Abstract
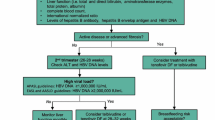
Hepatitis B in pregnancy must include diagnosis and management of the pregnant woman as well as modalities to decrease mother to child transmission (MTCT). MTCT remains the most important mode of hepatitis B virus (HBV) transmission, although effective strategies exist to reduce this risk. Universal screening for HBV can identify women with previously unrecognized infection and allow for targeted therapy to prevent MTCT. All children of HBV-infected mothers should receive passive active immunoprophylaxis with hepatitis B immune globulin (HBIG) and HBV vaccination within 12 h of birth. With such measures, the risk of transmission can be decreased to less than 1 % in women with low viral loads. Immunoprophylaxis failures occur in as many as 15 % of children born to mothers with high viral loads at the time of delivery (>6 log copies/ml or >200,000 IU/ml), and therefore, additional treatment in the third trimester is warranted in this group. Antiviral therapy with lamivudine, tenofovir, or telbivudine in the third trimester can decrease MTCT to less than 5 % and should be used in women with high viral loads in the third trimester. Postpartum flares of liver disease are common, and therefore, careful monitoring is warranted in women who stop therapy. The decision to breastfeed while on antiviral therapy should be individualized, but current evidence suggests that it is safe.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zhang Y, Fang W, Fan L, Gao X, Guo Y, Huang W, et al. Hepatitis B surface antigen prevalence among 12393 rural women of childbearing age in Hainan Province, China: a cross-sectional study. Virol J. 2013;10:25.
Beasley RP, Hwang LY, Lee GC, et al. Prevention of perinatally transmitted hepatitis B virus infections with hepatitis B virus infections with hepatitis B immune globulin and hepatitis B vaccine. Lancet. 1983;2:1099–102.
Lee C, Gong Y, Brok J, Boxall EH, Gluud C. Effect of hepatitis B immunisation in newborn infants of mothers positive for hepatitis B surface antigen: systematic review and meta-analysis. BMJ. 2006;332:328–36.
Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:1–36.
Antiretroviral Pregnancy Registry Steering Committee. Interim report. December 2014. 05 03 2015 <http://www.APRegistry.com>.
Centers for Disease Control and Prevention. Metropolitan Atlanta Congenital Defects Program 6-digit code defect list. To access an electronic copy of the code list, go to http://www.cdc.gov/ncbddd/birthdefects/MACDP.html.
Correa-Villasenor A, Cragan J, Kucik J, O’Leary L, Siffel C, Williams L. The Metropolitan Atlanta Congenital Defects Program: 35 years of birth defects surveillance at the Centers for Disease Control and Prevention. Birth Defects Res Part A. 2003;67:617–24.
Correa A, Cragan J, Kucik J, et al. Metropolitan Atlanta Congenital Defects Program 40th Anniversary Edition Surveillance Report: reporting birth defects surveillance data 1968–2003. Birth Defects Res Part A. 2007;79:65–93. Erratum: 2008;82:41–62.
Riehle-Colarusso T, Strickland MJ, Reller MD, Mahle WT, Botto LD, Siffel C, et al. Improving the quality of surveillance data on congenital heart defects in the Metropolitan Atlanta Congenital Defects Program. Birth Defects Res A Clin Mol Teratol. 2007;79:743–53.
Texas Birth Defect Surveillance System. Report of birth defects among 2000–2009 deliveries. Birth Defects Epidemiology & Surveillance, Texas Department of State Health Services. Published February 2012. Available from URL: http://www.dshs.state.tx.us/birthdefects/data/BD_Data_00-09/Report-of-Birth-Defects-Among-2000---2009-Deliveries.
Wang L, Koutis A, Elington S, Legardy-Williams J, Bulterys M. Safety of tenofovir during pregnancy for the mother and fetus: a systematic review. Clin Infect Dis. 2013;57:1773–81.
Tarantal AF, Castillo A, Ekert JE, Bischofberger N, Martin RB. Fetal and maternal outcome after administration of tenofovir to gravid rhesus monkeys. J Aquir Immune Defic Syndr. 2002;29:207–20.
Tarantal AF, Marthas ML, Shaw JP, Cundy K, Bischofberger N. Administration of 9-[2-(R)-(phosphonomethoxy) propyl]adenine (PMPA) to gravid and infant rehesus macaques(Macca mulatta): safety and efficacy studies. J Acquir Defic Syndr Hum Retroviro. 2000;20:323–33.
