Abstract
Purpose of Review
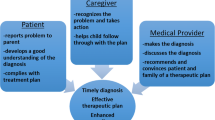
Bladder and bowel dysfunction is a common pediatric disorder that involves lower urinary tract symptoms (LUTS) as well as constipation and/or encopresis. Effective treatment of constipation in these patients leads to resolution or improvement of urinary symptoms in the majority of cases. Because many of these children initially present to the urologist with the primary complaint of LUTS, it is important for the consulting specialist to be well-versed on the topic of constipation. This review aims to provide an evidence-based guide on the evaluation and management of constipation in children.
Recent Findings
Recent papers have improved our knowledge on the utilization of interventions such as antegrade continence enemas and sacral nerve stimulation for more recalcitrant cases of constipation. Although there have been limited advancements in the use of pharmacologic therapies for the treatment of constipation in children, it is hoped that newer therapeutic agents proven effective for adult constipation will gain pediatric use over time.
Summary
Present therapy for constipation in BBD is effective for the majority of patients. There is promise for further improvement in treatment options in the near future.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Van den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006;101(10):2401–9. https://doi.org/10.1111/j.1572-0241.2006.00771.x.
Burgers R, de Jong TPVM, Visser M, Di Lorenzo C, Dijkgraaf MGW, Benninga MA. Functional defecation disorders in children with lower urinary tract symptoms. J Urol. 2013;189(5):1886–91. https://doi.org/10.1016/j.juro.2012.10.064.
McGrath KH, Caldwell PHY , Jones MP. The frequency of constipation in children with nocturnal enuresis: a comparison with parental reporting. J Paediatr Child Health 200844(1–2):19–27. https://doi.org/10.1111/j.1440-1754.2007.01207.x.
Chang S-J, Hsieh C-H, Yang SS-D. Constipation is associated with incomplete bladder emptying in healthy children. Neurourol Urodyn. 2012;31(1):105–8. https://doi.org/10.1002/nau.21225.
Kajiwara M, Kato M, Mutaguchi K, Usui T. Overactive bladder in children should be strictly differentiated from monosymptomatic nocturnal enuresis. Urol Int. 2008;80(1):57–61. https://doi.org/10.1159/000111731.
Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007;92(6):486–9. https://doi.org/10.1136/adc.2006.098335.
Franco I. Overactive bladder in children. Part 1: pathophysiology. J Urol. 2007;178(3 Pt 1):761–8; discussion 768. https://doi.org/10.1016/j.juro.2007.05.014.
Franco I. The central nervous system and its role in bowel and bladder control. Curr Urol Rep. 2011;12(2):153–7. https://doi.org/10.1007/s11934-010-0167-8.
Miyazato M, Sugaya K, Nishijima S, Ashitomi K, Ohyama C, Ogawa Y. Rectal distention inhibits bladder activity via glycinergic and GABAergic mechanisms in rats. J Urol. 2004;171(3):1353–6. https://doi.org/10.1097/01.ju.0000099840.09816.22.
Shopfner CE. Urinary tract pathology associated with constipation. Radiology. 1968;90(5):865–77. https://doi.org/10.1148/90.5.865.
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn. 2016;35(4):471–81. https://doi.org/10.1002/nau.22751.
O’Regan S, Yazbeck S. Constipation: a cause of enuresis, urinary tract infection and vesico-ureteral reflux in children. Med Hypotheses. 1985;17(4):409–13. https://doi.org/10.1016/0306-9877(85)90100-8.
Bush NC, Shah A, Barber T, Yang M, Bernstein I, Snodgrass W. Randomized, double-blind, placebo-controlled trial of polyethylene glycol (MiraLAX®) for urinary urge symptoms. J Pediatr Urol. 2013;9(5):597–604. https://doi.org/10.1016/j.jpurol.2012.10.011.
Chrzan R, Klijn AJ, Vijverberg MAW, Sikkel F, de Jong TPVM. Colonic washout enemas for persistent constipation in children with recurrent urinary tract infections based on dysfunctional voiding. Urology. 2008;71(4):607–10. https://doi.org/10.1016/j.urology.2007.11.136.
Erickson BA, Austin JC, Cooper CS, Boyt MA. Polyethylene glycol 3350 for constipation in children with dysfunctional elimination. J Urol. 2003;170(4 Pt 2):1518–20. https://doi.org/10.1097/01.ju.0000083730.70185.75.
