Abstract
Purpose of Review
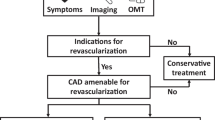
The purpose of this review is to examine current evidence on the benefit of chronic total occlusion (CTO) revascularization in patients with ischemic cardiomyopathy and propose a systematic approach on how and when to accomplish revascularization in these patients.
Recent Findings
Coronary revascularization in patients with reduced ejection fraction (EF) is advocated for to improve left ventricular function and consequently clinical outcomes. Approximately 16–31% of angiograms in patients with advanced CAD are noted to have a concomitant coronary CTO. Its presence is a main predictor of worse outcomes. Over the past 15 years, advancements in interventional technologies and techniques have made it possible to treat CTO lesions percutaneously with success rates exceeding 90%.
Summary
Different revascularization techniques have been organized into widely used algorithms for systematic CTO lesion crossing and treatment. Patients with reduced EF can be revascularized percutaneously with goal of complete functional revascularization. However, randomized prospective data is needed to justify the increased patient risks and healthcare costs associated with these procedures.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet (London, England). 2003;361(9351):13–20.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2016;67(10):1235–50.
Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–619.
Patel KV, Pandey A, de Lemos JA. Conceptual framework for addressing residual atherosclerotic cardiovascular disease risk in the era of precision medicine. Circulation. 2018;137(24):2551–3.
Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59(11):991–7.
• Jeroudi OM, Alomar ME, Michael TT, El Sabbagh A, Patel VG, Mogabgab O, et al. Prevalence and management of coronary chronic total occlusions in a tertiary Veterans Affairs hospital. Catheter Cardiovasc Interv. 2014;84(4):637–43 This paper demosntrates that in a contemporary veteran population, coronary CTOs are highly prevalent and are associated with more extensive comorbidities and higher likelihood for CABG referral.
Ramunddal T, Hoebers LP, Henriques JP, Dworeck C, Angeras O, Odenstedt J, et al. Chronic total occlusions in Sweden—a report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). PLoS One. 2014;9(8):e103850.
Di Mario C, Werner GS, Sianos G, Galassi AR, Buttner J, Dudek D, et al. European perspective in the recanalisation of chronic total occlusions (CTO): consensus document from the EuroCTO Club. EuroIntervention. 2007;3(1):30–43.
• Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61(3):282–94 This paper demonstrates and highlights the importance of incomplete revascualrization. Within the PCI and CABG arms of the all-comers SYNTAX trial, angiographically determined incomplete revascualrization has a detrimental impact on long-term clinical outcomes, including mortality. This effect remained consistent in patients with and without CTOs.
Christopoulos G, Karmpaliotis D, Alaswad K, Yeh RW, Jaffer FA, Wyman RM, et al. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter US registry. Int J Cardiol. 2015;198:222–8.
Wilson WM, Walsh SJ, Yan AT, Hanratty CG, Bagnall AJ, Egred M, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102(18):1486–93.
•• Tajti P, Burke MN, Karmpaliotis D, Alaswad K, Werner GS, Azzalini L, et al. Update in the percutaneous management of coronary chronic total occlusions. J Am Coll Cardiol Intv. 2018;11(7):615–25 In this review the authors summarize the latest publications in CTO PCI and provide an overview of the current state of the field.
Azzalini L, Jolicoeur EM, Pighi M, Millan X, Picard F, Tadros VX, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. 2016;118(8):1128–35.
• Patel MR, Calhoon JH, Dehmer GJ, Grantham JA, Maddox TM, Maron DJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Nucl Cardiol. 2017;24(5):1759–92 This paper summarized the methodology used to determine the approriateness of coronary revascularization. It also describes the appropriate use and inappropriate use of percutaneous revascualrization in most clinical scenarios including intervention in CTO lesions.
Ong AT, Serruys PW. Complete revascularization: coronary artery bypass graft surgery versus percutaneous coronary intervention. Circulation. 2006;114(3):249–55.
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):e44–e164.
