Abstract
Purpose of Review
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have been shown to exert benefit on cardiac outcomes. In this review, we provide updates on available clinical data, studies on potential mechanisms for the CV effects, as well as discuss potential clinical implications of these new findings.
Recent Findings
Since the publications of the EMPA-REG and CANVAS trials, large multi-national cohort studies have further shown the cardioprotective effects of SGLT2i. Moreover, new studies examining SGLT2i action on sodium-hydrogen exchanger proteins in both the heart and the kidney, on myocardial energetics and impact on inflammation and atherosclerosis continue to shed light on the multitude of pleotropic effects of these agents.
Summary
Though more data is needed to substantiate the safety and efficacy, SGLT2i should be considered as a valuable therapy to help reduce CV risk in patients with diabetes. Ultimately, SGLT2i may have utility in preventing progression to diabetes or providing CV protection in patients who do not have diabetes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352(9131):837–53.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Association AD. 8. Pharmacologic approaches to glycemic treatment. Diabetes Care. 2018;41(Suppl 1):S73–85.
Association AD. 9. Cardiovascular disease and risk management. Diabetes Care. 2018;41(Suppl 1):S86–S104.
Mechanick JI, Pessah-Pollack R, Camacho P, Correa R, Figaro MK, Garber JR, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Protocol for Standardized Production of Clinical Practice Guidelines, Algorithms, and Checklists—2017 update. Endocr Pract. 2017;23(8):1006–21.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Marso SP, Holst AG, Semaglutide VT. Cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2017;376(9):891–2.
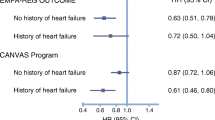
•• Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. Major randomized control trial that concluded CV benefit of empagliflozin
•• Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57. Major randomized control trial that concluded CV benefit of canagliflozin
• Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J. 2016;37(19):1526–34. Post-hoc analysis that showed benefit seen in EMPA-REG was independent of pre-existing heart failure
Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME trial: a “thrifty substrate” hypothesis. Diabetes Care. 2016;39(7):1108–14.
Januzzi JL, Butler J, Jarolim P, Sattar N, Vijapurkar U, Desai M, et al. Effects of canagliflozin on cardiovascular biomarkers in older adults with type 2 diabetes. J Am Coll Cardiol. 2017;70(6):704–12.
Hartmann F, Packer M, Coats AJ, Fowler MB, Krum H, Mohacsi P, et al. Prognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure: a substudy of the carvedilol prospective randomized cumulative survival (COPERNICUS) trial. Circulation. 2004;110(13):1780–6.
Ndumele CE, Matsushita K, Sang Y, Lazo M, Agarwal SK, Nambi V, et al. N-terminal pro-brain natriuretic peptide and heart failure risk among individuals with and without obesity: the atherosclerosis risk in communities (ARIC) study. Circulation. 2016;133(7):631–8.
Blankenberg S, Salomaa V, Makarova N, Ojeda F, Wild P, Lackner KJ, et al. Troponin I and cardiovascular risk prediction in the general population: the BiomarCaRE consortium. Eur Heart J. 2016;37(30):2428–37.
•• Udell JA, Yuan Z, Rush T, Sicignano NM, Galitz M, Rosenthal N. Cardiovascular outcomes and risks after initiation of a sodium glucose cotransporter 2 inhibitor: results from the EASEL population-based cohort study (evidence for cardiovascular outcomes with sodium glucose cotransporter 2 inhibitors in the real world). Circulation. 2018;137(14):1450–9. Large cohort study with results consistent with EMPA-REG and CANVAS
•• Birkeland KI, Jørgensen ME, Carstensen B, Persson F, Gulseth HL, Thuresson M, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 2017;5(9):709–17. Observational study with further evidence of CV benefit of dapagliflozin
•• Kosiborod M, Lam CSP, Kohsaka S, Kim DJ, Karasik A, Shaw J, et al. Lower cardiovascular risk associated with SGLT-2i in >400,000 patients: the CVD-REAL 2 Study. J Am Coll Cardiol 2018;71(23):2628-39. Propensity-matched study showing reduction of MI with dapagliflozin.
Raz I, Mosenzon O, Bonaca MP, Cahn A, Kato ET, Silverman MG, et al. DECLARE-TIMI 58: participants’ baseline characteristics. Diabetes Obes Metab. 2018;20:1102–10.
• Butler J, Hamo CE, Filippatos G, Pocock SJ, Bernstein RA, Brueckmann M, et al. The potential role and rationale for treatment of heart failure with sodium-glucose co-transporter 2 inhibitors. Eur J Heart Fail. 2017;19(11):1390–400. Study showing reduction in plasma volume via SGLT2i
Inoue BH, dos Santos L, Pessoa TD, Antonio EL, Pacheco BP, Savignano FA, et al. Increased NHE3 abundance and transport activity in renal proximal tubule of rats with heart failure. Am J Phys Regul Integr Comp Phys. 2012;302(1):R166–74.