Hodges SJ, Colaco M. Daily enema regimen is superior to traditional therapies for nonneurogenic pediatric overactive bladder. Glob Pediatr Health. 2016;3:2333794X16632941. https://doi.org/10.1177/2333794X16632941.
Loening-Baucke V. Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediatrics. 1997;100(2 Pt 1):228–32. https://doi.org/10.1542/peds.100.2.228.
Dohil R, Roberts E, Jones KV, Jenkins HR. Constipation and reversible urinary tract abnormalities. Arch Dis Child. 1994;70(1):56–7. https://doi.org/10.1136/adc.70.1.56.
Loening-Baucke V. Prevalence, symptoms and outcome of constipation in infants and toddlers. J Pediatr. 2005 Mar;146(3):359–63. https://doi.org/10.1016/j.jpeds.2004.10.046.
•• Tabbers MM, Di Lorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258–74. https://doi.org/10.1097/MPG.0000000000000266. It provides consensus recommendations on the evaluation and treatment of childhood constipation from worldwide experts.
Blethyn AJ, Verrier Jones K, Newcombe R, Roberts GM, Jenkins HR. Radiological assessment of constipation. Arch Dis Child. 1995;73(6):532–3. https://doi.org/10.1136/adc.73.6.532.
Moylan S, Armstrong J, Diaz-Saldano D, Saker M, Yerkes EB, Lindgren BW. Are abdominal x-rays a reliable way to assess for constipation? J Urol. 2010;184(4 Suppl):1692–8.
Pensabene L, Buonomo C, Fishman L, Chitkara D, Nurko S. Lack of utility of abdominal x-rays in the evaluation of children with constipation: comparison of different scoring methods. J Pediatr Gastroenterol Nutr. 2010;51(2):155–9. https://doi.org/10.1097/MPG.0b013e3181cb4309.
Benninga MA, Büller HA, Tytgat GN, Akkermans LM, Bossuyt PM, Taminiau JA. Colonic transit time in constipated children: does pediatric slow-transit constipation exist? J Pediatr Gastroenterol Nutr. 1996;23(3):241–51. https://doi.org/10.1097/00005176-199610000-00007.
Queiroz Machado V, Monteiro A, Peçanha A, Garcez da Fonseca E. Slow transit constipation and lower urinary tract dysfunction. J Pediatr Urol. 2015;11(6):357.e1–5. https://doi.org/10.1016/j.jpurol.2015.05.032.
Southwell BR, Clarke MCC, Sutcliffe J, Hutson JM. Colonic transit studies: normal values for adults and children with comparison of radiological and scintigraphic methods. Pediatr Surg Int. 2009;25(7):559–72. https://doi.org/10.1007/s00383-009-2387-x.
Tipnis NA, El-Chammas KI, Rudolph CD, Werlin SL, Sood MR. Do oro-anal transit markers predict which children would benefit from colonic manometry studies? J Pediatr Gastroenterol Nutr. 2012;54(2):258–62. https://doi.org/10.1097/MPG.0b013e31822bbcd8.
Mugie SM, Perez ME, Burgers R, Hingsbergen EA, Punati J, Mousa H, et al. Colonic manometry and colonic scintigraphy as a diagnostic tool for children with severe constipation. J Pediatr Gastroenterol Nutr. 2013;57(5):598–602. https://doi.org/10.1097/MPG.0b013e31829e0bdd.
Bijoś A, Czerwionka-Szaflarska M, Mazur A, Romañczuk W. The usefulness of ultrasound examination of the bowel as a method of assessment of functional chronic constipation in children. Pediatr Radiol. 2007;37(12):1247–52. https://doi.org/10.1007/s00247-007-0659-y.
Joensson IM, Siggaard C, Rittig S, Hagstroem S, Djurhuus JC. Transabdominal ultrasound of rectum as a diagnostic tool in childhood constipation. J Urol. 2008;179(5):1997–2002. https://doi.org/10.1016/j.juro.2008.01.055.
Klijn AJ, Asselman M, Vijverberg MAW, Dik P, de Jong TPVM. The diameter of the rectum on ultrasonography as a diagnostic tool for constipation in children with dysfunctional voiding. J Urol. 2004;172(5 Pt 1):1986–8. https://doi.org/10.1097/01.ju.0000142686.09532.46.
