Abstract
Purpose of Review
Porcine islets represent a potentially attractive beta-cell source for xenotransplantation into patients with type 1 diabetes, who are not eligible to islet allo-transplantation due to a lack of suitable human donor organs. Recent progress in genetic engineering/gene editing of donor pigs provides new opportunities to overcome rejection of xeno-islets, to improve their engraftment and insulin secretion capacity, and to reduce the risk for transmission of porcine endogenous retroviruses. This review summarizes the current issues and progress in islet xenotransplantation with special emphasis on genetically modified/gene edited donor pigs.
Recent Findings
Attempts to overcome acute rejection of xeno-islets, especially after intraportal transplantation into the liver, include the genetic elimination of specific carbohydrate antigens such as αGal, Neu5Gc, and Sd(a) for which humans and—in part—non-human primates have natural antibodies that bind to these targets leading to activation of complement and coagulation. A complementary approach is the expression of one or more human complement regulatory proteins (hCD46, hCD55, hCD59). Transgenic attempts to overcome cellular rejection of islet xenotransplants include the expression of proteins that inhibit co-stimulation of T cells. Expression of glucagon-like peptide-1 and M3 muscarinic receptors has been shown to increase the insulin secretion of virally transduced porcine islets in vitro and it will be interesting to see the effects of these modifications in transgenic pigs and islet products derived from them. Genome-wide inactivation of porcine endogenous retrovirus (PERV) integrants by mutating their pol genes using CRISPR/Cas9 is a recent approach to reduce the risk for PERV transmission by xeno-islets.
Summary
Genetic engineering/gene editing of xeno-islet donor pigs facilitated major progress towards clinical islet xenotransplantation. The required set of genetic modifications will depend on the source of islets (fetal/neonatal vs. adult), the mode of delivery (encapsulated vs. free), and the transplantation site.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000;343(4):230–8. https://doi.org/10.1056/NEJM200007273430401.
Chang CA, Lawrence MC, Naziruddin B. Current issues in allogeneic islet transplantation. Curr Opin Organ Transplant. 2017;22(5):437–43. https://doi.org/10.1097/MOT.0000000000000448.
Rickels MR, Stock PG, de Koning EJP, Piemonti L, Pratschke J, Alejandro R, et al. Defining outcomes for beta-cell replacement therapy in the treatment of diabetes: a consensus report on the Igls criteria from the IPITA/EPITA opinion leaders workshop. Transpl Int. 2018;31(4):343–52. https://doi.org/10.1111/tri.13138.
Schuetz C, Anazawa T, Cross SE, Labriola L, Meier RPH, Redfield RR 3rd, et al. Beta cell replacement therapy: the next 10 years. Transplantation. 2018;102(2):215–29. https://doi.org/10.1097/TP.0000000000001937.
Ellis C, Ramzy A, Kieffer TJ. Regenerative medicine and cell-based approaches to restore pancreatic function. Nat Rev Gastroenterol Hepatol. 2017;14(10):612–28. https://doi.org/10.1038/nrgastro.2017.93.
Zhou Q, Melton DA. Pancreas regeneration. Nature. 2018;557(7705):351–8. https://doi.org/10.1038/s41586-018-0088-0.
Suchy F, Nakauchi H. Interspecies chimeras. Curr Opin Genet Dev. 2018;52:36–41. https://doi.org/10.1016/j.gde.2018.05.007.
Nagaraju S, Bottino R, Wijkstrom M, Trucco M, Cooper DK. Islet xenotransplantation: what is the optimal age of the islet-source pig? Xenotransplantation. 2015;22(1):7–19. https://doi.org/10.1111/xen.12130.
Liu Z, Hu W, He T, Dai Y, Hara H, Bottino R, et al. Pig-to-primate islet xenotransplantation: past, present, and future. Cell Transplant. 2017;26(6):925–47. https://doi.org/10.3727/096368917x694859.
Steffen A, Kiss T, Schmid J, Schubert U, Heinke S, Lehmann S et al. Production of high-quality islets from goettingen minipigs: Choice of organ preservation solution, donor pool, and optimal cold ischemia time. Xenotransplantation. 2017;24(1). https://doi.org/10.1111/xen.12284.
Ellis C, Lyon JG, Korbutt GS. Optimization and scale-up isolation and culture of neonatal porcine islets: potential for clinical application. Cell Transplant. 2016;25(3):539–47. https://doi.org/10.3727/096368915x689451.
Mourad NI, Gianello PR. Xenoislets: porcine pancreatic islets for the treatment of type I diabetes. Curr Opin Organ Transplant. 2017;22(6):529–34. https://doi.org/10.1097/mot.0000000000000464.
Hassouna T, Seeberger KL, Salama B, Korbutt GS. Functional maturation and in vitro differentiation of neonatal porcine islet grafts. Transplantation. 2018. https://doi.org/10.1097/tp.0000000000002354.
