Abstract
Purpose of Review
Spinal cord injuries are a well-known cause of neurogenic bladder in children. The aim of this review is to bring the reader up to date on the management of neurogenic bladder in patients with spinal cord injuries.
Recent Findings
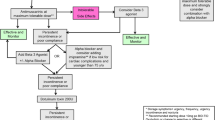
After spinal shock resolution, the most common treatments are anticholinergic medications and intermittent catheterization. Alpha-adrenergic blockers and beta-agonists are the other available medical therapies. Nonetheless, surgery is an alternative when medical treatment alone fails. Slings and urinary sphincters aim to increase bladder outlet resistance, while bladder augmentations increase continence and promote safe storage pressures.
Summary
Initially, spinal cord injuries cause spinal shock and bladder atony. For this reason, acute management involves adequate bladder emptying with catheterization. Catheterization is essential to protect renal function during the spinal shock phase. Similarly, long-term management also focuses on protecting renal function. However, long-term management should also aim to optimize bladder capacity and pressure, achieve continence, and prevent complications. Several medical and surgical management options are safe and effective for treating neurogenic bladder. Improving the quality of life and considering patient preferences are essential components to treating neurogenic bladder in children.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ginsberg DA, Boone TB, Cameron AP, Gousse A, Kaufman MR, Keays E, et al. The AUA/SUFU guideline on adult neurogenic lower urinary tract dysfunction: diagnosis and evaluation. J Urol NLM (Medline). 2021;206:1097–105.
Bauer SB. Neurogenic bladder: etiology and assessment. Pediatr Nephrol. 2008;23:541–51.
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O KC, et al. Traumatic spinal cord injury in the United States. The Journal of the American Medical Association [Internet]. 2015;313:2236–43. Available from: https://jamanetwork.com/
Chen Y, Tang Y, Vogel LC, DeVivo MJ. Causes of spinal cord injury. Top Spinal Cord Inj Rehabil [Internet]. 2013;19:1–8. Available from: https://www.thomasland.com
Parent S, Mac-Thiong J-M, Roy-Beaudry M, Sosa JF, Labelle H. Spinal cord injury in the pediatric population: a systematic review of the literature. J Neurotrauma. 2011;28:1515–24.
Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013;19.
Ziu E, Mesfin FB. Spinal Shock - StatPearls - NCBI Bookshelf [Internet]. Spinal Shock. 2022 [cited 2022 Jun 19]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448163/
Welk B, Schneider MP, Thavaseelan J, Traini LR, Curt A, Kessler TM. Early urological care of patients with spinal cord injury. World J Urol Springer Verlag. 2018;36:1537–44.
Lucas E. Medical management of neurogenic bladder for children and adults: a review. Top Spinal Cord Inj Rehabil [Internet]. 2019;25:195–204. Available from: https://www.thomasland.com
Eswara JR, Castellan M, González R, Mendieta N, Cendron M. The urological management of children with spinal cord injury. World Journal of Urology Springer Verlag. 2018;36:1593–601.
Koff SA. Estimating bladder capacity in children. Urology. 1983;21:248.
Nijman RJM. Urodynamic studies of the lower urinary tract. Pediatric Urology. Elsevier; 2010. p. 127–40.
Cheol Shin J, Lee Y, Yang H, Hyun Kim D. Clinical significance of urodynamic study parameters in maintenance of renal function in spinal cord injury patients. 2014; Available from: https://doi.org/10.5535/arm.2014.38.3.353
McGuire EJ, Woodside JR, Borden TA, Weiss RM. Prognostic value of urodynamic testing in myelodysplastic patients. J Urol. 1981;126:205–9.
Wilson DA, Prince JR. MR Imaging determination of the location of the normal conus medullaris throughout childhood. Am J Neuroradiol. 1989;10:259–62.
Samson G, Cardenas DD. Neurogenic bladder in spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18:255–74.
Welk B, Lenherr S, Elliott S, Stoffel J, Presson AP, Zhang C, et al. The Neurogenic Bladder Symptom Score (NBSS): a secondary assessment of its validity, reliability among people with a spinal cord injury. Spinal Cord [Internet]. 2018;56:259–64. Available from: https://doi.org/10.1038/s41393-017-0028-0
Sturm RM, Cheng EY. The management of the pediatric neurogenic bladder. Curr Bladder Dysfunct Rep. 2016;11:225–33.
Abrams P, Agarwal M, Drake M, El-Masri W, Fulford S, Reid S, et al. A proposed guideline for the urological management of patients with spinal cord injury. BJU Int. 2008;101:989–94.
Alexander MA, Matthews DJ. Pediatric rehabilitation: principles and practice [Internet]. 5th ed. New York: Demos Medical Publishing; 2015 [cited 2022 Jun 19]. Available from: https://www.demosmedical.com
Weld KJ, Dmochowski RR. Effect of bladder management on urological complications in spinal cord injured patients. J Urol. 2000;163:768–72.
Generao SE, Dall’Era JP, Stone AR, Kurzrock EA. Spinal cord injury in children: long-term urodynamic and urological outcomes. Journal of Urology. Lippincott Williams and Wilkins; 2004;172:1092–4. Retrospectively reviewed pediatric cases of SCI and identified age of injury, mechanism of injury and bladder management strategy.
Schottler J, Vogel LC, Sturm P. Spinal cord injuries in young children: a review of children injured at 5 years of age and younger. Dev Med Child Neurol. 2012;54:1138–43.
Chao R, Mayo ME. Long-term urodynamic follow up in pediatric spinal cord injury. Paraplegia. 1994;32:806–9.