Singh SJ, Gibbons NJ, Vincent MV, Sithole J, Nwokoma NJ, Alagarswami KV. Use of pelvic ultrasound in the diagnosis of megarectum in children with constipation. J Pediatr Surg. 2005;40(12):1941–4. https://doi.org/10.1016/j.jpedsurg.2005.08.012.
Mason MD, Ching CB, Clayton DB, Thomas JC, Pope JC, Adams MC, et al. Diagnosis of constipation does not correlate with trans-abdominal ultrasound of rectal distention. J Pediatr Urol. 2015;11(3):146.e1–4. https://doi.org/10.1016/j.jpurol.2015.01.017.
Burgers RE, Mugie SM, Chase J, Cooper CS, von Gontard A, Rittig CS, et al. Management of functional constipation in children with lower urinary tract symptoms: report from the Standardization Committee of the International Children’s Continence Society. J Urol. 2013;190(1):29–36. https://doi.org/10.1016/j.juro.2013.01.001.
Van Ginkel R, Reitsma JB, Büller HA, van Wijk MP, Taminiau JAJM, Benninga MA. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003;125(2):357–63. https://doi.org/10.1016/S0016-5085(03)00888-6.
Gordon M, MacDonald JK, Parker CE, Akobeng AK, Thomas AG. Osmotic and stimulant laxatives for the management of childhood constipation. Cochrane Database Syst Rev. 2016;17(8):CD009118. https://doi.org/10.1002/14651858.CD009118.pub3.
Bekkali N-L-H, van den Berg M-M, Dijkgraaf MGW, van Wijk MP, Bongers MEJ, Liem O, et al. Rectal fecal impaction treatment in childhood constipation: enemas versus high doses oral PEG. Pediatrics. 2009;124(6):e1108–15. https://doi.org/10.1542/peds.2009-0022.
Koppen IJN, Broekaert IJ, Wilschanski M, Papadopoulou A, Ribes-Koninckx C, Thapar N, et al. Role of polyethylene glycol in the treatment of functional constipation in children. J Pediatr Gastroenterol Nutr. 2017;65(4):361–3. https://doi.org/10.1097/MPG.0000000000001704.
Youssef NN, Peters JM, Henderson W, Shultz-Peters S, Lockhart DK, Di Lorenzo C. Dose response of PEG 3350 for the treatment of childhood fecal impaction. J Pediatr. 2002;141(3):410–4. https://doi.org/10.1067/mpd.2002.126603.
Biebl A, Grillenberger A, Schmitt K. Enema-induced severe hyperphosphatemia in children. Eur J Pediatr. 2009;168(1):111–2. https://doi.org/10.1007/s00431-008-0705-2.
Ingebo KB, Heyman MB. Polyethylene glycol-electrolyte solution for intestinal clearance in children with refractory encopresis. A safe and effective therapeutic program. Am J Dis Child. 1988;142(3):340–2.
NASPGHAN. NASPGHAN position on Miralax use in children. 2015. https://cmcpediatrics.com/2015/01/naspghan-position-miralax-use-children/. Accessed 2 Dec 2017.
Zanetti G, Marchiori E, Gasparetto TD, Escuissato DL, Soares Souza A. Lipoid pneumonia in children following aspiration of mineral oil used in the treatment of constipation: high-resolution CT findings in 17 patients. Pediatr Radiol. 2007;37(11):1135–9. https://doi.org/10.1007/s00247-007-0603-1.
Joo JS, Ehrenpreis ED, Gonzalez L, Kaye M, Breno S, Wexner SD, et al. Alterations in colonic anatomy induced by chronic stimulant laxatives: the cathartic colon revisited. J Clin Gastroenterol. 1998;26(4):283–6. https://doi.org/10.1097/00004836-199806000-00014.
Koppen IJN, Lammers LA, Benninga MA, Tabbers MM. Management of functional constipation in children: therapy in practice. Paediatr Drugs. 2015;17(5):349–60. https://doi.org/10.1007/s40272-015-0142-4.
