Abstract
Purpose of Review
The goal of this study is to review current literature regarding the role of urodynamic studies (UDS) in evaluation of non-neurogenic patients with pelvic floor disorders of stress urinary incontinence (SUI), pelvic organ prolapse (POP), voiding dysfunction, and interstitial cystitis/bladder pain syndrome (IC/BPS).
Recent Findings
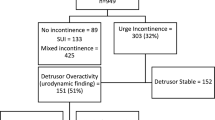
Rates of pre-operative UDS have decreased among women with SUI. Guidelines suggest UDS is not required for index SUI patients opting for surgical treatments. Non-index SUI patients are candidates for UDS testing if such objective information will better clarify symptomology or guide management decisions. Women undergoing POP repair should be evaluated for occult SUI via physical exam or UDS. Women with high grade POP may have associated LUTS which may impact outcomes. UDS can assist in developing adjunct treatments or guiding surgical repair. UDS should be considered in women with voiding dysfunction who fail empiric treatments.
Summary
UDS should be used judiciously, but may offer invaluable insights for symptom etiology and guide management for women with various pelvic floor disorders.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, et al. A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med. 2012;366(21):1987–97. https://doi.org/10.1056/NEJMoa1113595.
Malik RD, Hess DS, Carmel ME, Lemack GE, Zimmern PE. Prospective evaluation of urodynamic utility in a subspecialty tertiary practice. Urology. 2019;126:59–64. https://doi.org/10.1016/j.urology.2019.01.004.
•• Drake MJ, Doumouchtsis SK, Hashim H, Gammie A. Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations. Neurourol Urodyn. 2018;37(S6):S50–60. https://doi.org/10.1002/nau.23773Review of ICS recommendations for appropriate standard urodynamic testing and reporting.
McKinney T, Babin EA, Ciolfi V, McKinney CR, Shah N. Comparison of water and air charged transducer catheter pressures in the evaluation of cystometrogram and voiding pressure studies. Neurourol Urodyn. 2018;37(4):1434–40.
Chapple CHC, Patel A, MacDiarmid S. Urodynamics Made Easy. Amsterdam: Elsevier; 2018.
Yeung JY, Ma E, Pauls RN. Pain and embarrassment associated with urodynamic testing in women. Int Urogynecol J. 2014;25(5):645–50.
Rezvan A, Amaya S, Betson L, Yazdany T. Randomized controlled trial of the effect of environment on patient embarrassment and anxiety with urodynamics. Int Urogynecol J. 2017;29(2):291–6. https://doi.org/10.1007/s00192-017-3386-4.
McKee DC, Gonzalez EJ, Amundsen CL, Grill WM. Randomized controlled trial to assess the impact of high concentration Intraurethral Lidocaine on urodynamic voiding parameters. Urology. 2019;133:72–7. https://doi.org/10.1016/j.urology.2019.08.020.
Rosier P, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, et al. International continence society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017;36(5):1243–60.
Kathleen C. Kobashi M, FACS, FPMRS; Michael E. Albo, MD; Roger R. Dmochowski, MD; David A. Ginsberg, MD; Howard B. Goldman, MD; Alexander Gomelsky, MD; Stephen R. Kraus, MD, FACS; Jaspreet S. Sandhu, MD; Tracy Shepler; Jonathan R. Treadwell, PhD; Sandip Vasavada, MD; Gary E. Lemack, MD. Surgical treatment of female stress urinary incontinence (SUI): AUA/SUFU guideline. 2017. https://www.auanet.org/guidelines/stress-urinary-incontinence-(sui)-guideline. Accessed 1/15 2020.
van Leijsen SA, Kb K, Mol BWJ, Broekhuis SR, Milani AL, Bongers MY, et al. Can preoperative urodynamic investigation be omitted in women with stress urinary incontinence? A non-inferiority randomized controlled trial. Neurourol Urodyn. 2012;31(7):1118–23.
