Abstract
Purpose of Review
The aim of this review is to examine the prevalence of and impact of environmental exposures in the workplace and home on immigrant respiratory health in the USA.
Recent Findings
Few studies report levels of workplace and home environmental exposures for immigrant children and adults, and documenting these findings is an important first step to addressing their respiratory health concerns. Rates of respiratory disease are lowest upon first arrival and increase with duration of residency in the USA. Community Health Workers may be an efficacious intervention to reducing exposures and improving lung health among immigrant populations.
Summary
Immigrant children and adults have a high risk of occupational and home environmental exposures that can negatively affect their respiratory health. While limited studies exist, more documentation of these exposures and their impact on immigrant person’s respiratory health are needed to begin to tackle these disparities.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
United States Environmental Protection Agency. Asthma facts [May 2017]. Washington, DC: United States Environmental Protection Agency; 2017. https://www.epa.gov/sites/production/files/2017-08/documents/2017_asthma_fact_sheet.pdf. Last accessed February 25, 2018.
U.S. Census Bureau. Current population survey. January 3, 2001. Available at: https://www.census.gov/programs-surveys/cps.html. Last accessed February 25, 2018.
U.S. Census Bureau. American community survey reports: race and Hispanic origin of the foreign-born population in the United States: 2007. January 2010. Available at: http://www.census.gov/prod/2010pubs/acs-11.pdf. Last accessed February 25, 2018.
Azaroff LS, Lax MB, Levenstein C, Wegman DH. Wounding the messenger: the new economy makes occupational health indicators too good to be true. Int J Health Serv. 2004;345:271–303.
Cho CC, Oliva J, Sweitzer E, Nevarez J, Zanoni J, Sokas RK. An interfaith workers’ center approach to workplace rights: implications for workplace safety and health. J Occup Environ Med. 2007;49(3):275–81.
Dembe A. Social inequalities in occupational and health care for work-related injuries and illnesses. Int J Law Psychiatry. 1999;22:567–79.
American Federation of Labor--Congress of Industrial Organizations (AFL-CIO). Immigrant workers at risk: the urgent need for improved workplace safety and health policies and programs. Washington, DC: AFL-CIO; 2005. Available at: http://www.ncfh.org/pdfs/6000.pdf. Last accessed February 25, 2018.
McCauley LA. Immigrant workers in the United States: recent trends, vulnerable populations, and challenges for occupational health. AAOHN J. 2005;53:313–9.
Taylor AK, Murray LR. Occupational safety and health. In: Levy BS, Sidel VW, editors. Social injustice and public health. Oxford: Oxford University Press; 2006. p. 337–56.
Pransky G, Moshenberg D, Benjamin K, Portillo S, Thackrey JL, Hill-Fotouhi C. Occupational risks and injuries in non-agricultural immigrant Latino workers. Am J Ind Med. 2002;42(2):117–23.
• Cabieses B, Uphoff E, Pinart M, et al. A systematic review on the development of asthma and allergic diseases in relation to international immigration: the leading role of the environment confirmed. PLoS ONE. 2014; 9(8) e1015347: 1-16. Cabieses et al. present a systematic review demonstrating a strong correlation with environmental influences and respiratory disease in the immigrant population.
• Barr RG, Aviles-Santa L, Davis S, et al. Pulmonary disease and age at immigration among Hispanics: results from the Hispanic community health study/study of Latinos. Am J Respir Crit Care Med. 2016;193(4):386–95. The SOL study represents a large Latino cohort study of adults from multiple Latin countries of origin living across the USA
Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012;(94):1–8.
Stoecklin-Marois MT, Bigham CW, Bennett D, Tancredi DJ, Schenker MB. Occupational exposures and migration factors associated with respiratory health in California Latino farm workers: the MICASA study. J Occup Environ Med. 2015;57(2):152–8.
Corlin L, Woodin M, Thanikachalam M, Lowe L, Brugge D Evidence for the healthy immigrant effect in older Chinese immigrants: a cross-sectional study. BMC Public Health. June 2014: 14: 603: 1-8.
Huang B, Appel HB, Nicdao EG, Lee HJD, Ai AL. Chronic conditions, behavioral health, and use of health services among Asian American men: the first nationally representative sample. J Men's Health. 2013;7(1):66–76.
Chang M, Kelvin EA. Differing asthma prevalence by gross national index of country of birth among New York City residents. Allergy. 2014;69(4):494–500.
Kearney GD, Chatterjee AB, Talton J, Chen H, Quandt SA, Summers P, et al. The association of respiratory symptoms and indoor housing conditions among migrant farmworkers in eastern North Carolina. J Agromedicine. 2014;19(4):395–405.