Morales MA, Hernández D, Bustamante S, Bachiller I, Rojas A. Is senna laxative use associated to cathartic colon, genotoxicity, or carcinogenicity? J Toxicol. 2009;2009:287247. https://doi.org/10.1155/2009/287247.
Mugie SM, Korczowski B, Bodi P, Green A, Kerstens R, Ausma J, et al. Prucalopride is no more effective than placebo for children with functional constipation. Gastroenterology. 2014;147(6):1285–1295.e1. https://doi.org/10.1053/j.gastro.2014.09.005.
Piessevaux H, Corazziari E, Rey E, Simren M, Wiechowska-Kozlowska A, Kerstens R, et al. A randomized, double-blind, placebo-controlled trial to evaluate the efficacy, safety, and tolerability of long-term treatment with prucalopride. Neurogastroenterol Motil. 2015;27(6):805–15. https://doi.org/10.1111/nmo.12553.
•• IJN K, Di Lorenzo C, Saps M, Dinning PG, Yacob D, Levitt MA, et al. Childhood constipation: finally something is moving! Expert Rev Gastroenterol Hepatol. 2016;10(1):141–55. https://doi.org/10.1586/17474124.2016.1098533. This evidence-based review discusses the most recent developments in the evaluation and treatment of constipation in childhood.
Acosta A, Camilleri M. Elobixibat and its potential role in chronic idiopathic constipation. Therap Adv Gastroenterol. 2014;7(4):167–75. https://doi.org/10.1177/1756283X14528269.
Wong BS, Camilleri M, McKinzie S, Burton D, Graffner H, Zinsmeister AR. Effects of A3309, an ileal bile acid transporter inhibitor, on colonic transit and symptoms in females with functional constipation. Am J Gastroenterol. 2011;106(12):2154–64. https://doi.org/10.1038/ajg.2011.285.
Chmielewska A, Szajewska H. Systematic review of randomised controlled trials: probiotics for functional constipation. World J Gastroenterol. 2010;16(1):69–75.
Malone PS, Ransley PG, Kiely EM. Preliminary report: the antegrade continence enema. Lancet. 1990 Nov 17;336(8725):1217–8. https://doi.org/10.1016/0140-6736(90)92834-5.
• Arya S, Gupta N, Gupta R, Aggarwal A. Constipation and outcomes of cecostomy. Am J Ther. 2016;23(6):e1867–75. https://doi.org/10.1097/MJT.0000000000000417. Provides an up-to-date summary of 12 studies investigating the efficacy of ACE therapy, concluding that it is a promising option for patients with severe, refactory constipation and fecal incontinence.
Kuizenga-Wessel S, Mousa HM, Benninga MA, Di Lorenzo C. Lack of agreement on how to use antegrade enemas in children. J Pediatr Gastroenterol Nutr. 2016;62(1):71–9. https://doi.org/10.1097/MPG.0000000000000899.
Har AF, Rescorla FJ, Croffie JM. Quality of life in pediatric patients with unremitting constipation pre and post Malone antegrade continence enema (MACE) procedure. J Pediatr Surg. 2013;48(8):1733–7. https://doi.org/10.1016/j.jpedsurg.2013.01.045.
Mousa HM, van den Berg MM, Caniano DA, Hogan M, Di Lorenzo C, Hayes J. Cecostomy in children with defecation disorders. Dig Dis Sci. 2006;51(1):154–60. https://doi.org/10.1007/s10620-006-3101-7.
Aspirot A, Fernandez S, Di Lorenzo C, Skaggs B, Mousa H. Antegrade enemas for defecation disorders: do they improve the colonic motility? J Pediatr Surg. 2009;44(8):1575–80. https://doi.org/10.1016/j.jpedsurg.2008.11.061.
Rodriguez L, Nurko S, Flores A. Factors associated with successful decrease and discontinuation of antegrade continence enemas (ACE) in children with defecation disorders: a study evaluating the effect of ACE on colon motility. Neurogastroenterol Motil. 2013;25(2):140–e81. https://doi.org/10.1111/nmo.12018.
Dolejs SC, Smith JK, Sheplock J, Croffie JM, Rescorla FJ. Contemporary short- and long-term outcomes in patients with unremitting constipation and fecal incontinence treated with an antegrade continence enema. J Pediatr Surg. 2017;52(1):79–83. https://doi.org/10.1016/j.jpedsurg.2016.10.022.