Committee on Gynecologic Practice A. Evaluation of uncomplicated stress urinary incontinence before surgical treatment. 2014. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Gynecologic-Practice/Evaluation-of-Uncomplicated-Stress-Urinary-Incontinence-in-Women-Before-Surgical-Treatment?IsMobileSet=false. Accessed 1/15 2020.
•• Lloyd J, Dielubanza E, Goldman HB. Trends in urodynamic testing prior to midurethral sling placement-What was the value of the VALUE trial? Neurourol Urodyn. 2018;37(3):1046–52 Retrospective study revealing downtrend in UDS evaluation prior to SUI treatment and impact on outcomes.
• Mengerink BB, Nelen W, van Leijsen SAL, Heesakkers J, KBL K, Karmakar D. De-implementation of urodynamics in The Netherlands after the VALUE/VUSIS-2 results: a nationwide survey. Int Urogynecol J. 2018;29(9):1279–80. https://doi.org/10.1007/s00192-018-3661Retrospective study revealing downtrend of UDS testing among specialists managing SUI in Netherlands.
Rubilotta E, Balzarro M, D'Amico A, Cerruto MA, Bassi S, Bovo C, et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC Urol. 2019;19(1):44. https://doi.org/10.1186/s12894-019-0468-2.
Serati M, Topazio L, Bogani G, Costantini E, Pietropaolo A, Palleschi G, et al. Urodynamics useless before surgery for female stress urinary incontinence: are you sure? Results from a multicenter single nation database. Neurourol Urodyn. 2016;35(7):809–12. https://doi.org/10.1002/nau.22804.
Sirls LT, Ritcher H, Litman HJ, Kenton K, Lemack GE, Lukacz ES, et al. The effect of urodynamic testing on clinical diagnosis, treatment plan and outcomes in women undergoing stress urinary incontinence surgery. J Urol. 2013;189(1):204–9.
•• Finazzi-Agro E, Gammie A, Kessler TM, van Koeveringe G, Serati M, Solomon E, et al. Urodynamics useless in female stress urinary incontinence? Time for some sense-A European expert consensus. Eur Urol Focus. 2020;6(1):137–45. https://doi.org/10.1016/j.euf.2018.07.031Key review of current literature for UDS in SUI.
• Suskind AM, Cox L, Clemens JQ, Oldendorf A, Stoffel JT, Malaeb B, et al. The value of urodynamics in an academic specialty referral practice. Urology. 2017;105:48–53. https://doi.org/10.1016/j.urology.2017.02.049Retrospective study assessing patterns of UDS ordering and implications on management.
J. Christian Winters, RR Dmochowski, Howard B. Goldman, C.D. Anthony Herndon, Kathleen C. Kobashi, Stephen R. Kraus, Gary E. Lemack, Victor W. Nitti, Eric S. Rovner, Alan J. Wein. Adult Urodynamics: AUA/SUFU Guideline. American Urological Association. 2012.
Rosenzweig BA. S P, Blumenfeld D, Bhatia NN. Prevalence of abnormal urodynamic test results in continent women with severe genitourinary prolapse. Obstet Gynecol. 1992;79(4):539–42.
• Glass D, Lin FC, Khan AA, Van Kuiken M, Drain A, Siev M, et al. Impact of preoperative urodynamics on women undergoing pelvic organ prolapse surgery. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-04084-8Retrospective study that showed how UDS did not impact management of POP.
Hwang SM, de Toledo LGM, da Silva CS, Frade AB, Matos AC, Auge APF. Is urodynamics necessary to identify occult stress urinary incontinence? World J Urol. 2019;37(1):189–93. https://doi.org/10.1007/s00345-018-2366-8.
•• Asfour V, Gargasole C, Fernando R, Digesu GG, Khullar V. Urodynamics are necessary for patients with asymptomatic pelvic organ prolapse. Neurourol Urodyn. 2018;37(8):2841–6. https://doi.org/10.1002/nau.23796Retrospective study which demonstrates the high rate of LUTS among women with asymptomatic prolapse.