Van Rompay KK, Brignolo LL, Meyer DJ, et al. Biological effects of short-term or prolonged administration of 9-[2-(R)-(phosphonomethoxy) propyl]adenine (tenofovir) to newborn and infant rhesus macaques. Antimicrob Agents Chemother. 2004;48:1467–87.
Nurutdinova D, Onen NF, Hayes E, Mondy K, Overton ET. Adverse effects of tenofovir use in HIV-infected pregnant women and their infants. Ann Pharmacother. 2008;42:1581–5.
Vigano A, Mora S, Giacomet V, et al. In utero exposure to tenofovir disoproxil fumarate does not impair growth and bone health in HIV-uninfected children born to HIV-infected mothers. Antivir Ther. 2011;16:1259–66.
Silberry GK, Williams PL, Mendez H, et al. Safety of tenofovir use during pregnancy: early growth outcomes in HIV-exposed uninfected infants. AIDS. 2012;26(9):1151–9.
Zeng H, Cai H, Wang Y, Shen Y. Growth and development of children perinatally exposed to telbivudine administered for the treatment of chronic hepatitis B in their mothers. Int J Infect Dis. 2015;33:e97–101.
European Association for the Study of the Liver. EASL clinical practice guidelines: management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–85.
Burrows RF, Kelton JG. Thrombocytopenia at delivery: a prospective survey of 6,715 deliveries. Am J Obstet Gynecol. 1990;162:731–4.
Kim HY, Choi JY, Park CH, Jang JW, Kim CW, Bae SH, et al. Outcomes after discontinuing antiviral agents during pregnancy in women infected with hepatitis B virus. J Clin Virol. 2013;56:299–305.
Chen Y, Wang L, Xu Y, Liu X, Li S, Qian Q, et al. Role of maternal viremia and placental infection in hepatitis B virus intrauterine transmission. Microbes Infect. 2013;15:409–15.
Lin HH, Lee TY, Chen DS, Sung JL, Ohto H, Etoh T, et al. Transplacental leakage of HBeAg-positive maternal blood as the most likely route in causing intrauterine infection with hepatitis B virus. J Pediatr. 1987;111:877e881.
Lucifora G, Calabro S, Carroccio G, Brigandi A. Immunocytochemical HBsAg evidence in placentas of asymptomatic carrier mothers. Am J Obstet Gynecol. 1988;159:839e842.
Bhat P, Anderson DA. Hepatitis B virus translocates across a trophoblastic barrier. J Virol. 2007;81:7200e7207.
Elefsiniotis S, Tsoumakas K, Papadakis M, Vlachos G, Saroglou G, Antsaklis A. Importance of maternal and cord blood viremia in pregnant women with chronic hepatitis B virus infection. Eur J Intern Med. 2011;22:182e186.
Lopez M, Coll O. Chronic viral infections and invasive procedures: risk of vertical transmission and current recommendations. Fetal Diagn Ther. 2010;28(1):1.
Yi W, Pan CQ, Hao J, Hu Y, Liu M, Li L, et al. Risk of hepatitis B virus vertical transmission after amniocentsis in mothers with chronic hepatitis B. J Hepatol. 2013. doi:10.1016/j.jhep.2013.11.008.
Zou H, Chen Y, Duan Z, Zhang H, Pan C. Virologic factors associated with failure to passive-active immunoprophylaxis in infants born to HBsAg-positive mothers. J Viral Hepat. 2012;19:e18–25.
Xu WM, Cui YT, Wang L, Yang H, Liang ZQ, Li XM, et al. Lamivudine in late pregnancy to prevent perinatal transmission of hepatitis B virus infection: a multicentre, randomized, double-blind, placebo-controlled study. J Viral Hepat. 2009;16:94–103.
Han L, Zhang H-W, Xie J-X, Zhang Q, Wang H-Y, Cao G-W. A meta-analysis of lamivudine for interruption of mother-to-child transmission of hepatitis B virus. World J Gastroenterol. 2011;17(38):4321–33. doi:10.3748/wjg.v17.i38.4321.
Pan CQ, Liu M, Cai H, Yo W. Safety of tenofovir disoproxil fumarate (TDF) treatment for the entire pregnancy in mothers with active chronic hepatitis B or cirrhosis [abstract]. Hepatology. 2013;58:624A.