Jimenez-Vera E, Davies S, Phillips P, O'Connell PJ, Hawthorne WJ. Long-term cultured neonatal islet cell clusters demonstrate better outcomes for reversal of diabetes: in vivo and molecular profiles. Xenotransplantation. 2015;22(2):114–23. https://doi.org/10.1111/xen.12151.
Li WC, Chen CY, Kao CW, Huang PC, Hsieh YT, Kuo TY, et al. Porcine neonatal pancreatic cell clusters maintain their multipotency in culture and after transplantation. Sci Rep. 2018;8(1):8212. https://doi.org/10.1038/s41598-018-26404-6.
Klymiuk N, Ludwig B, Seissler J, Reichart B, Wolf E. Current concepts of using pigs as a source for beta-cell replacement therapy of type 1 diabetes. Curr Mol Biol Rep. 2016;2(2):73–82. https://doi.org/10.1007/s40610-016-0039-1.
Zhu HT, Yu L, Lyu Y, Wang B. Optimal pig donor selection in islet xenotransplantation: current status and future perspectives. J Zhejiang Univ Sci B. 2014;15(8):681–91. https://doi.org/10.1631/jzus.B1400120.
Salama BF, Korbutt GS. Porcine islet xenografts: a clinical source of ss-cell grafts. Curr Diab Rep. 2017;17(3):14. https://doi.org/10.1007/s11892-017-0846-7.
Shin JS, Min BH, Kim JM, Kim JS, Yoon IH, Kim HJ, et al. Failure of transplantation tolerance induction by autologous regulatory T cells in the pig-to-non-human primate islet xenotransplantation model. Xenotransplantation. 2016;23(4):300–9. https://doi.org/10.1111/xen.12246.
Shin JS, Kim JM, Min BH, Yoon IH, Kim HJ, Kim JS et al. Pre-clinical results in pig-to-non-human primate islet xenotransplantation using anti-CD40 antibody (2C10R4)-based immunosuppression. Xenotransplantation. 2018;25(1). https://doi.org/10.1111/xen.12356.
Morozov VA, Wynyard S, Matsumoto S, Abalovich A, Denner J, Elliott R. No PERV transmission during a clinical trial of pig islet cell transplantation. Virus Res. 2017;227:34–40. https://doi.org/10.1016/j.virusres.2016.08.012.
Wynyard S, Nathu D, Garkavenko O, Denner J, Elliott R. Microbiological safety of the first clinical pig islet xenotransplantation trial in New Zealand. Xenotransplantation. 2014;21(4):309–23. https://doi.org/10.1111/xen.12102.
Matsumoto S, Abalovich A, Wechsler C, Wynyard S, Elliott RB. Clinical benefit of islet xenotransplantation for the treatment of type 1 diabetes. EBioMedicine. 2016;12:255–62. https://doi.org/10.1016/j.ebiom.2016.08.034.
Ludwig B, Ludwig S, Steffen A, Knauf Y, Zimerman B, Heinke S, et al. Favorable outcome of experimental islet xenotransplantation without immunosuppression in a nonhuman primate model of diabetes. Proc Natl Acad Sci U S A. 2017;114(44):11745–50. https://doi.org/10.1073/pnas.1708420114.
Cohrs CM, Chen C, Jahn SR, Stertmann J, Chmelova H, Weitz J, et al. Vessel network architecture of adult human islets promotes distinct cell-cell interactions in situ and is altered after transplantation. Endocrinology. 2017;158(5):1373–85. https://doi.org/10.1210/en.2016-1184.
Kemter E, Cohrs CM, Schafer M, Schuster M, Steinmeyer K, Wolf-van Buerck L, et al. INS-eGFP transgenic pigs: a novel reporter system for studying maturation, growth and vascularisation of neonatal islet-like cell clusters. Diabetologia. 2017;60(6):1152–6. https://doi.org/10.1007/s00125-017-4250-2.
Schuetz C, Markmann JF. Islet cell transplant: update on current clinical trials. Curr Transplant Rep. 2016;3(3):254–63. https://doi.org/10.1007/s40472-016-0103-z.
Aigner B, Klymiuk N, Wolf E. Transgenic pigs for xenotransplantation: selection of promoter sequences for reliable transgene expression. Curr Opin Organ Transplant. 2010;15(2):201–6. https://doi.org/10.1097/MOT.0b013e328336ba4a.
Phelps CJ, Koike C, Vaught TD, Boone J, Wells KD, Chen SH, et al. Production of alpha 1,3-galactosyltransferase-deficient pigs. Science. 2003;299(5605):411–4. https://doi.org/10.1126/science.1078942.
Mourad NI, Gianello P. Gene editing, gene therapy, and cell xenotransplantation: cell transplantation across species. Curr Transplant Rep. 2017;4(3):193–200. https://doi.org/10.1007/s40472-017-0157-6.
Fischer K, Kind A, Schnieke A. Assembling multiple xenoprotective transgenes in pigs. Xenotransplantation. 2018:e12431. https://doi.org/10.1111/xen.12431.