Sierra T, Sullivan G, Leung K, Flynn M. The negative predictive value of preoperative urodynamics for stress urinary incontinence following prolapse surgery. Int Urogynecol J. 2019;30(7):1119–24. https://doi.org/10.1007/s00192-018-03864-y.
Alas AN, Chinthakanan O, Espaillat L, Plowright L, Davila GW, Aguilar VC. De novo stress urinary incontinence after pelvic organ prolapse surgery in women without occult incontinence. Int Urogynecol J. 2017;28(4):583–90. https://doi.org/10.1007/s00192-016-3149-7.
•• Huang L, He L, Wu SL, Sun RY, Lu D. Impact of preoperative urodynamic testing for urinary incontinence and pelvic organ prolapse on clinical management in Chinese women. J Obstet Gynaecol Res. 2016;42(1):72–6. https://doi.org/10.1111/jog.12854Retrospective study which demonstrates how pre-operative UDS impacted management of POP.
Serati M, Giarenis I, Meschia M, Cardozo L. Role of urodynamics before prolapse surgery. Int Urogynecol J. 2015;26(2):165–8. https://doi.org/10.1007/s00192-014-2534-3.
Lo TS, Nagashu S, Hsieh WC, Uy-Patrimonio MC, Yi-Hao L. Predictors for detrusor overactivity following extensive vaginal pelvic reconstructive surgery. Neurourol Urodyn. 2018;37(1):192–9. https://doi.org/10.1002/nau.23273.
Abdullah B, Nomura J, Moriyama S, Huang T, Tokiwa S, Togo M. Clinical and urodynamic assessment in patients with pelvic organ prolapse before and after laparoscopic sacrocolpopexy. Int Urogynecol J. 2017;28(10):1543–9. https://doi.org/10.1007/s00192-017-3306-7.
Liedl B, Goeschen K, Sutherland SE, Roovers JP, Yassouridis A. Can surgical reconstruction of vaginal and ligamentous laxity cure overactive bladder symptoms in women with pelvic organ prolapse? BJU Int. 2019;123(3):493–510. https://doi.org/10.1111/bju.14453.
•• Panicker J, Anding R, Arlandis S, Blok B, Dorrepaal C, Harding CX, et al. Do we understand voiding dysfunction in women? Current understanding and future perspectives: ICI-RS 2017. Neurourol Urodyn. 2018;37(S4):S75–85 Review of most recent ICI understanding of voiding dysfunction and role of urodynamics.
• Malde S, Solomon E, Spilotros M, Mukhtar B, Pakzad M, Hamid R, et al. Female bladder outlet obstruction: common symptoms masking an uncommon cause. Low Urin Tract Symptoms. 2019;11(1):72–7. https://doi.org/10.1111/luts.12196Retrospective review of large videourodynamic series identifying prevalence and cause of bladder outlet obstruction in women.
Hsiao S-M, Lin H-H, Kuo H-C. Videourodynamic studies of women with voiding dysfunction. Sci Rep. 2017;7(1):6845. https://doi.org/10.1038/s41598-017-07163-2.
Meier K, Padmanabhan P. Female bladder outlet obstruction: an update on diagnosis and management. Curr Opin Urol. 2016;26(4):334–41. https://doi.org/10.1097/MOU.0000000000000303.
Dasgupta R, Critchley HD, Dolan RJ, Fowler CJ. Changes in brain activity following sacral neuromodulation for urinary retention. J Urol. 2005;174(6):2268–72. https://doi.org/10.1097/01.ju.0000181806.59363.d1.
de Groat WC, Fraser MO, Yoshiyama M, Smerin S, Tai C, Chancellor MB, et al. Neural control of the urethra. Scand J Urol Nephrol Suppl. 2001;207:35–43; discussion 106-25. https://doi.org/10.1080/003655901750174872.