Pan CQ, Mi LJ, Bunchorntavakul C, Karsdon J, Huang WM, Singhvi G, et al. Tenofovir disoproxil fumarate for prevention of vertical transmission of hepatitis B virus infection by highly viremic pregnant women: a case series. Dig Dis Sci. 2012;57:2423–9.
Tsai Pai-Jong S, Chang A, Yamada S, Tsai N, Bartholomew L. Use of tenofovir disoproxil fumarate in highly viremic hepatitis B mono-infected pregnant women. Dig Dis Sci. 2014;59:2797–803.
Greenup AJ, Tan PK, Nguyen V, Glass A, Davison S, Chatterjee U, et al. Efficacy and safety of tenofovir tisoproxil fumarate in pregnancy to prevent perinatal transmission of hepatitis B virus. J Hepatol. 2014;61:502–7. First prospective, controlled study to demonstrate the safety and efficacy of tenofovir in prevention MTCT in women with high viral load (>7 log copies/ml).
Han GR, Cao MK, Zhao W, Jiang HX, Wang CM, Bai SF, et al. A prospective and open-label study for the efficacy and safety of telbivudine in pregnancy for the prevention of perinatal transmission of hepatitis B virus infection. J Hepatol. 2011;55:1215–21.
Pan CQ, Han GR, Jiang HX, Zhao W, Cao MK, Wang CM. Telbivudine prevents vertical transmission from HBeAg-positive women with chronic hepatitis B. Clin Gastroenterol Hepatol. 2012;10:520–6.
Liu M, Cai H, Yi W. Safety of telbivudine treatment for chronic hepatitis B for the entire pregnancy. J Viral Hepat. 2013;20:S1:65–70.
Zhang H, Pan CQ, Pang Q, Tian R, Yan M, Liu X. Telbivudine or lamivudine use in late pregnancy safely reduces perinatal transmission of hepatitis B virus in real-life practice. Hepatology. 2014;60(2):468–76. Largest prospective study to date of telbivudine for prevention of MTCT of HBV in women with high viral load (>6 log copies/ml).
Mast R, Margolis H, Fiore A, Brink E, Goldstein S, Wang S. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunizations of infants, children, and adolescents. Atlanta: CDC; 2005. p. 1–23.
Wiseman E, Fraser MA, Holden S, Glass A, Kidson BL, Heron LG, et al. Perinatal transmission of hepatitis B virus: an Australian experience. Med J Aust. 2009;190(9):489.
Guo Z, Xiaohong S, Feng Y, Wang B, Feng L, Wang S, et al. Risk factors of HBV intrauterine transmission among HBsAg-positive pregnant women. J Viral Hepat. 2013;20:317–21.
Kang W, Ding Z, Shen L, Zhao Z, Huang G, Zhang J, et al. Risk factors associated with immunoprophylaxis failure against mother to child transmission of hepatitis B virus and hepatitis B vaccination status in Yunnan Province, China. Vaccine. 2014;32:3362–6.
Kubo A, Shlager L, Marks A, Lakritz D, Beaumont C, Gabellini K, et al. Prevention of vertical transmission of hepatitis B: an observational study. Ann Intern Med. 2014;160:828–35.
Chang MS, Gavini S, Andrade PC, McNabb-Baltar J. Caesarean section to prevent transmission of hepatitis B: a meta-analysis. Can J Gastroenterol Hepatol. 2014;28:439–44.
Nguyen V, Tan PK, Greenup AJ, Glass A, Davison S, Samarsinghe D, et al. Anti-viral therapy for prevention of perinatal HBV transmission: extending therapy beyond birth does not protect against post-partum flare. Aliment Pharmacol Ther. 2014;39:1225–34. Observational study of 101 pregnancies in women with HBV treated with either lamivudine, tenofovir or no antiviral. Post partum flare rates between 30–50%, not significantly impacted by length of post-partum antiviral treatment, most of which were mild and resolved spontaneously.
Giles M, Visvanathan K, Lewin S, Bowden S, Locarnini S, Spelman T, et al. Clinical and virologic predictors of hepatic flares in pregnant women with chronic hepatitis B. Gut. 2014;1–6.