Thompson P, Badell IR, Lowe M, Cano J, Song M, Leopardi F, et al. Islet xenotransplantation using gal-deficient neonatal donors improves engraftment and function. Am J Transplant. 2011;11(12):2593–602. https://doi.org/10.1111/j.1600-6143.2011.03720.x.
Kwon DN, Lee K, Kang MJ, Choi YJ, Park C, Whyte JJ, et al. Production of biallelic CMP-Neu5Ac hydroxylase knock-out pigs. Sci Rep. 2013;3:1981. https://doi.org/10.1038/srep01981.
Lutz AJ, Li P, Estrada JL, Sidner RA, Chihara RK, Downey SM, et al. Double knockout pigs deficient in N-glycolylneuraminic acid and galactose alpha-1,3-galactose reduce the humoral barrier to xenotransplantation. Xenotransplantation. 2013;20(1):27–35. https://doi.org/10.1111/xen.12019.
Salama A, Mosser M, Leveque X, Perota A, Judor JP, Danna C, et al. Neu5Gc and alpha1-3 GAL Xenoantigen knockout does not affect Glycemia homeostasis and insulin secretion in pigs. Diabetes. 2017;66(4):987–93. https://doi.org/10.2337/db16-1060.
Estrada JL, Martens G, Li P, Adams A, Newell KA, Ford ML, et al. Evaluation of human and non-human primate antibody binding to pig cells lacking GGTA1/CMAH/beta4GalNT2 genes. Xenotransplantation. 2015;22(3):194–202. https://doi.org/10.1111/xen.12161.
Diamond LE, Quinn CM, Martin MJ, Lawson J, Platt JL, Logan JS. A human CD46 transgenic pig model system for the study of discordant xenotransplantation. Transplantation. 2001;71(1):132–42.
McKenzie IF, Li YQ, Xing PX, Dinatale I, Koulmanda M, Loveland BE, et al. CD46 protects pig islets from antibody but not cell-mediated destruction in the mouse. Xenotransplantation. 2003;10(6):615–21.
van der Windt DJ, Bottino R, Casu A, Campanile N, Smetanka C, He J, et al. Long-term controlled normoglycemia in diabetic non-human primates after transplantation with hCD46 transgenic porcine islets. Am J Transplant. 2009;9(12):2716–26. https://doi.org/10.1111/j.1600-6143.2009.02850.x.
Cozzi E, White DJ. The generation of transgenic pigs as potential organ donors for humans. Nat Med. 1995;1(9):964–6.
Hawthorne WJ, Salvaris EJ, Phillips P, Hawkes J, Liuwantara D, Burns H, et al. Control of IBMIR in neonatal porcine islet xenotransplantation in baboons. Am J Transplant. 2014;14(6):1300–9. https://doi.org/10.1111/ajt.12722.
Mandel TE, Koulmanda M, Cozzi E, Waterworth P, Tolan M, Langford G, et al. Transplantation of normal and DAF-transgenic fetal pig pancreas into cynomolgus monkeys. Transplant Proc. 1997;29(1–2 /01):940.
Fodor WL, Williams BL, Matis LA, Madri JA, Rollins SA, Knight JW, et al. Expression of a functional human complement inhibitor in a transgenic pig as a model for the prevention of xenogeneic hyperacute organ rejection. Proc Natl Acad Sci U S A. 1994;91(23):11153–7.
Kwon DJ, Kim DH, Hwang IS, Kim DE, Kim HJ, Kim JS, et al. Generation of alpha-1,3-galactosyltransferase knocked-out transgenic cloned pigs with knocked-in five human genes. Transgenic Res. 2017;26(1):153–63. https://doi.org/10.1007/s11248-016-9979-8.
Wuensch A, Baehr A, Bongoni AK, Kemter E, Blutke A, Baars W, et al. Regulatory sequences of the porcine THBD gene facilitate endothelial-specific expression of bioactive human thrombomodulin in single- and multitransgenic pigs. Transplantation. 2014;97(2):138–47. https://doi.org/10.1097/TP.0b013e3182a95cbc.
Iwase H, Ekser B, Hara H, Phelps C, Ayares D, Cooper DK, et al. Regulation of human platelet aggregation by genetically modified pig endothelial cells and thrombin inhibition. Xenotransplantation. 2014;21(1):72–83. https://doi.org/10.1111/xen.12073.
Lin CC, Ezzelarab M, Hara H, Long C, Lin CW, Dorling A, et al. Atorvastatin or transgenic expression of TFPI inhibits coagulation initiated by anti-nonGal IgG binding to porcine aortic endothelial cells. J Thromb Haemost. 2010;8(9):2001–10. https://doi.org/10.1111/j.1538-7836.2010.03950.x.