Tarakji KG, Brunken R, McCarthy PM, Al-Chekakie MO, Abdel-Latif A, Pothier CE, et al. Myocardial viability testing and the effect of early intervention in patients with advanced left ventricular systolic dysfunction. Circulation. 2006;113(2):230–7.
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949–3003.
Alderman EL, Fisher LD, Litwin P, Kaiser GC, Myers WO, Maynard C, et al. Results of coronary artery surgery in patients with poor left ventricular function (CASS). Circulation. 1983;68(4):785–95.
O’Connor CM, Velazquez EJ, Gardner LH, Smith PK, Newman MF, Landolfo KP, et al. Comparison of coronary artery bypass grafting versus medical therapy on long-term outcome in patients with ischemic cardiomyopathy (a 25-year experience from the Duke Cardiovascular Disease Databank). Am J Cardiol. 2002;90(2):101–7.
Phillips HR, O’Connor CM, Rogers J. Revascularization for heart failure. Am Heart J. 2007;153(4 Suppl):65–73.
Tsuyuki RT, Shrive FM, Galbraith PD, Knudtson ML, Graham MM. Revascularization in patients with heart failure. CMAJ: Can Med Assoc J. 2006;175(4):361–5.
•• Cardona M, Martin V, Prat-Gonzalez S, Ortiz JT, Perea RJ, de Caralt TM, et al. Benefits of chronic total coronary occlusion percutaneous intervention in patients with heart failure and reduced ejection fraction: insights from a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson. 2016;18(1):78 This is one of the very few studies evaluating the potential role of CTO revascularization in patient with reduced ejection fraction.
Sapontis J, Salisbury AC, Yeh RW, Cohen DJ, Hirai T, Lombardi W, et al. Early procedural and health status outcomes after chronic total occlusion angioplasty: a report from the OPEN-CTO registry (outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures). JACC Cardiovasc Interv. 2017;10(15):1523–34.
Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–21.
Christopoulos G, Kandzari DE, Yeh RW, Jaffer FA, Karmpaliotis D, Wyman MR, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc Interv. 2016;9(1):1–9.
• Brilakis ES, Grantham JA, Rinfret S, Wyman RM, Burke MN, Karmpaliotis D, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5(4):367–79 This paper describes for the first time in detail a step by step, progressive, and sequential approach to treat and increased success rate to percutaneous intervention to CTOs.
Harding SA, Wu EB, Lo S, Lim ST, Ge L, Chen JY, et al. A new algorithm for crossing chronic total occlusions from the Asia Pacific chronic total occlusion club. JACC Cardiovasc Interv. 2017;10(21):2135–43.
Colombo A, Mikhail GW, Michev I, Iakovou I, Airoldi F, Chieffo A, et al. Treating chronic total occlusions using subintimal tracking and reentry: the STAR technique. Catheter Cardiovasc Interv. 2005;64(4):407–11 discussion 12.
Surmely JF, Tsuchikane E, Katoh O, Nishida Y, Nakayama M, Nakamura S, et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006;18(7):334–8.
Galassi AR, Sianos G, Werner GS, Escaned J, Tomasello SD, Boukhris M, et al. Retrograde recanalization of chronic total occlusions in Europe: procedural, in-hospital, and long-term outcomes from the multicenter ERCTO registry. J Am Coll Cardiol. 2015;65(22):2388–400.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19.
Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, et al. Association of the hospital readmissions reduction program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol. 2018;3(1):44–53.
Emond M, Mock MB, Davis KB, Fisher LD, Holmes DR Jr, Chaitman BR, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1994;90(6):2645–57.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975.
Baker DW, Jones R, Hodges J, Massie BM, Konstam MA, Rose EA. Management of heart failure. III. The role of revascularization in the treatment of patients with moderate or severe left ventricular systolic dysfunction. JAMA. 1994;272(19):1528–34.
• Carson P, Wertheimer J, Miller A, O’Connor CM, Pina IL, Selzman C, et al. The STICH trial (Surgical Treatment for Ischemic Heart Failure): mode-of-death results. JACC Heart Fail. 2013;1(5):400–8 This is the largest contemporary randomized study demonstrating the benefit of coronary revascularization in patients with reduced left ventricular ejection fraction compared with optimal medical treatment.