Saikaly SK, Rich MA, Swana HS. Assessment of pediatric Malone antegrade continence enema (MACE) complications: effects of variations in technique. J Pediatr Urol. 2016;12(4):246.e1–6. https://doi.org/10.1016/j.jpurol.2016.04.020.
DasGupta R, Murphy FL. Botulinum toxin in paediatric urology: a systematic literature review. Pediatr Surg Int. 2009;25(1):19–23. https://doi.org/10.1007/s00383-008-2260-3.
Dykstra DD, Sidi AA, Scott AB, Pagel JM, Goldish GD. Effects of botulinum A toxin on detrusor-sphincter dyssynergia in spinal cord injury patients. J Urol. 1988;139(5):919–22. https://doi.org/10.1016/S0022-5347(17)42717-0.
Pasricha PJ, Ravich WJ, Hendrix TR, Sostre S, Jones B, Kalloo AN. Intrasphincteric botulinum toxin for the treatment of achalasia. N Engl J Med. 1995 23;332(12):774–8. https://doi.org/10.1056/NEJM199503233321203.
Maria G, Cassetta E, Gui D, Brisinda G, Bentivoglio AR, Albanese A. A comparison of botulinum toxin and saline for the treatment of chronic anal fissure. N Engl J Med. 1998;338(4):217–20. https://doi.org/10.1056/NEJM199801223380402.
Minkes RK, Langer JC. A prospective study of botulinum toxin for internal anal sphincter hypertonicity in children with Hirschsprung’s disease. J Pediatr Surg. 2000;35(12):1733–6. https://doi.org/10.1053/jpsu.2000.19234.
Jones OM, Brading AF, Mortensen NJM. Mechanism of action of botulinum toxin on the internal anal sphincter. Br J Surg. 2004;91(2):224–8. https://doi.org/10.1002/bjs.4394.
Ahmadi J, Azary S, Ashjaei B, Paragomi P, Intrasphincteric K-SA. Botulinum toxin injection in treatment of chronic idiopathic constipation in children. Iran J Pediatr. 2013;23(5):574–8.
Irani K, Rodriguez L, Doody DP, Goldstein AM. Botulinum toxin for the treatment of chronic constipation in children with internal anal sphincter dysfunction. Pediatr Surg Int. 2008;24(7):779–83. https://doi.org/10.1007/s00383-008-2171-3.
Keshtgar AS, Ward HC, Sanei A, Clayden GS. Botulinum toxin, a new treatment modality for chronic idiopathic constipation in children: long-term follow-up of a double-blind randomized trial. J Pediatr Surg. 2007;42(4):672–80. https://doi.org/10.1016/j.jpedsurg.2006.12.045.
Keshtgar AS, Ward HC, Clayden GS. Transcutaneous needle-free injection of botulinum toxin: a novel treatment of childhood constipation and anal fissure. J Pediatr Surg. 2009;44(9):1791–8. https://doi.org/10.1016/j.jpedsurg.2009.02.056.
Tanagho EA. Neural stimulation for bladder control. Semin Neurol. 1988;8(2):170–3. https://doi.org/10.1055/s-2008-1041373.
Brazzelli M, Murray A, Fraser C. Efficacy and Safety of sacral nerve stimulation for urinary urge incontinence: a systematic review. J Urol. 2006;175(3 Pt 1):835–41. https://doi.org/10.1016/S0022-5347(05)00326-5.
Mowatt G, Glazener C, Jarrett M. Sacral nerve stimulation for fecal incontinence and constipation in adults: a short version Cochrane review. Neurourol Urodyn. 2008;27(3):155–61. https://doi.org/10.1002/nau.20565.
Thaha MA, Abukar AA, Thin NN, Ramsanahie A, Knowles CH. Sacral nerve stimulation for faecal incontinence and constipation in adults. Cochrane Database Syst Rev. 2015;24(8):CD004464. https://doi.org/10.1002/14651858.CD004464.pub3.
Kamm MA, Dudding TC, Melenhorst J, Jarrett M, Wang Z, Buntzen S, et al. Sacral nerve stimulation for intractable constipation. Gut. 2010;59(3):333–40. https://doi.org/10.1136/gut.2009.187989.