Lütken SC, Kim SW, Jonassen T, Marples D, Knepper MA, Kwon TH, et al. Changes of renal AQP2, ENaC, and NHE3 in experimentally induced heart failure: response to angiotensin II AT1 receptor blockade. Am J Physiol Ren Physiol. 2009;297(6):F1678–88.
Yokoyama H, Gunasegaram S, Harding SE, Avkiran M. Sarcolemmal Na+/H+ exchanger activity and expression in human ventricular myocardium. J Am Coll Cardiol. 2000;36(2):534–40.
Nakamura TY, Iwata Y, Arai Y, Komamura K, Wakabayashi S. Activation of Na+/H+ exchanger 1 is sufficient to generate Ca2+ signals that induce cardiac hypertrophy and heart failure. Circ Res. 2008;103(8):891–9.
Baartscheer A, Schumacher CA, van Borren MM, Belterman CN, Coronel R, Opthof T, et al. Chronic inhibition of Na+/H+−exchanger attenuates cardiac hypertrophy and prevents cellular remodeling in heart failure. Cardiovasc Res. 2005;65(1):83–92.
Darmellah A, Baetz D, Prunier F, Tamareille S, Rücker-Martin C, Feuvray D. Enhanced activity of the myocardial Na+/H+ exchanger contributes to left ventricular hypertrophy in the Goto-Kakizaki rat model of type 2 diabetes: critical role of Akt. Diabetologia. 2007;50(6):1335–44.
Engelhardt S, Hein L, Keller U, Klämbt K, Lohse MJ. Inhibition of Na(+)-H(+) exchange prevents hypertrophy, fibrosis, and heart failure in beta(1)-adrenergic receptor transgenic mice. Circ Res. 2002;90(7):814–9.
• Baartscheer A, Schumacher CA, Wüst RC, Fiolet JW, Stienen GJ, Coronel R, et al. Empagliflozin decreases myocardial cytoplasmic Na. Diabetologia. 2017;60(3):568–73. Study showing improved cardiac energetics via empagliflozin
• Uthman L, Baartscheer A, Bleijlevens B, Schumacher CA, JWT F, Koeman A, et al. Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na. Diabetologia. 2018;61(3):722–6. Study showing improved cardiac energetics via multiple SGLT2i agents.
• National Institutes of Health. Empagliflozin outcome trial in patients with chronic heart failure with reduced ejection fraction (EMPEROR-Reduced). https://clinicaltrials.gov/ct2/show/NCT03057977. Accessed 24 Mar 2018. Active ongoing trial of empagliflozin in heart failure.
• National Institutes of Health. Study to Evaluate the Effect of Dapagliflozin on the Incidence of Worsening Heart Failure or Cardiovascular Death in Patients with Chronic Heart Failure (Data-HF). https://clinicaltrials.gov/ct2/show/NCT03036124. Accessed 24 Mar 2018. Active ongoing trial of dapagliflozin in heart failure.
Mudaliar S, Alloju S, Henry RR. Can a shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG OUTCOME study? A unifying hypothesis. Diabetes Care. 2016;39(7):1115–22.
Mather KJ, Hutchins GD, Perry K, Territo W, Chisholm R, Acton A, et al. Assessment of myocardial metabolic flexibility and work efficiency in human type 2 diabetes using 16-[18F]fluoro-4-thiapalmitate, a novel PET fatty acid tracer. Am J Physiol Endocrinol Metab. 2016;310(6):E452–60.
Young ME, McNulty P, Taegtmeyer H. Adaptation and maladaptation of the heart in diabetes: part II: potential mechanisms. Circulation. 2002;105(15):1861–70.
Levelt E, Rodgers CT, Clarke WT, Mahmod M, Ariga R, Francis JM, et al. Cardiac energetics, oxygenation, and perfusion during increased workload in patients with type 2 diabetes mellitus. Eur Heart J. 2016;37(46):3461–9.
Sato K, Kashiwaya Y, Keon CA, Tsuchiya N, King MT, Radda GK, et al. Insulin, ketone bodies, and mitochondrial energy transduction. FASEB J. 1995;9(8):651–8.
• Ye Y, Bajaj M, Yang HC, Perez-Polo JR, Birnbaum Y. SGLT-2 inhibition with dapagliflozin reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further augmentation of the effects with saxagliptin, a DPP4 inhibitor. Cardiovasc Drugs Ther. 2017;31(2):119–32. Study to evaluate mechanistic effects of dapagliflozin on cardiac remodeling and fibrosis
Lin B, Koibuchi N, Hasegawa Y, Sueta D, Toyama K, Uekawa K, et al. Glycemic control with empagliflozin, a novel selective SGLT2 inhibitor, ameliorates cardiovascular injury and cognitive dysfunction in obese and type 2 diabetic mice. Cardiovasc Diabetol. 2014;13:148.