Bottino R, Wijkstrom M, van der Windt DJ, Hara H, Ezzelarab M, Murase N, et al. Pig-to-monkey islet xenotransplantation using multi-transgenic pigs. Am J Transplant. 2014;14(10):2275–87. https://doi.org/10.1111/ajt.12868.
Wheeler DG, Joseph ME, Mahamud SD, Aurand WL, Mohler PJ, Pompili VJ, et al. Transgenic swine: expression of human CD39 protects against myocardial injury. J Mol Cell Cardiol. 2012;52(5):958–61. https://doi.org/10.1016/j.yjmcc.2012.01.002.
Lee SC, Lee H, Oh KB, Hwang IS, Yang H, Park MR, et al. Production and breeding of transgenic cloned pigs expressing human CD73. Dev Reprod. 2017;21(2):157–65. https://doi.org/10.12717/dr.2017.21.2.157.
Klymiuk N, van Buerck L, Bahr A, Offers M, Kessler B, Wuensch A, et al. Xenografted islet cell clusters from INSLEA29Y transgenic pigs rescue diabetes and prevent immune rejection in humanized mice. Diabetes. 2012;61(6):1527–32. https://doi.org/10.2337/db11-1325.
• Wolf-van Buerck L, Schuster M, Oduncu FS, Baehr A, Mayr T, Guethoff S, et al. LEA29Y expression in transgenic neonatal porcine islet-like cluster promotes long-lasting xenograft survival in humanized mice without immunosuppressive therapy. Sci Rep. 2017;7(1):3572. https://doi.org/10.1038/s41598-017-03913-4. Local transgene expression of the immunoregulator LEA29Y by the graft induce local immuneregulation and enables free islet transplant survival without systemic immunosuppression.
Martin C, Plat M, Nerriere-Daguin V, Coulon F, Uzbekova S, Venturi E, et al. Transgenic expression of CTLA4-Ig by fetal pig neurons for xenotransplantation. Transgenic Res. 2005;14(4):373–84.
Phelps CJ, Ball SF, Vaught TD, Vance AM, Mendicino M, Monahan JA, et al. Production and characterization of transgenic pigs expressing porcine CTLA4-Ig. Xenotransplantation. 2009;16(6):477–85. https://doi.org/10.1111/j.1399-3089.2009.00533.x.
Reyes LM, Estrada JL, Wang ZY, Blosser RJ, Smith RF, Sidner RA, et al. Creating class I MHC-null pigs using guide RNA and the Cas9 endonuclease. J Immunol. 2014;193(11):5751–7. https://doi.org/10.4049/jimmunol.1402059.
Hara H, Witt W, Crossley T, Long C, Isse K, Fan L, et al. Human dominant-negative class II transactivator transgenic pigs - effect on the human anti-pig T-cell immune response and immune status. Immunology. 2013;140(1):39–46. https://doi.org/10.1111/imm.12107.
Klose R, Kemter E, Bedke T, Bittmann I, Kelsser B, Endres R, et al. Expression of biologically active human TRAIL in transgenic pigs. Transplantation. 2005;80(2):222–30.
Kemter E, Lieke T, Kessler B, Kurome M, Wuensch A, Summerfield A, et al. Human TNF-related apoptosis-inducing ligand-expressing dendritic cells from transgenic pigs attenuate human xenogeneic T cell responses. Xenotransplantation. 2012;19(1):40–51. https://doi.org/10.1111/j.1399-3089.2011.00688.x.
Buermann A, Petkov S, Petersen B, Hein R, Lucas-Hahn A, Baars W, et al. Pigs expressing the human inhibitory ligand PD-L1 (CD 274) provide a new source of xenogeneic cells and tissues with low immunogenic properties. Xenotransplantation. 2018; https://doi.org/10.1111/xen.12387.
Weiss EH, Lilienfeld BG, Muller S, Muller E, Herbach N, Kessler B, et al. HLA-E/human beta2-microglobulin transgenic pigs: protection against xenogeneic human anti-pig natural killer cell cytotoxicity. Transplantation. 2009;87(1):35–43. https://doi.org/10.1097/TP.0b013e318191c784.
Tena A, Kurtz J, Leonard DA, Dobrinsky JR, Terlouw SL, Mtango N, et al. Transgenic expression of human CD47 markedly increases engraftment in a murine model of pig-to-human hematopoietic cell transplantation. Am J Transplant. 2014;14(12):2713–22. https://doi.org/10.1111/ajt.12918.
Oropeza M, Petersen B, Carnwath JW, Lucas-Hahn A, Lemme E, Hassel P, et al. Transgenic expression of the human A20 gene in cloned pigs provides protection against apoptotic and inflammatory stimuli. Xenotransplantation. 2009;16(6):522–34. https://doi.org/10.1111/j.1399-3089.2009.00556.x.
Petersen B, Ramackers W, Lucas-Hahn A, Lemme E, Hassel P, Queisser AL, et al. Transgenic expression of human heme oxygenase-1 in pigs confers resistance against xenograft rejection during ex vivo perfusion of porcine kidneys. Xenotransplantation. 2011;18(6):355–68. https://doi.org/10.1111/j.1399-3089.2011.00674.x.