Fortin A, Morin V, Ramsay S, Gervais P, Bolduc S, Frcsc MD. Adherence to antimuscarinics in children with overactive bladder. 2017;255–8. Available from: https://academic.oup.com/pch/article/22/5/255/3829186
Noh JW, Lee B, Kim JH. Efficacy and safety of anticholinergics for children or adolescents with idiopathic overactive bladder: systematic review and meta-analysis. Int Urol Nephrol [Internet]. Int Urol Nephrol; 2019 [cited 2022 Jun 28];51:1459–71. Available from: https://pubmed.ncbi.nlm.nih.gov/31243632/
Veenboer PW, Huisman J, Chrzan RJ, Kuijper CF, Dik P, de Kort LMO, et al. Behavioral effects of long-term antimuscarinic use in patients with spinal dysraphism: a case control study. J Urol. Elsevier Inc.; 2013;190:2228–32.
Wöllner J, Pannek J. Initial experience with the treatment of neurogenic detrusor overactivity with a new beta-3 agonist (mirabegron) in patients with spinal cord injury. International Spinal Cord Society [Internet]. 2016;54:78–82. Available from: https://www.nature.com/sc
Blais A-S, Nadeau G, Moore K, Genois L, Bolduc S. Prospective pilot study of mirabegron in pediatric patients with overactive bladder. Eur Urol. 2016;70:9–13.
Kareem DA, Hassan OA. The role of alpha blockers in the treatment of children with voiding dysfunction. Iraqui Postgrad Med J. 2016;15.
al Taweel W, Seyam R. Neurogenic bladder in spinal cord injury patients. Research and Reports in Urology [Internet]. 2015;7–85. Available from: https://doi.org/10.2147/RRU.S29644
Holmes NM, Kogan BA, Baskin LS. Placement of artificial urinary sphincter in children and simultaneous gastrocystoplasty. The Journal of Urology. 2001;2366–8.
Li G-P, Wang X-Y, Zhang Y. Efficacy and safety of OnabotulinumtoxinA in patients with neurogenic detrusor overactivity caused by spinal cord injury: a systematic review and meta-analysis. Int Neurourol J. 2018;22:275–86.
Schurch B, Schulte-Baukloh H. Botulinum toxin in the treatment of neurogenic bladder in adults and children. Eur Urol Suppl. 2006;5:679–84.
Akbar M, Abel R, Seyler TM, Gerner HJ, Möhring K. Repeated botulinum-A toxin injections in the treatment of myelodysplastic children and patients with spinal cord injuries with neurogenic bladder dysfunction. BJU Int. 2007;100:639–45.
Greer T, Abbott J, Breytenbach W, McGuane D, Barker A, Khosa J, et al. Ten years of experience with intravesical and intrasphincteric onabotulinumtoxinA in children. Journal of Pediatric Urology. 2016;12:94.e1–94.e6. Demonstrated that intravesical Botox remained effective in response quality and response time in children up to an eleventh injection.
Bennett CJ, Bennett JK. Augmentation cystoplasty and urinary diversion in patients with spinal cord injury. Phys Med Rehabil Clin N Am. 1993;4:377–89.
Rhee AC, Yerkes EB, Rink RC. Incontinent and continent urinary diversion. Pediatric Surgery. Mosby; 2012;1487–96.
Gurung PMS, Attar KH, Abdul-Rahman A, Morris T, Hamid R, Julian P, et al. Long-term outcomes of augmentation ileocystoplasty in patients with spinal cord injury: a minimum of 10 years of follow-up. BJU Int. 2012;109:1236–42.
Mills RD, Studer UE. Metabolic consequences of continent urinary diversion. J Urol. 1999;161:1057–66.
Maldonado N, Michel J, Barnes K. Thirty-day hospital readmissions after augmentation cystoplasty: a nationwide readmissions database analysis. J Pediatr Urol. 2018;14:533.e1–533.e9. Maldonado et al. determined the rate, causes, risk factors, and costs associated with 30-day readmissions for children undergoing augmentation cystoplasty.
Husmann DA. Long-term complications following bladder augmentations in patients with spina bifida: bladder calculi, perforation of the augmented bladder and upper tract deterioration. Transl Androl Urol [Internet]. AME Publications; 2016 [cited 2022 Jun 30];5:3. Available from: /pmc/articles/PMC4739984/
Best KL, Ethans K, Craven BC, Noreau L, Hitzig SL. Identifying and classifying quality of life tools for neurogenic bladder function after spinal cord injury: a systematic review. https://doi.org/101080/1079026820161226700 [Internet]. Taylor & Francis; 2016 [cited 2022 Jun 30];40:505–29. Available from: https://doi.org/10.1080/10790268.2016.1226700
Hwang M, Zebracki K, Lawrence VC, Mulcahey MJ, Varni JW. Development of the Pediatric Quality of Life InventoryTM Spinal Cord Injury (PedsQLTM SCI) module: qualitative methods. Spinal Cord [Internet]. 2020;58:1134–42. Available from: https://doi.org/10.1038/s41393-020-0450-6
Garma SI, Kelly EH, Daharsh EZ, Vogel LC. Health-related quality of life after pediatric spinal cord injury. Available from: https://academic.oup.com/jpepsy/article/36/2/226/890960
Shalaby MS, Gibson A, Granitsiotis P, Conn G, Cascio S. Assessment of the introduction of an adolescent transition urology clinic using a validated questionnaire. J Pediatr Urol. 2015;11:89.e1–89.e5. Reported that the transition of adolescents with complex urological conditions to adult urology clinic is beneficial in addressing the patients’ needs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Neurogenic Bladder
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suria Cordero, N.F., Johnston, A.W. & Dangle, P.P. Optimal Management of Neurogenic Bladder due to Spinal Cord Injury in Pediatric Patients. Curr Bladder Dysfunct Rep 18, 71–77 (2023). https://doi.org/10.1007/s11884-022-00681-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-022-00681-4