Abstract
Purpose of Review
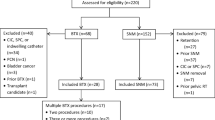
Sacral neuromodulation and intradetrusor onabotulinum toxinA are FDA approved treatment options for overactive bladder (OAB) and considered third-line therapies according to the American Urological Association (AUA) guidelines. Although each therapy has unique associated risks, infection is a common adverse event shared by both. The purpose of this review is to identify risk factors for infection in third-line therapies for OAB. A PUBMED® and MEDLINE® search was performed for scientific publications on “sacral neuromodulation,” “sacral nerve stimulation,” “onabotulinum toxinA,” “Botox,” “percutaneous tibial nerve stimulation (PTNS)” and “infection,” and “overactive bladder (OAB)” between the years 2003 and 2016. Articles were screened for reports on adverse events and were included in the review if they contained information on infection. We also limited this review to idiopathic OAB in adults.
Recent Findings
A total of 127 articles were identified (61 in the onabotulinum toxinA and 64 in the sacral neuromodulation (SNM) groups, respectively, and two containing combined data). No articles referencing PTNS and infection were identified; thus, PTNS is not reviewed in this manuscript. Twenty-nine articles met criteria and served as the source information for this article. The primary infection associated with sacral neuromodulation is device-related and ranges between 1.7 and 7.8% in patients implanted for OAB. The most common infection in the onabotulinum toxinA group is a urinary tract infection, with rates ranging from 9.5 to 44%, with the vast majority classified as uncomplicated. Potential risk factors for surgical site infection associated with SNM include patients who are immunocompromised, those with diabetes, or those with a higher BMI. Potential risk factors for urinary tract infection (UTI) associated with onabotulinum toxinA include active medication vs. placebo, urinary retention, and the use of clean intermittent catheterization.
Summary
Onabotulinum toxinA and SNM are safe and effective third-line therapies for refractory OAB. Onabotulinum toxinA injection is associated with UTIs, and risk factors appear to be the use of active drug vs. placebo, urinary retention, and use of clean intermittent catheterization. In contrast, SNM is associated primarily with surgical site infection. Risk factors identified include diabetes, higher BMI, or immunocompromised status.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327.
Gormley EA, Lightner DJ, Faraday M, Vasavada SP; American Urological Association; Society of Urodynamics, Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment.
Siegel S, Noblett K, Mangel J, Griebling TL, Sutherland SE, Bird ET, et al. Results of a prospective, randomized, multicenter study evaluating sacral neuromodulation with InterStim therapy compared to standard medical therapy at 6-months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn. 2015;34(3):224–30. doi:10.1002/nau.22544.
Visco AG, Brubaker L, Richter HE, et al. Pelvic floor disorders network. Anticholinergic therapy vs. onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med. 2012;367(19):1803–13.
• Amundsen CL, Richter HE, Menefee SA, Komesu YM, Arya LA, Gregory WT, et al. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA. 2016;316(13):1366–74. The Rosetta trial represents the first randomized clinical trial comparing intradetrusor onabotulinum toxinA to sacral neuromodulation. This trial was able to look at clinical outcomes as well as a comparison of adverse events
Spinelli M, Giardiello G, Gerber M, Arduini A, van den Hombergh U, Malaguti S. New sacral neuromodulation lead for percutaneous implantation using local anesthesia: description and first experience. J Urol. 2003;170(5):1905–7.
Clavien P, Barkun J, de Oliveira M, Dindo D. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Chapple C, Sievert KD, MacDiarmid S, Khullar V, Radziszewski P, Nardo C, et al. Onabotulinum toxinA 100 u significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomised, double-blind, placebo-controlled trial. Eur Urol. 2013;64:249–56.
•• Nitti VW, Dmochowski R, Herschorn S, Sand P, Thompson C, Nardo C, et al. Onabotulinum toxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol. 2013;189:2186–93. This study was key in obtaining FDA approval for Onabotulinum toxinA in the United States and helps elucidate the adverse events associated with this therapy.
Kuo HC, Liao CH, Chung SD. Adverse events of intravesical botulinum toxinA injections for idiopathic detrusor overactivity: risk factors and influence on treatment outcome. Eur Urol. 2010;58:919–26.
White WM, Pickens RB, Doggweiler R, Klein FA. Short-term efficacy of botulinum toxinA for refractory overactive bladder in the elderly population. J Urol. 2008;180:2522–6.
Liao CH, Kuo HC. Increased risk of large post-void residual urine and decreased long-term success rate after intravesical onabotulinumtoxinA injection for refractory idiopathic detrusor overactivity. J Urol. 2013;189:1804–10.
Wang CC, Liao CH, Kuo HC. Diabetes mellitus does not affect the efficacy and safety of intravesical onabotulinumtoxinA injection in patients with refractory detrusor overactivity. Neurourol Urodyn. 2014;33:1235–9.
Habashy D, Losco G, Tse V, Collins R, Chan L. Botulinum toxin (onabotulinumtoxinA) in the male non-neurogenic overactive bladder: clinical and quality of life outcomes. BJU Int. 2015;116(Suppl 3):61–5.
Jiang YH, Ong HL, Kuo HC. Predictive factors of adverse events after intravesical suburothelial onabotulinumtoxina injections for overactive bladder syndrome—a real-life practice of 290 cases in a single center. Neurourol Urodyn. 2015;
Tincello DG, Kenyon S, Abrams KR, et al. Botulinum toxinA versus placebo for refractory detrusor overactivity in women: a randomized blinded placebo-controlled trial of 240 women (the RELAX study). Eur Urol. 2012;62(3):507–14.