Swinn MJ, Kitchen ND, Goodwin RJ, Fowler CJ. Sacral neuromodulation for women with Fowler's syndrome. Eur Urol. 2000;38(4):439–43. https://doi.org/10.1159/000020321.
Brucker BM, Fong E, Shah S, Kelly C, Rosenblum N, Nitti VW. Urodynamic differences between dysfunctional voiding and primary bladder neck obstruction in women. Urology. 2012;80(1):55–60. https://doi.org/10.1016/j.urology.2012.04.011.
Cohn JA, Brown ET, Reynolds WS, Kaufman MR, Dmochowski RR. Pharmacologic management of non-neurogenic functional obstruction in women. Expert Opin Pharmacother. 2016;12(6):657–67.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. https://doi.org/10.1002/nau.20798.
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An international urogynecological association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn. 2017;36(2):221–44. https://doi.org/10.1002/nau.23107.
Chen CH, Hsiao SM, Chang TC, Wu WY, Lin HH. Clinical and urodynamic effects of baclofen in women with functional bladder outlet obstruction: preliminary report. J Obstet Gynaecol Res. 2016;42(5):560–5. https://doi.org/10.1111/jog.12932.
•• Chapple CR, Osman NI, Birder L, Dmochowski R, Drake MJ, van Koeveringe G, et al. Terminology report from the International Continence Society (ICS) Working Group on Underactive Bladder (UAB). Neurourol Urodyn. 2018;37(8):2928–31. https://doi.org/10.1002/nau.23701Updates ICS terminology and diagnosis of underactive bladder.
Osman NI, Chapple CR, Abrams P, Dmochowski R, Haab F, Nitti V, et al. Detrusor underactivity and the underactive bladder: a new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol. 2014;65(2):389–98. https://doi.org/10.1016/j.eururo.2013.10.015.
Gammie A, Kaper M, Dorrepaal C, Kos T, Abrams P. Signs and symptoms of detrusor underactivity: an analysis of clinical presentation and urodynamic tests from a large group of patients undergoing pressure flow studies. Eur Urol. 2016;69(2):361–9. https://doi.org/10.1016/j.eururo.2015.08.014.
Jeong SJ, Lee JK, Kim KM, Kook H, Cho SY, Oh S-J. How do we diagnose detrusor underactivity? Comparison of diagnostic criteria based on an urodynamic measure. Investig Clin Urol. 2017;58(4):247–54. https://doi.org/10.4111/icu.2017.58.4.247.
Hanno PM, Erickson D, Moldwin R, Faraday MM. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53. https://doi.org/10.1016/j.juro.2015.01.086.
Shim JS, Kang SG, Park JY, Bae JH, Kang SH, Park HS, et al. Differences in urodynamic parameters between women with interstitial cystitis and/or bladder pain syndrome and severe overactive bladder. Urology. 2016;94:64–9.
• Kuo Y-C, Kuo H-C. Videourodynamic characteristics of interstitial cystitis/bladder pain syndrome-the role of bladder outlet dysfunction in the pathophysiology. Neurourol Urodyn. 2018;37(6):1971–7. https://doi.org/10.1002/nau.23542Retrospective study examining videourodynamic results in patients with diagnosis of interstitial cystitis/bladder pain syndrome; identifying the specific anatomic and functional pelvic floor disorders associated.
Cameron AP, Gajewski JB. Bladder outlet obstruction in painful bladder syndrome/interstitial cystitis. Neurourol Urodyn. 2009;28(8):944–8. https://doi.org/10.1002/nau.20729.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reconstructed Bladder Function & Dysfunction
Rights and permissions
About this article
Cite this article
Gleicher, S., Ginzburg, N. Understanding and Redefining the Role of Urodynamics in Pelvic Floor Disorders. Curr Bladder Dysfunct Rep 15, 127–134 (2020). https://doi.org/10.1007/s11884-020-00591-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-020-00591-3