Park SJ, Cho B, Koo OJ, Kim H, Kang JT, Hurh S, et al. Production and characterization of soluble human TNFRI-fc and human HO-1(HMOX1) transgenic pigs by using the F2A peptide. Transgenic Res. 2014;23(3):407–19. https://doi.org/10.1007/s11248-013-9780-x.
Yan JJ, Yeom HJ, Jeong JC, Lee JG, Lee EW, Cho B, et al. Beneficial effects of the transgenic expression of human sTNF-alphaR-fc and HO-1 on pig-to-mouse islet xenograft survival. Transpl Immunol. 2016;34:25–32. https://doi.org/10.1016/j.trim.2016.01.002.
Lee HS, Lee JG, Yeom HJ, Chung YS, Kang B, Hurh S, et al. The introduction of human heme oxygenase-1 and soluble tumor necrosis factor-alpha receptor type I with human IgG1 fc in porcine islets prolongs islet xenograft survival in humanized mice. Am J Transplant. 2016;16(1):44–57. https://doi.org/10.1111/ajt.13467.
Miyagawa S, Nakatsu S, Nakagawa T, Kondo A, Matsunami K, Hazama K, et al. Prevention of PERV infections in pig to human xenotransplantation by the RNA interference silences gene. J Biochem. 2005;137(4):503–8. https://doi.org/10.1093/jb/mvi059.
Dieckhoff B, Petersen B, Kues WA, Kurth R, Niemann H, Denner J. Knockdown of porcine endogenous retrovirus (PERV) expression by PERV-specific shRNA in transgenic pigs. Xenotransplantation. 2008;15(1):36–45. https://doi.org/10.1111/j.1399-3089.2008.00442.x.
Ramsoondar J, Vaught T, Ball S, Mendicino M, Monahan J, Jobst P, et al. Production of transgenic pigs that express porcine endogenous retrovirus small interfering RNAs. Xenotransplantation. 2009;16(3):164–80. https://doi.org/10.1111/j.1399-3089.2009.00525.x.
Semaan M, Kaulitz D, Petersen B, Niemann H, Denner J. Long-term effects of PERV-specific RNA interference in transgenic pigs. Xenotransplantation. 2012;19(2):112–21. https://doi.org/10.1111/j.1399-3089.2012.00683.x.
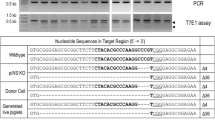
•• Niu D, Wei HJ, Lin L, George H, Wang T, Lee IH, et al. Inactivation of porcine endogenous retrovirus in pigs using CRISPR-Cas9. Science. 2017;357(6357):1303–7. https://doi.org/10.1126/science.aan4187. Animals with inactivated PERVs in the pig genome were generated.
Wijkstrom M, Bottino R, Iwase H, Hara H, Ekser B, van der Windt D, et al. Glucose metabolism in pigs expressing human genes under an insulin promoter. Xenotransplantation. 2015;22(1):70–9. https://doi.org/10.1111/xen.12145.
Le Bas-Bernardet S, Tillou X, Poirier N, Dilek N, Chatelais M, Devalliere J, et al. Xenotransplantation of galactosyl-transferase knockout, CD55, CD59, CD39, and fucosyl-transferase transgenic pig kidneys into baboons. Transplant Proc. 2011;43(9):3426–30. https://doi.org/10.1016/j.transproceed.2011.09.024.
Chen Y, Stewart JM, Gunthart M, Hawthorne WJ, Salvaris EJ, O'Connell PJ, et al. Xenoantibody response to porcine islet cell transplantation using GTKO, CD55, CD59, and fucosyltransferase multiple transgenic donors. Xenotransplantation. 2014;21(3):244–53. https://doi.org/10.1111/xen.12091.
Liu F, Liu J, Yuan Z, Qing Y, Li H, Xu K, et al. Generation of GTKO Diannan miniature pig expressing human complementary regulator proteins hCD55 and hCD59 via T2A peptide-based Bicistronic vectors and SCNT. Mol Biotechnol. 2018;60:550–62. https://doi.org/10.1007/s12033-018-0091-6.
Gao H, Zhao C, Xiang X, Li Y, Zhao Y, Li Z, et al. Production of alpha1,3-galactosyltransferase and cytidine monophosphate-N-acetylneuraminic acid hydroxylase gene double-deficient pigs by CRISPR/Cas9 and handmade cloning. J Reprod Dev. 2017;63(1):17–26. https://doi.org/10.1262/jrd.2016-079.
Fischer K, Kraner-Scheiber S, Petersen B, Rieblinger B, Buermann A, Flisikowska T, et al. Efficient production of multi-modified pigs for xenotransplantation by 'combineering', gene stacking and gene editing. Sci Rep. 2016;6:29081. https://doi.org/10.1038/srep29081.