Iqbal MB, Smith RD, Lane R, Patel N, Mattar W, Kabir T, et al. The prognostic significance of incomplete revascularization and untreated coronary anatomy following percutaneous coronary intervention: an analysis of 6,755 patients with multivessel disease. Catheter Cardiovasc Interv. 2018;91(7):1229–39.
Hannan EL, Zhong Y, Berger PB, Jacobs AK, Walford G, Ling FSK, et al. Association of coronary vessel characteristics with outcome in patients with percutaneous coronary interventions with incomplete revascularization. JAMA Cardiol. 2018;3(2):123–30.
Stewart RA, Szalewska D, She L, Lee KL, Drazner MH, Lubiszewska B, et al. Exercise capacity and mortality in patients with ischemic left ventricular dysfunction randomized to coronary artery bypass graft surgery or medical therapy: an analysis from the STICH trial (Surgical Treatment for Ischemic Heart Failure). JACC Heart Fail. 2014;2(4):335–43.
Jones EL, Weintraub WS. The importance of completeness of revascularization during long-term follow-up after coronary artery operations. J Thorac Cardiovasc Surg. 1996;112(2):227–37.
Bell MR, Gersh BJ, Schaff HV, Holmes DR Jr, Fisher LD, Alderman EL, et al. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1992;86(2):446–57.
Rizzello V, Poldermans D, Biagini E, Schinkel AF, Boersma E, Boccanelli A, et al. Prognosis of patients with ischaemic cardiomyopathy after coronary revascularisation: relation to viability and improvement in left ventricular ejection fraction. Heart. 2009;95(15):1273–7.
Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol. 2002;39(7):1151–8.
Pagley PR, Beller GA, Watson DD, Gimple LW, Ragosta M. Improved outcome after coronary bypass surgery in patients with ischemic cardiomyopathy and residual myocardial viability. Circulation. 1997;96(3):793–800.
Senior R, Kaul S, Lahiri A. Myocardial viability on echocardiography predicts long-term survival after revascularization in patients with ischemic congestive heart failure. J Am Coll Cardiol. 1999;33(7):1848–54.
Schinkel AF, Poldermans D, Elhendy A, Bax JJ. Assessment of myocardial viability in patients with heart failure. J Nucl Med. 2007;48(7):1135–46.
Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607–16.
Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511–20.
•• Galassi AR, Boukhris M, Toma A, Elhadj Z, Laroussi L, Gaemperli O, et al. Percutaneous coronary intervention of chronic total occlusions in patients with low left ventricular ejection fraction. JACC Cardiovasc Interv. 2017;10(21):2158–70 With the caveat of being a small study, this is the first randomied study showing a benefit of opening a CTO in patients with reduced LVEF.
Safley DM, Grantham JA, Hatch J, Jones PG, Spertus JA. Quality of life benefits of percutaneous coronary intervention for chronic occlusions. Catheter Cardiovasc Interv. 2014;84(4):629–34.
Wijeysundera HC, Norris C, Fefer P, Galbraith PD, Knudtson ML, Wolff R, et al. Relationship between initial treatment strategy and quality of life in patients with coronary chronic total occlusions. EuroIntervention. 2014;9(10):1165–72.
Mashayekhi K, Neuser H, Kraus A, Zimmer M, Dalibor J, Akin I, et al. Successful percutaneous coronary intervention improves cardiopulmonary exercise capacity in patients with chronic total occlusions. J Am Coll Cardiol. 2017;69(8):1095–6.
Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, Rangan BV, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115(10):1367–75.
Toma A, Stahli BE, Gick M, Gebhard C, Kaufmann BA, Mashayekhi K, et al. Comparison of benefit of successful percutaneous coronary intervention for chronic total occlusion in patients with versus without reduced (≤40%) left ventricular ejection fraction. Am J Cardiol. 2017;120(10):1780–6.