Thomas GP, Dudding TC, Rahbour G, Nicholls RJ, Vaizey CJ. Sacral nerve stimulation for constipation. Br J Surg. 2013;100(2):174–81. https://doi.org/10.1002/bjs.8944.
Janssen PTJ, Meyer YM, SMJ VK, Benninga MA, LPS S, Bouvy ND, et al. Long-term outcome of intractable constipation treated by sacral neuromodulation: a comparison between children and adults. Color Dis. 2017; https://doi.org/10.1111/codi.13837.
Van der Wilt AA, van Wunnik BPW, Sturkenboom R, Han-Geurts IJ, Melenhorst J, Benninga MA, et al. Sacral neuromodulation in children and adolescents with chronic constipation refractory to conservative treatment. Int J Color Dis. 2016;31(8):1459–66. https://doi.org/10.1007/s00384-016-2604-8.
Van Wunnik BP, Peeters B, Govaert B, Nieman FH, Benninga MA, Baeten CG. Sacral neuromodulation therapy: a promising treatment for adolescents with refractory functional constipation. Dis Colon Rectum. 2012;55(3):278–85. https://doi.org/10.1097/DCR.0b013e3182405c61.
Veiga ML, Lordêlo P, Farias T, Barroso U. Evaluation of constipation after parasacral transcutaneous electrical nerve stimulation in children with lower urinary tract dysfunction—a pilot study. J Pediatr Urol. 2013;9(5):622–6. https://doi.org/10.1016/j.jpurol.2012.06.006.
Lu PL, Asti L, Lodwick DL, Nacion KM, Deans KJ, Minneci PC, et al. Sacral nerve stimulation allows for decreased antegrade continence enema use in children with severe constipation. J Pediatr Surg. 2017;52(4):558–62. https://doi.org/10.1016/j.jpedsurg.2016.11.003.
•• Sulkowski JP, Nacion KM, Deans KJ, Minneci PC, Levitt MA, Mousa HM, et al. Sacral nerve stimulation: a promising therapy for fecal and urinary incontinence and constipation in children. J Pediatr Surg. 2015;50(10):1644–7. https://doi.org/10.1016/j.jpedsurg.2015.03.043. This study demonstrates the success of sacral nerve stimulation (SNS) in the BBD population, specificall. While most studies aim to evaluate urinary and bowel outcomes separately, this group measured the efficacy of SSN for treatment of both systems.
Dwyer ME, Vandersteen DR, Hollatz P, Reinberg YE. Sacral neuromodulation for the dysfunctional elimination syndrome: a 10-year single-center experience with 105 consecutive children. Urology. 2014;84(4):911–7. https://doi.org/10.1016/j.urology.2014.03.059.
Humphreys MR, Vandersteen DR, Slezak JM, Hollatz P, Smith CA, Smith JE, et al. Preliminary results of sacral neuromodulation in 23 children. J Urol. 2006;176(5):2227–31. https://doi.org/10.1016/j.juro.2006.07.013.
Lu PL, Koppen IJN, Orsagh-Yentis DK, Leonhart K, Ambeba EJ, Deans KJ, et al. Sacral nerve stimulation for constipation and fecal incontinence in children: long-term outcomes, patient benefit, and parent satisfaction. Neurogastroenterol Motil. 2017; https://doi.org/10.1111/nmo.13184.
Maeda Y, Lundby L, Buntzen S, Laurberg S. Suboptimal outcome following sacral nerve stimulation for faecal incontinence. Br J Surg. 2011;98(1):140–7. https://doi.org/10.1002/bjs.7302.
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterol, Rome IV Funct Disord: Disorders Gut-Brain Interaction. 2016;150:1456–1468.e2. https://doi.org/10.1053/j.gastro.2016.02.015.
Funding
This research was supported in part by the National Institutes of Health T32 training grants awarded to the Vanderbilt University Medical Center under award numbers T32GM007569 and T32DK007663.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Bernal, Dole, and Thame have no financial relationships relevant to this article to report.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Voiding Dysfunction
Rights and permissions
About this article
Cite this article
Bernal, C.J., Dole, M. & Thame, K. The Role of Bowel Management in Children with Bladder and Bowel Dysfunction. Curr Bladder Dysfunct Rep 13, 46–55 (2018). https://doi.org/10.1007/s11884-018-0458-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-018-0458-3