Kim GA, Lee EM, Jin JX, Lee S, Taweechaipaisankul A, Hwang JI, et al. Generation of CMAHKO/GTKO/shTNFRI-fc/HO-1 quadruple gene modified pigs. Transgenic Res. 2017;26(4):435–45. https://doi.org/10.1007/s11248-017-0021-6.
Martens GR, Reyes LM, Butler JR, Ladowski JM, Estrada JL, Sidner RA, et al. Humoral reactivity of renal transplant-waitlisted patients to cells from GGTA1/CMAH/B4GalNT2, and SLA class I knockout pigs. Transplantation. 2017;101(4):e86–92. https://doi.org/10.1097/tp.0000000000001646.
Zhang R, Wang Y, Chen L, Wang R, Li C, Li X, et al. Reducing immunoreactivity of porcine bioprosthetic heart valves by genetically-deleting three major glycan antigens, GGTA1/beta4GalNT2/CMAH. Acta Biomater. 2018;72:196–205. https://doi.org/10.1016/j.actbio.2018.03.055.
Li P, Estrada JL, Burlak C, Montgomery J, Butler JR, Santos RM, et al. Efficient generation of genetically distinct pigs in a single pregnancy using multiplexed single-guide RNA and carbohydrate selection. Xenotransplantation. 2015;22(1):20–31. https://doi.org/10.1111/xen.12131.
Choi K, Shim J, Ko N, Eom H, Kim J, Lee JW, et al. Production of heterozygous alpha 1,3-galactosyltransferase (GGTA1) knock-out transgenic miniature pigs expressing human CD39. Transgenic Res. 2017;26(2):209–24. https://doi.org/10.1007/s11248-016-9996-7.
Kourtzelis I, Magnusson PU, Kotlabova K, Lambris JD, Chavakis T. Regulation of instant blood mediated inflammatory reaction (IBMIR) in pancreatic islet xeno-transplantation: points for therapeutic interventions. Adv Exp Med Biol. 2015;865:171–88. https://doi.org/10.1007/978-3-319-18603-0_11.
Byrne GW, McGregor CG, Breimer ME. Recent investigations into pig antigen and anti-pig antibody expression. Int J Surg. 2015;23(Pt B):223–8. https://doi.org/10.1016/j.ijsu.2015.07.724.
Rayat GR, Rajotte RV, Hering BJ, Binette TM, Korbutt GS. In vitro and in vivo expression of Galalpha-(1,3)gal on porcine islet cells is age dependent. J Endocrinol. 2003;177(1):127–35.
Lee W, Hara H, Ezzelarab MB, Iwase H, Bottino R, Long C, et al. Initial in vitro studies on tissues and cells from GTKO/CD46/NeuGcKO pigs. Xenotransplantation. 2016;23(2):137–50. https://doi.org/10.1111/xen.12229.
Martin BM, Samy KP, Lowe MC, Thompson PW, Cano J, Farris AB, et al. Dual islet transplantation modeling of the instant blood-mediated inflammatory reaction. Am J Transplant. 2015;15(5):1241–52. https://doi.org/10.1111/ajt.13098.
Hawthorne WJ, Lew AM, Thomas HE. Genetic strategies to bring islet xenotransplantation to the clinic. Curr Opin Organ Transplant. 2016;21(5):476–83. https://doi.org/10.1097/mot.0000000000000353.
van der Windt DJ, Bottino R, Casu A, Campanile N, Cooper DK. Rapid loss of intraportally transplanted islets: an overview of pathophysiology and preventive strategies. Xenotransplantation. 2007;14(4):288–97. https://doi.org/10.1111/j.1399-3089.2007.00419.x.
Cowan PJ, Robson SC. Progress towards overcoming coagulopathy and hemostatic dysfunction associated with xenotransplantation. Int J Surg. 2015;23(Pt B):296–300. https://doi.org/10.1016/j.ijsu.2015.07.682.
Vadori M, Cozzi E. The immunological barriers to xenotransplantation. Tissue Antigens. 2015;86(4):239–53. https://doi.org/10.1111/tan.12669.
Lunney JK, Ho CS, Wysocki M, Smith DM. Molecular genetics of the swine major histocompatibility complex, the SLA complex. Dev Comp Immunol. 2009;33(3):362–74. https://doi.org/10.1016/j.dci.2008.07.002.
Griesemer A, Yamada K, Sykes M. Xenotransplantation: immunological hurdles and progress toward tolerance. Immunol Rev. 2014;258(1):241–58. https://doi.org/10.1111/imr.12152.
Plege A, Borns K, Baars W, Schwinzer R. Suppression of human T-cell activation and expansion of regulatory T cells by pig cells overexpressing PD-ligands. Transplantation. 2009;87(7):975–82. https://doi.org/10.1097/TP.0b013e31819c85e8.
