scale. Am J Gastroenterol. 2016;111(12):1759–67. https://doi.org/10.1038/ajg.2016.303 Development of a frailty scale that can be used in clinical practice to predict outcomes in cirrhosis.
Carey EJ, Steidley DE, Aqel BA, Byrne TJ, Mekeel KL, Rakela J, et al. Six-minute walk distance predicts mortality in liver transplant candidates. Liver Transpl. 2010;16(12):1373–8. https://doi.org/10.1002/lt.22167.
Lai JC, Feng S, Terrault NA, Lizaola B, Hayssen H, Covinsky K. Frailty predicts waitlist mortality in liver transplant candidates. Am J Transplant. 2014;14(8):1870–9. https://doi.org/10.1111/ajt.12762.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Joel Wedd and Kavitha Nair each declare no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Management of Cirrhotic Patient
Rights and permissions
About this article
Cite this article
Wedd, J., Nair, K. Predicting Future Complications of Cirrhosis. Curr Hepatology Rep 18, 9–19 (2019). https://doi.org/10.1007/s11901-019-00445-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-019-00445-5