World Health Organization. First-line ART for pregnant and breastfeeding women and ARV drugs for their infants. June 2013. 9 March 2015 <www.who.int/hiv/pub/guidelines/arv2013/art/artpregnantwomen/en>.
Ehrhardt S, Xie C, Guo N, Nelson K, Thio C. Breastfeeding while taking lamivudine or tenofovir disoproxil fumarate: a review of the evidence. CID. 2015;60:275–8. Narrative review of the evidence for antiviral use while breastfeeding.
Yeh RF, Rezk NL, Kashuba AD, et al. Genital tract, cord blood, and amniotic fluid exposures of seven antiretroviral drugs during and after pregnancy in human immunodeficiency virus type 1-infected women. Antimicrob Agents Chemother. 2009;53:2367–74.
Shapiro RL, Holland DT, Capparelli E, et al. Antiretroviral concentrations in breastfeeding infants of women in Botswana receiving antiretroviral treatment. J Infect Dis. 2005;192:720–7.
Giuliano M, Guidotti G, Andreotti M, et al. Triple antiretroviral prophylaxis administered during pregnancy and after delivery significantly reduces breast milk viral load: a study within the Drug Resource Enhancement Against AIDS and Malnutrition Program. J Acquir Immune Defic Syndr. 2007;44:286–91.
Moodley J, Moodley D, Pillay K, et al. Pharmacokinetics and antiretroviral activity of lamivudine alone or when coadministered with zidovudine in human immunodeficiency virus type 1-infected pregnant women and their offspring. J Infect Dis. 1998;178:1327–33.
Chappuy H, Treluyer JM, Jullien V, et al. Maternal-fetal transfer and amniotic fluid accumulation of nucleoside analogue reverse transcriptase inhibitors in human immunodeficiency virus-infected pregnant women. Antimicrob Agents Chemother. 2004;48:4332–6.
Mandelbrot L, Peytavin G, Firtion G, Farinotti R. Maternal-fetal transfer and amniotic fluid accumulation of lamivudine in human immunodeficiency virus-infected pregnant women. Am J Obstet Gynecol. 2001;184:153–8.
Corbett AH, Kayira D, White NR, et al. Antiretroviral pharmacokinetics in mothers and breastfeeding infants from 6 to 24 weeks post partum: results of the BAN study. Antivir Ther. 2014. doi:10.3851/IMP2739.
Palombi L, Pirillo MF, Andreotti M, et al. Antiretroviral prophylaxis for breastfeeding transmission in Malawi: drug concentrations, virological efficacy and safety. Antivir Ther. 2012;17:1511–9.
Mirochnick M, Thomas T, Capparelli E, et al. Antiretroviral concentrations in breastfeeding infants of mothers receiving highly active antiretroviral therapy. Antimicrob Agents Chemother. 2009;53:1170–6.
Benaboud S, Pruvost A, Coffie PA, et al. Concentrations of tenofovir and emtricitabine in breast milk of HIV-1-infected women in Abidjan, Cote d’Ivoire, in the ANRS 12109 TEmAA study, step 2. Antimicrob Agents Chemother. 2011;55:1315–7.
Van Rompay KK, Brignolo LL, Meyer DJ, et al. Biological effects of short-term or prolonged administration of 9-[2-(phosphonomethoxy) propyl]adenine (tenofovir) to newborn and infant rhesus macaques. Antimicrob Agents Chemother. 2004;48:1469–87.
Chen X, Chen J, Wen J, Xu C, Zhang S, et al. Breastfeeding is not a risk factor for mother-to-child transmission of hepatitis B virus. PLoS ONE. 2013;8, e55303. doi:10.1371/journal.pone.0055303.
Chang M, Tuomala R, Rutherford A, Muthoka M, Andersson K, Burman B, et al. Postpartum care for mothers diagnosed with hepatitis B during pregnancy. Am J Obstet Gynecol. 2014;211:1.e1–7.
Compliance with Ethics Guidelines
Conflict of Interest
Erin Kelly declares no conflict of interest. Marion Peters reports honoraria from J&J, Biotron, Merck, Roche, and Genentech Research and Development.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Hepatitis B
Rights and permissions
About this article
Cite this article
Kelly, E., Peters, M.G. Management of HBV in Pregnancy. Curr Hepatology Rep 14, 145–152 (2015). https://doi.org/10.1007/s11901-015-0266-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-015-0266-6