• White H, Khan K, Lau C, et al. Identifying health and safety concerns in southeast Asian immigrant nail salon workers. Arch Environ Occup Health. 2015;70(4):196–203. This article highlights serious concerns in nail salon workers and an overall need for improving education and protective measures in this population.
Johnson M, Nriagu J, Hammad A. Asthma, environmental risk factors, and hypertension among Arab Americans in metro Detroit. J Immigr Minor Health. 2010;12(5):640–51.
Kim YA, Collins TW, Grineski SE. Neighborhood context and the Hispanic health paradox: differential effects of immigrant density on children’s wheezing by poverty, nativity and medical history. Health Place. May 2014: 27:1-8.
• Balcazar AJ, Grineski SE, Collins TW. The Hispanic health paradox across generations: the relationship of child generational status and citizenship with health outcomes. Public Health. 2015;129(6):691–7. A large survey sampling a Texan border town with Mexico that shows a clear generational effect where each generation in the USA carries an increased risk of respiratory disease.
Litt JS, Goss C, Diao L, Allshouse A, Diaz-Castillo S, Bardwell RA, et al. Housing environments and child health conditions among recent Mexican immigrant families: a population-based study. J Immigr Minor Health. 2010;12(5):617–25.
Koinis-Mitchell D, Sato AF, Kopel SJ, McQuaid EL, Seifer R, Klein R, et al. Immigration and acculturation-related factors and asthma morbidity in Latino children. J Pediatr Psychol. 2011;36(10):1130–43.
•• Burchard EG, Avila PC, Nazario S, et al. Genetics of Asthma in Latino Americans (GALA) Study: lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. Am J Respir Crit Care Med. 2004;169:386–92. This study includes a sample of Mexican and Puerto Ricans living in Mexico, Puerto Rico, and the mainland USA seeking to understand differences in asthma trends and medication responsiveness in the distinct populations whose GALA study additionally sought to understand the potential role of genetic variations.
•• Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. The authors presented a study highlighting the severe asthma seen in Puerto Rican children compared to other Latino groups.
Singh GK, Yu SM, Kogan MD. Health, chronic conditions, and behavioral risk disparities among U.S. immigrant children and adolescents. Public Health Rep. 2013;128(6):463–79.
Postma JM, Smalley K, Ybarra V, Kieckhefer G. The feasibility and acceptability of a home-visitation, asthma education program in a rural, Latino/a population. J Asthma. 2011;48(2):139–46.
Martin MA, Mosnaim GS, Rojas D. Evaluation of an asthma medication training program for immigrant Mexican community health workers. Prog Community Health Partnersh. 2011;5(1):95–103.
Pawankar R, Canonica GW, ST Holgate ST, Lockey RF, Blaiss M. The WAO white book on allergy (Update 2013).
Pawankar R. Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J. 2014;7:12.
Parker EA, Israel BA, Robins TG, Mentz G, Xihong Lin, Brakefield-Caldwell W, et al. Evaluation of community action against asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35:376–95.
• Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95:652–9. This study offers support of future community health worker interventions as this randomized control trial showed improvements in asthma symptoms, health care utilization, and caregiver quality of life.
Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediatr Adolesc Med. 2009;163:141–9.
Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of community health worker interventions. Evidence report/technology assessment no. 181 (prepared by the RTI inter-national-University of North Carolina Evidence-based Practice Center under contract no. 290 2007 10056 I). AHRQ publication no. 09-E014. Rockville: Agency for Healthcare Research and Quality; 2009.
APHA Section definition. Available: http://www.apha.org/membergroups/primary/aphaspigwebsites/chw/. Last accessed February 25, 2018.
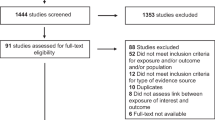
Moher D, Liberati A, Altman DG, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Acknowledgements
Thank you to Victoria Steigerwald for her assistance with formatting this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This review is in compliant with ethical standards.
Conflict of Interest
Giselle Mosnaim receives research grant support from GlaxoSmithKline and Propeller Health, owns stock options in Electrocore, and serves as a consultant and/or member of a scientific advisory board for Electrocore, GlaxoSmithKline, Teva, Novartis, Astra Zeneca, Boehringer Ingelheim, and Propeller Health. Andrea Pappalardo served on the Speaker’s Bureau for Boehringer Ingelheim in 2017.
Human and Animal Rights Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Occupational Allergies
Rights and permissions
About this article
Cite this article
Pappalardo, A.A., Mosnaim, G. Immigrant Respiratory Health: a Diverse Perspective in Environmental Influences on Respiratory Health. Curr Allergy Asthma Rep 18, 21 (2018). https://doi.org/10.1007/s11882-018-0779-5
Published:
DOI: https://doi.org/10.1007/s11882-018-0779-5