Claessen BE, van der Schaaf RJ, Verouden NJ, Stegenga NK, Engstrom AE, Sjauw KD, et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009;2(11):1128–34.
Claessen BE, Dangas GD, Weisz G, Witzenbichler B, Guagliumi G, Mockel M, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J. 2012;33(6):768–75.
Tajstra M, Pyka L, Gorol J, Pres D, Gierlotka M, Gadula-Gacek E, et al. Impact of chronic total occlusion of the coronary artery on long-term prognosis in patients with ischemic systolic heart failure: insights from the COMMIT-HF registry. JACC Cardiovasc Interv. 2016;9(17):1790–7.
Fefer P, Gannot S, Kochkina K, Maor E, Matetzky S, Raanani E, et al. Impact of coronary chronic total occlusions on long-term mortality in patients undergoing coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2014;18(6):713–6.
Konstanty-Kalandyk J, Bartus K, Piatek J, Kedziora A, Darocha T, Bryniarski KL, et al. Is right coronary artery chronic total vessel occlusion impacting the surgical revascularization results of patients with multivessel disease? A retrospective study. PeerJ. 2018;6:e4909.
Pereg D, Fefer P, Samuel M, Shuvy M, Deb S, Sparkes JD, et al. Long-term follow-up of coronary artery bypass patients with preoperative and new postoperative native coronary artery chronic total occlusion. Can J Cardiol. 2016;32(11):1326–31.
van Dongen IM, Yilmaz D, Elias J, Claessen BEPM, Delewi R, Knops RE, et al. Evaluation of the impact of a chronic total coronary occlusion on ventricular arrhythmias and long-term mortality in patients with ischemic cardiomyopathy and an implantable cardioverter-defibrillator (the eCTOpy-in-ICD Study). J Am Heart Assoc. 2018;7(10). https://doi.org/10.1161/JAHA.118.008609.
Nombela-Franco L, Iannaccone M, Anguera I, Amat-Santos IJ, Sanchez-Garcia M, Bautista D, et al. Impact of chronic total coronary occlusion on recurrence of ventricular arrhythmias in ischemic secondary prevention implantable cardioverter-defibrillator recipients (VACTO secondary study): insights from coronary angiogram and electrogram analysis. JACC Cardiovasc Interv. 2017;10(9):879–88.
Rizzello V, Schinkel AF, Bax JJ, Boersma E, Bountioukos M, Vourvouri EC, et al. Individual prediction of functional recovery after coronary revascularization in patients with ischemic cardiomyopathy: the scar-to-biphasic model. Am J Cardiol. 2003;91(12):1406–9.
Danek BA, Basir MB, O’Neill WW, Alqarqaz M, Karatasakis A, Karmpaliotis D, et al. Mechanical circulatory support in chronic total occlusion percutaneous coronary intervention: insights from a multicenter U.S. registry. J Invasive Cardiol. 2018;30(3):81–7.
Yamada S, Kamiya K, Kono Y. Frailty may be a risk marker for adverse outcome in patients with congestive heart failure. ESC Heart Fail. 2015;2(3):168–70.
Denfeld QE, Winters-Stone K, Mudd JO, Gelow JM, Kurdi S, Lee CS. The prevalence of frailty in heart failure: a systematic review and meta-analysis. Int J Cardiol. 2017;236:283–9.
Madan SA, Fida N, Barman P, Sims D, Shin J, Verghese J, et al. Frailty assessment in advanced heart failure. J Card Fail. 2016;22(10):840–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nayef A. Abouzaki, Jose E. Exaire, and Luis A. Guzmán declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Abouzaki, N.A., Exaire, J.E. & Guzmán, L.A. Role of Percutaneous Chronic Total Occlusion Interventions in Patients with Ischemic Cardiomyopathy and Reduced Left Ventricular Ejection Fraction. Curr Cardiol Rep 20, 124 (2018). https://doi.org/10.1007/s11886-018-1066-8
Published:
DOI: https://doi.org/10.1007/s11886-018-1066-8