Tosaki T, Kamiya H, Himeno T, Kato Y, Kondo M, Toyota K, et al. Sodium-glucose co-transporter 2 inhibitors reduce the abdominal visceral fat area and may influence the renal function in patients with type 2 diabetes. Intern Med. 2017;56(6):597–604.
Tahara A, Kurosaki E, Yokono M, Yamajuku D, Kihara R, Hayashizaki Y, et al. Effects of SGLT2 selective inhibitor ipragliflozin on hyperglycemia, hyperlipidemia, hepatic steatosis, oxidative stress, inflammation, and obesity in type 2 diabetic mice. Eur J Pharmacol. 2013;715(1–3):246–55.
Shigiyama F, Kumashiro N, Miyagi M, Ikehara K, Kanda E, Uchino H, et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with early-stage type 2 diabetes mellitus: DEFENCE study. Cardiovasc Diabetol. 2017;16(1):84.
Solini A, Giannini L, Seghieri M, Vitolo E, Taddei S, Ghiadoni L, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16(1):138.
Han JH, Oh TJ, Lee G, Maeng HJ, Lee DH, Kim KM, et al. The beneficial effects of empagliflozin, an SGLT2 inhibitor, on atherosclerosis in ApoE. Diabetologia. 2017;60(2):364–76.
Leng W, Ouyang X, Lei X, Wu M, Chen L, Wu Q, et al. The SGLT-2 inhibitor dapagliflozin has a therapeutic effect on atherosclerosis in diabetic ApoE. Mediat Inflamm. 2016;2016:6305735.
Nakatsu Y, Kokubo H, Bumdelger B, Yoshizumi M, Yamamotoya T, Matsunaga Y, et al. The SGLT2 inhibitor luseogliflozin rapidly normalizes aortic mRNA levels of inflammation-related but not lipid-metabolism-related genes and suppresses atherosclerosis in diabetic ApoE KO mice. Int J Mol Sci. 2017;18(8)
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344(8934):1383–9.
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425–35.
Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333(20):1301–7.
Tanaka A, Murohara T, Taguchi I, Eguchi K, Suzuki M, Kitakaze M, et al. Rationale and design of a multicenter randomized controlled study to evaluate the preventive effect of ipragliflozin on carotid atherosclerosis: the PROTECT study. Cardiovasc Diabetol. 2016;15(1):133.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91.
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the collaborative atorvastatin diabetes study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364(9435):685–96.
Association AD. Standards of medical care in diabetes—2007. Diabetes Care. 2007;30(Suppl 1):S4–S41.
• Rosenstock J, Chuck L, González-Ortiz M, Merton K, Craig J, Capuano G, et al. Initial combination therapy with canagliflozin plus metformin versus each component as monotherapy for drug-naïve type 2 diabetes. Diabetes Care. 2016;39(3):353–62. Study with evidence of non-inferiority of canagliflozin compared to metformin in glycemic control
UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854–65.
Griffin SJ, Leaver JK, Irving GJ. Impact of metformin on cardiovascular disease: a meta-analysis of randomised trials among people with type 2 diabetes. Diabetologia. 2017;60(9):1620–9.
Yancy CW, Januzzi JL, Allen LA, Butler J, Davis LL, Fonarow GC, et al. 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71(2):201–30.
GoodRx, Inc. SGLT2 Inhibitors. https://www.goodrx.com/sglt2-inhibitors. Accessed 27 Mar 2018.
Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334(7588):299.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
American Diabetes Association. Standards of Medical Care in Diabetes-2016: Summary of Revisions. Diabetes Care. 2016;39(Suppl 1):S4–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Xiaoming Jia, Paras B. Mehta, and Mahboob Alam declare that they have no conflict of interest.
Yumei Ye reports grants from AstraZeneca and Boehringer-Ingelheim.
Yochai Birnbaum reports grants from AstraZeneca and Boehringer-Ingelheim.
Mandeep Bajaj reports grants from Amylin, AstraZeneca, Boehringer-Ingelheim, Eli Lilly, Sanofi-Aventis, and Novo Nordisk.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Therapies and New Technologies in the Treatment of Diabetes
Rights and permissions
About this article
Cite this article
Jia, X., Mehta, P.B., Ye, Y. et al. SGLT2 Inhibitors and Cardiovascular Outcomes: Current Perspectives and Future Potentials. Curr Diab Rep 18, 63 (2018). https://doi.org/10.1007/s11892-018-1038-9
Published:
DOI: https://doi.org/10.1007/s11892-018-1038-9