Abstract
Purpose of Review
This goal of this review is to summarize the current literature on the diagnosis and evaluation of female urethral stricture.
Recent Findings
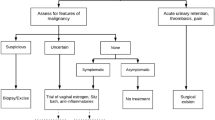
Female urethral stricture is a rare condition, which can present with a wide variety of symptoms, including both obstructive and irritative voiding symptoms, pain, or infection. Initial evaluation with post-void residual and uroflowmetry are good screening tests but are unable to diagnose stricture. Diagnosis often requires more than one modality, most commonly cystoscopy and voiding cystourethrogram, with or without urodynamics. Ultrasound is a newer diagnostic tool that can aid in diagnosis and surgical planning.
Summary
Female urethral stricture is a rare pathology and requires a high-clinical suspicion for accurate diagnosis. While there is a lack of consensus on clear diagnostic criteria, multiple modalities are often used to establish a diagnosis.


Similar content being viewed by others
Data Availability
N/A.
Code Availability
N/A.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Osman NI, Chapple CR. Contemporary surgical management of female urethral stricture disease. Curr Opin Urol. 2015;25:341–5.
Smith AL, Ferlise VJ, Rovner ES. Female urethral strictures: successful management with long-term clean intermittent catheterization after urethral dilatation. BJU Int. 2006;98:96–9.
Osman NI, Mangera A, Chapple CR. A systematic review of surgical techniques used in the treatment of female urethral stricture. Eur Urol. 2013;64:965–73.
West C, Lawrence A. Female urethroplasty: contemporary thinking. World J Urol. 2019;37:619–29.
Waterloos M, Verla W. Female urethroplasty: a practical guide emphasizing diagnosis and surgical treatment of female urethral stricture disease. BioMed Res Int. 2019;2019:e6715257.
Wessells H, Angermeier KW, Elliott S, et al. Male urethral stricture: American Urological Association Guideline. J Urol. 2017;197:182–90.
Spilotros M, Malde S, Solomon E, Grewal M, Mukhtar BM, Pakzad M, Hamid R, Ockrim JL, Greenwell TJ. Female urethral stricture: a contemporary series. World J Urol. 2017;35:991–5.
Hampson LA, Mcaninch JW, Breyer BN. Male urethral strictures and their management. Nat Rev Urol. 2014;11:43–50.
Agochukwu-Mmonu N, Srirangapatanam S, Cohen A, Breyer B. Female urethral strictures: review of diagnosis, etiology, and management. Curr Urol Rep. 2019;20:74.
•• Sarin I, Narain TA, Panwar VK, Bhadoria AS, Goldman HB, Mittal A. Deciphering the enigma of female urethral strictures: a systematic review and meta-analysis of management modalities. Neurourol Urodyn. 2021;40:65–79. Meta-analysis to identify the best diagnostic methods and surgical outcomes for female urethral strictures.
Faiena I, Koprowski C, Tunuguntla H. Female urethral reconstruction. J Urol. 2016;195:557–67.
Patel DN, Fok CS, Webster GD, Anger JT. Female urethral injuries associated with pelvic fracture: a systematic review of the literature. BJU Int. 2017;120:766–73.
Anast J, Brandes SB, Klutke C. Female urethral reconstruction. In: Brandes SB, editor. Urethral Reconstr. Surg. Totowa: Humana Press; 2008. p. 303–13.
Blaivas JG. Vaginal flap urethral reconstruction: an alternative to the bladder flap neourethra. J Urol. 1989;141:542–5.
Blaivas JG, Sandhu J. Urethral reconstruction after erosion of slings in women. Curr Opin Urol. 2004;14:335–8.
Heidari F, Abbaszadeh S, Ghadian A, Tehrani Kia F. On demand urethral dilatation versus intermittent urethral dilatation: results and complications in women with urethral stricture. Nephro-Urol Mon. 2014. https://doi.org/10.5812/numonthly.15212.
Santucci RA, Payne CK, Anger JT, Saigal CS, Urologic Diseases in America Project. Office dilation of the female urethra: a quality of care problem in the field of urology. J Urol. 2008;180:2068–75.
Brucker BM. Female urethral stricture. Rev Urol. 2018;20:174–6.
Blaivas JG, Santos JA, Tsui JF, Deibert CM, Rutman MP, Purohit RS, Weiss JP. Management of urethral stricture in women. J Urol. 2012;188:1778–82.
Meyrick Thomas RH, Ridley CM, McGibbon DH, Black MM. Lichen sclerosus et atrophicus and autoimmunity–a study of 350 women. Br J Dermatol. 1988;118:41–6.
Belsante MJ, Selph JP, Peterson AC. The contemporary management of urethral strictures in men resulting from lichen sclerosus. Transl Androl Urol. 2015;4:22–8.
Levy A, Browne B, Fredrick A, Stensland K, Bennett J, Sullivan T, Rieger-Christ KM, Vanni AJ. Insights into the pathophysiology of urethral stricture disease due to lichen sclerosus: comparison of pathological markers in lichen sclerosus induced strictures vs nonlichen sclerosus induced strictures. J Urol. 2019;201:1158–63.
Ackerman AL, Blaivas J, Anger JT. Female Urethral Reconstruction. Curr Bladder Dysfunct Rep. 2010;5:225–32.