Dowson C, Watkins J, Khan MS, Dasgupta P, Sahai A. Repeated botulinum toxin type a injections for refractory overactive bladder: medium-term outcomes, safety profile, and discontinuation rates. Eur Urol. 2012;61:834–9.
Brubaker L, Richter HE, Visco A, et al. Refractory idiopathic urge urinary incontinence and botulinum a injection. J Urol. 2008;180:217–22.
Osborn DJ, Kaufman MR, Mock S, Guan MJ, Dmochowski RR, Reynolds WS. Urinary retention rates after intravesical onabotulinumtoxinA injection for idiopathic overactive bladder in clinical practice and predictors of this outcome. Neurourol Urodyn. 2015;34(7):675–8.
Sahai A, Khan MS, Dasgupta P. Efficacy of botulinum toxin-a for treating idiopathic detrusor overactivity: results from a single center, randomized, double-blind, placebo controlled trial. J Urol. 2007;177:2231.
Denys P, Le Normand L, Ghout I, et al. Efficacy and safety of low doses of onabotulinumtoxinA for the treatment of refractory idiopathic overactive bladder: a multicentre, double-blind, randomised, placebo-controlled dose-ranging study. Eur Urol. 2012;61:520–9.
Dmochowski R, Chapple C, Nitti VW, et al. Efficacy and safety of onabotulinumtoxinA for idiopathic overactive bladder: a double-blind, placebo controlled, randomized, dose ranging trial. J Urol. 2010;184:2416–22.
Flynn MK, Amundsen CL, Perevich M, et al. Outcome of a randomized, double-blind, placebo controlled trial of botulinum a toxin for refractory overactive bladder. J Urol. 2009;181:2608–15.
López Ramos H, Castellanos L, Esparza I, Jaramillo A, Rodriguez A, Bencardino C. Management of overactive bladder with onabotulinumtoxinA: systematic review and meta-analysis. Urology. 2017;100:53–8.
Altaweel W, Mokhtar A, Rabah DM. Prospective randomized trial of 100u vs 200u botox in the treatment of idiopathic overactive bladder. Urol Ann. 2011;3:66–70.
Liao CH, Wang CC, Jiang YH. Intravesical onabotulinumtoxinA injection for overactive bladder patients with frailty, medical comorbidities or prior lower urinary tract surgery. Toxins (Basel). 2016;8(4):91.
Liao CH, Chen SF, Kuo HC. Different number of intravesical onabotulinumtoxinA injections for patients with refractory detrusor overactivity do not affect treatment outcome: a prospective randomized comparative study. Neurourol Urodyn. 2016;35(6):717–23.
Guralnick ML, Benouni S, O’Connor RC, et al. Characteristics of infections in patients undergoing staged implantation for sacral nerve stimulation. Urology. 2007;69(6):1073–6.
•• Noblett K, Benson K, Kreder K. Detailed analysis of adverse events and surgical interventions in a large prospective trial of sacral neuromodulation therapy for overactive bladder patients. Neurourol Urodyn. 2016; The InSite trial is a landmark randomized trial of sacral neuromodulation vs. standard medical therapy. This article details the adverse events associated with SNM, most importantly infection rates at one year.
Kessler TM, Burkhard FC, Madersbacher H, Kofler A, Poewe W, Kiss G. Safety of prolonged sacral neuromodulation tined lead testing. Curr Med Res Opin. 2008;24(2):343–7.
Siddiqui NY, Wu JM, Amundsen CL. Efficacy and adverse events of sacral nerve stimulation for overactive bladder: a systematic review. Neurourol Urodyn. 2010;29(suppl 1):S18–23.
Daniels D, Powell C, Braasch M, Kreder K. Sacral neuromodulation in diabetic patients: success and complications in the treatment of voiding dysfunction. Neurourol Urodyn. 2010;29:578–81.
Brueseke T, Livingston B, Warda H, et al. Risk factors for surgical site infection in patients undergoing sacral nerve modulation therapy. Female Pelvic Med Reconstr Surg. 2015;21:198–204.
White WM, Mobley JD III, Doggweiler R, et al. Incidence and predictors of complications with sacral neuromodulation. Urology. 2009;73:731–5.
Amend B, Bedke J, Khalil M, Stenzl A, Sievert KD. Prolonged percutaneous SNM testing does not cause infection-related explanation. BJU Int. 2012;11:485–91.
Haraway A, Clemens JQ, He C, Stroup C, Atiemo H, Cameron A. Differences in sacral neuromodulation device infection rates based on preoperative antibiotic selection. Int Urogynecol J. 2013;24:2081–5.
Abdallah DY, Jadaan M, McCabe J. Body mass index and risk of surgical site infection following spine surgery: a meta-analysis. Eur Spine J. 2013;22(12):2800–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Noblett reports personal fees from Medtronic, grants and personal fees from Allergan, outside the submitted work
Dr. Lane has no conflicts of interests to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Reconstructed Bladder Function and Dysfunction
Rights and permissions
About this article
Cite this article
Noblett, K.L., Lane, F. Risk Factors for Infection Following Third-line Therapy for Overactive Bladder. Curr Bladder Dysfunct Rep 12, 268–272 (2017). https://doi.org/10.1007/s11884-017-0433-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-017-0433-4