Plege-Fleck A, Lieke T, Romermann D, Duvel H, Hundrieser J, Buermann A, et al. Pig to rat cell transplantation: reduced cellular and antibody responses to xenografts overexpressing PD-L1. Xenotransplantation. 2014;21(6):533–42. https://doi.org/10.1111/xen.12121.
• Samy KP, Davis RP, Gao Q, Martin BM, Song M, Cano J, et al. Early barriers to neonatal porcine islet engraftment in a dual transplant model. Am J Transplant. 2018;18(4):998–1006. https://doi.org/10.1111/ajt.14601. This dual islet transplant model provides robust insights into pathomechanism of (xeno)transplant rejection due to properly control experiments comparing modified xenoislet preparations within one transplant recipient.
Bartlett ST, Markmann JF, Johnson P, Korsgren O, Hering BJ, Scharp D, et al. Report from IPITA-TTS opinion leaders meeting on the future of beta-cell replacement. Transplantation. 2016;100(Suppl 2):S1–44. https://doi.org/10.1097/tp.0000000000001055.
Tritschler S, Theis FJ, Lickert H, Bottcher A. Systematic single-cell analysis provides new insights into heterogeneity and plasticity of the pancreas. Mol Metab. 2017;6(9):974–90. https://doi.org/10.1016/j.molmet.2017.06.021.
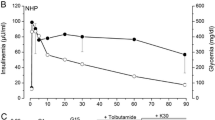
• Mourad NI, Perota A, Xhema D, Galli C, Gianello P. Transgenic expression of glucagon-like Peptide-1 (GLP-1) and activated muscarinic receptor (M3R) significantly improves pig islet secretory function. Cell Transplant. 2017;26(5):901–11. https://doi.org/10.3727/096368916x693798. Insulin content and secretory function of pig islets can be distinctly increased by genetic modifications.
Schuurman HJ. Regulatory aspects of clinical xenotransplantation. Int J Surg. 2015;23(Pt B):312–21. https://doi.org/10.1016/j.ijsu.2015.09.051.
Denner J, Mankertz A. Porcine circoviruses and xenotransplantation. Viruses 2017:9(4). https://doi.org/10.3390/v9040083.
Denner J. Xenotransplantation and porcine cytomegalovirus. Xenotransplantation. 2015;22(5):329–35. https://doi.org/10.1111/xen.12180.
Denner J, Mueller NJ. Preventing transfer of infectious agents. Int J Surg. 2015;23(Pt B):306–11. https://doi.org/10.1016/j.ijsu.2015.08.032.
Denner J. Xenotransplantation and hepatitis E virus. Xenotransplantation. 2015;22(3):167–73. https://doi.org/10.1111/xen.12156.
Egerer S, Fiebig U, Kessler B, Zakhartchenko V, Kurome M, Reichart B, Kupatt C, Klymiuk N, Wolf E, Denner J, Bähr A. Early weaning completely eliminates porcine cytomegalovirus from a newly established pig donor facility for xenotransplantation. Xenotransplantation. 2018;25:e12449. https://doi.org/10.1111/xen.12449.
Crossan C, O'Hara Z, Mourad N, Gianello P, Scobie L. Examining the potential for porcine-derived islet cells to harbour viral pathogens. Xenotransplantation. 2018;25(2):e12375. https://doi.org/10.1111/xen.12375.
Denner J, Tonjes RR. Infection barriers to successful xenotransplantation focusing on porcine endogenous retroviruses. Clin Microbiol Rev. 2012;25(2):318–43. https://doi.org/10.1128/cmr.05011-11.
Crossan C, Mourad NI, Smith K, Gianello P, Scobie L. Assessment of porcine endogenous retrovirus transmission across an alginate barrier used for the encapsulation of porcine islets. Xenotransplantation. 2018:e12409. https://doi.org/10.1111/xen.12409.
Denner J. Why was PERV not transmitted during preclinical and clinical xenotransplantation trials and after inoculation of animals? Retrovirology. 2018;15(1):28. https://doi.org/10.1186/s12977-018-0411-8.
• Denner J, Graham M. Xenotransplantation of islet cells: what can the non-human primate model bring for the evaluation of efficacy and safety? Xenotransplantation. 2015;22(3):231–5. https://doi.org/10.1111/xen.12169. Evidence is provided that non-human primates are of reduced value for efficacy and safety evaluation of islet xenotransplantation.
Denner J, Scobie L, Schuurman HJ. Is it currently possible to evaluate the risk posed by PERVs for clinical xenotransplantation? Xenotransplantation. 2018;25:e12403. https://doi.org/10.1111/xen.12403.
Tacke SJ, Specke V, Denner J. Differences in release and determination of subtype of porcine endogenous retroviruses produced by stimulated normal pig blood cells. Intervirology. 2003;46(1):17–24. https://doi.org/10.1159/000068120.