Elliott CS. Female urethral stricture management: the initial experience of an female pelvic medicine and reconstructive surgery-trained urologist. Female Pelvic Med Reconstr Surg. 2020. https://doi.org/10.1097/SPV.0000000000000969.
• Kocadag H, Toia B, Axell R, Yasmin H, Pakzad MH, Hamid R, Greenwell TJ, Ockrim JL. A comparison of flow rate curve shape and video-urodynamic findings in women with lower urinary tract symptoms: can flow rate curve shape predict female bladder outflow obstruction or detrusor underactivity? World J Urol. 2020. https://doi.org/10.1007/s00345-020-03343-4. Retrospective study correlating uroflowmetry curves to types of bladder outlet obstruction, enhancing screening utility of uroflowmetry for urethral stricture.
• Sussman RD, Kozirovsky M, Telegrafi S, Peyronnet B, Palmerola R, Smilen S, Pape DM, Rosenblum N, Nitti VW, Brucker BM. Gel-infused translabial ultrasound in the evaluation of female urethral stricture. Female Pelvic Med Reconstr Surg. 2019. https://doi.org/10.1097/SPV.0000000000000699. Case series describing a novel technique for diagnosis female urethral stricture using gel-infused translabial ultrasound.
Winters JC, Dmochowski RR, Goldman HB, et al. Urodynamic studies in adults: AUA/SUFU guideline. J Urol. 2012;188:2464–72.
Marks BK, Goldman HB. Videourodynamics: indications and technique. Urol Clin North Am. 2014;41:383–91.
Lim CS, Abrams P. The Abrams-Griffiths nomogram. World J Urol. 1995;13:34–9.
Griffiths D, Höfner K, van Mastrigt R, Rollema HJ, Spångberg A, Gleason D. Standardization of terminology of lower urinary tract function: pressure-flow studies of voiding, urethral resistance, and urethral obstruction. International Continence Society Subcommittee on Standardization of Terminology of Pressure-Flow Studies. Neurourol Urodyn. 1997;16:1–18.
Massey JA, Abrams PH. Obstructed voiding in the female. Br J Urol. 1988;61:36–9.
Chassagne S, Bernier PA, Haab F, Roehrborn CG, Reisch JS, Zimmern PE. Proposed cutoff values to define bladder outlet obstruction in women. Urology. 1998;51:408–11.
• Solomon E, Yasmin H, Duffy M, Rashid T, Akinluyi E, Greenwell TJ. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourol Urodyn. 2018;37:368–378. Created and validated nomogram specifically for women with bladder outlet obstruction.
Hsiao S-M, Lin H-H, Kuo H-C. Videourodynamic studies of women with voiding dysfunction. Sci Rep. 2017;7:6845.
Santucci R, Chen M. Evaluation and treatment of female urethral stricture disease. Curr Bladder Dysfunct Rep. 2013;8:123–7.
Chaudhari VV, Patel MK, Douek M, Raman SS. MR imaging and US of female urethral and periurethral disease. Radiographics. 2010;30:1857–74.
Bhatt S, Goel M, Gupta A, Tandon A, Roy S. Diagnosis of urethral stricture on dynamic voiding transvaginal sonourethrography: a case report. J Diagn Med Sonogr. 2017;33:140–3.
Dwarkasing RS, Verschuuren SI, Leenders GJLH, Thomeer MGJ, Dohle GR, Krestin GP. Chronic lower urinary tract symptoms in women: classification of abnormalities and value of dedicated MRI for diagnosis. Am J Roentgenol. 2013;202:W59–66.
Surabhi VR, Menias CO, George V, Siegel CL, Prasad SR. Magnetic resonance imaging of female urethral and periurethral disorders. Radiol Clin N Am. 2013;51:941–53.
Aldamanhori R, Inman R. The treatment of complex female urethral pathology. Asian J Urol. 2018;5:160–3.
•• Lane GI, Smith AL, Stambakio H, et al. Treatment of urethral stricture disease in women: a multi-institutional collaborative project from the SUFU research network. Neurourol Urodyn. 2020;39:2433–2441. One of the largest, multi-institutional retrospective studies evaluating diagnosis, etiology and surgical management of urethral strictures.
Horbach SER, Bouman M-B, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of Vaginoplasty in Male-to-female transgenders: a systematic review of surgical techniques. J Sex Med. 2015;12:1499–512.
Waterloos M, Hollebosch S, Verla W, Spinoit A-F, Hoebeke P, Monstrey S, Lumen N. Neo-vaginal advancement flaps in the treatment of urethral strictures in transwomen. Urology. 2019;129:217–22.
Author information
Authors and Affiliations
Contributions
Joanna Marantidis performed the literature review and drafted the work. Rachael Sussman critically revised the work.
Corresponding author
Ethics declarations
Ethics Approval
N/A
Consent to Participate
N/A
Consent for Publication
N/A
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Voiding Dysfunction Evaluation
Rights and permissions
About this article
Cite this article
Marantidis, J., Sussman, R.D. Etiology and Evaluation of Female Urethral Strictures. Curr Bladder Dysfunct Rep 17, 13–19 (2022). https://doi.org/10.1007/s11884-021-00637-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-021-00637-0