Dieckhoff B, Kessler B, Jobst D, Kues W, Petersen B, Pfeifer A, et al. Distribution and expression of porcine endogenous retroviruses in multi-transgenic pigs generated for xenotransplantation. Xenotransplantation. 2009;16(2):64–73. https://doi.org/10.1111/j.1399-3089.2009.00515.x.
Wilson CA. Porcine endogenous retroviruses and xenotransplantation. Cell Mol Life Sci. 2008;65(21):3399–412. https://doi.org/10.1007/s00018-008-8498-z.
Denner J, Specke V, Thiesen U, Karlas A, Kurth R. Genetic alterations of the long terminal repeat of an ecotropic porcine endogenous retrovirus during passage in human cells. Virology. 2003;314(1):125–33.
Harrison I, Takeuchi Y, Bartosch B, Stoye JP. Determinants of high titer in recombinant porcine endogenous retroviruses. J Virol. 2004;78(24):13871–9. https://doi.org/10.1128/jvi.78.24.13871-13879.2004.
Kaulitz D, Mihica D, Adlhoch C, Semaan M, Denner J. Improved pig donor screening including newly identified variants of porcine endogenous retrovirus-C (PERV-C). Arch Virol. 2013;158(2):341–8. https://doi.org/10.1007/s00705-012-1490-9.
Kaulitz D, Mihica D, Dorna J, Costa MR, Petersen B, Niemann H, et al. Development of sensitive methods for detection of porcine endogenous retrovirus-C (PERV-C) in the genome of pigs. J Virol Methods. 2011;175(1):60–5. https://doi.org/10.1016/j.jviromet.2011.04.017.
Karlas A, Kurth R, Denner J. Inhibition of porcine endogenous retroviruses by RNA interference: increasing the safety of xenotransplantation. Virology. 2004;325(1):18–23. https://doi.org/10.1016/j.virol.2004.04.022.
Dieckhoff B, Karlas A, Hofmann A, Kues WA, Petersen B, Pfeifer A, et al. Inhibition of porcine endogenous retroviruses (PERVs) in primary porcine cells by RNA interference using lentiviral vectors. Arch Virol. 2007;152(3):629–34. https://doi.org/10.1007/s00705-006-0868-y.
Kaulitz D, Fiebig U, Eschricht M, Wurzbacher C, Kurth R, Denner J. Generation of neutralising antibodies against porcine endogenous retroviruses (PERVs). Virology. 2011;411(1):78–86. https://doi.org/10.1016/j.virol.2010.12.032.
Waechter A, Eschricht M, Denner J. Neutralization of porcine endogenous retrovirus by antibodies against the membrane-proximal external region of the transmembrane envelope protein. J Gen Virol. 2013;94(Pt 3):643–51. https://doi.org/10.1099/vir.0.047399-0.
Denner J, Mihica D, Kaulitz D, Schmidt CM. Increased titers of neutralizing antibodies after immunization with both envelope proteins of the porcine endogenous retroviruses (PERVs). Virol J. 2012;9:260. https://doi.org/10.1186/1743-422x-9-260.
Denner J. How active are porcine endogenous retroviruses (PERVs)? Viruses. 2016;8(8). https://doi.org/10.3390/v8080215.
Fiebig U, Fischer K, Baehr A, Runge C, Schnieke A, Wolf E et al. Porcine endogenous retroviruses (PERV): quantification of the copy number in cell lines, pig breeds and organs. Xenotransplantation. 2018;25:e12445. https://doi.org/10.1111/xen.12445.
Semaan M, Ivanusic D, Denner J. Cytotoxic effects during knock out of multiple porcine endogenous retrovirus (PERV) sequences in the pig genome by zinc finger nucleases (ZFN). PLoS One. 2015;10(4):e0122059. https://doi.org/10.1371/journal.pone.0122059.
• Yang L, Guell M, Niu D, George H, Lesha E, Grishin D, et al. Genome-wide inactivation of porcine endogenous retroviruses (PERVs). Science. 2015;350(6264):1101–4. https://doi.org/10.1126/science.aad1191. Proof-of-principle study that inactivation of all PERV loci genome-wide is feasible.
Denner J. Paving the path toward porcine organs for transplantation. N Engl J Med. 2017;377(19):1891–3. https://doi.org/10.1056/NEJMcibr1710853.
Funding
This work was supported by the Horizon2020 Program, Grant Number 760986 ‘iNanoBIT’, and by the German Research Foundation (DFG), Grant Number 213602983, TRR 127: Biology of xenogeneic cell and organ transplantation—from bench to bedside.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elisabeth Kemter, Joachim Denner, and Eckhard Wolf declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Immunology, Transplantation, and Regenerative Medicine
Rights and permissions
About this article
Cite this article
Kemter, E., Denner, J. & Wolf, E. Will Genetic Engineering Carry Xenotransplantation of Pig Islets to the Clinic?. Curr Diab Rep 18, 103 (2018). https://doi.org/10.1007/s11892-018-1074-5
Published:
DOI: https://doi.org/10.1007/s11892-018-1074-5