Abstract
Background/aims
Limited data exists on the outcomes of COVID-19 patients presenting with altered mental status (AMS). Hence, we studied the characteristics and outcomes of hospitalized COVID-19 patients who presented with AMS at our hospital in rural southwest Georgia.
Methods
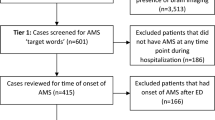
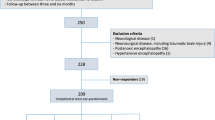
Data from electronic medical records of all hospitalized COVID-19 patients from March 2, 2020, to June 17, 2020, were analyzed. Patients were divided in 2 groups, those presenting with and without AMS. Primary outcome of interest was in-hospital mortality. Secondary outcomes were needed for mechanical ventilation, need for intensive care unit (ICU) care, need for dialysis, and length of stay. All analyses were performed using SAS 9.4 and R 3.6.0.
Results
Out of 710 patients, 73 (10.3%) presented with AMS. Majority of the population was African American (83.4%). Patients with AMS were older and more likely to have hypertension, chronic kidney disease (CKD), cerebrovascular disease, and dementia. Patients with AMS were less likely to present with typical COVID-19 symptoms, including dyspnea, cough, fever, and gastrointestinal symptoms. Predictors of AMS included age ≥ 70 years, CKD, cerebrovascular disease, and dementia. After multivariable adjustment, patients with AMS had higher rates of in-hospital mortality (30.1% vs 14.8%, odds ratio (OR) 2.139, p = 0.019), ICU admission (43.8% vs 40.2%, OR 2.59, p < 0.001), and need for mechanical ventilation (27.4% vs 18.5%, OR 2.06, p = 0.023). Patients presenting with AMS had increased length of stay.
Conclusions
Patients with COVID-19 presenting with AMS are less likely to have typical COVID-19 symptoms, and AMS is an independent predictor of in-hospital mortality, need for ICU admission, and need for mechanical ventilation.
Similar content being viewed by others
Introduction
As of October 31, 2020, the novel coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, accounted for more than 1,197,126 deaths (46,189,124 cases) globally, and more than 230,566 deaths (9,127,708 cases) in the United States (US) [1]. The main clinical manifestations of COVID-19 include fever, chills, cough, and dyspnea. Additional complaints include altered mental status, headache, anosmia, and dysgeusia. In some cases, nervous system involvement including encephalitis, polyneuropathy, and stroke have been reported [2].
Many viruses can alter the structure and function of the central and peripheral nervous system. These alterations may include encephalitis, toxic encephalopathy, and acute demyelinating lesions [2]. Certain viruses have been described as “neurotropic,” which means they have the potential to invade nervous tissues and infect macrophages, microglia, or astrocytes in the central nervous system [2]. Some potential mechanisms of CNS invasion include blood–brain barrier damage, cytokine-induced impairment of neurons, and neuronal transmission of the virus through axonal transport [3].
Common predictors of mortality in COVID-19 patients include age ≥ 65 years, morbid obesity, hypertension, and immunosuppression [4]. Patients with diabetes have been reported in some instances to have a twofold increase in mortality [5]. A study of critically ill older patients with COVID-19 found that 86% of patients had comorbidities including chronic kidney disease, congestive heart failure, COPD, and diabetes, which further increases their risk of mortality from the virus [6]. A recent small study reported worse outcomes in patients that presented with neurological symptoms, including AMS, headache, lethargy, seizure, and syncope [3]. However, they did not look at AMS separately and its independent effect on the outcomes of COVID-19 patients.
Scarce data exists on the outcomes of COVID-19 patients that present with AMS. The primary objective of our study was to determine if AMS is an independent predictor of mortality in COVID-19 patients. Secondary objectives were to determine if AMS was an independent predictor of need for ICU admission, need for mechanical ventilation, need for new dialysis, and increased length of stay in the hospital in COVID-19 patients.
Materials and methods
We performed a retrospective study of COVID-19 patients admitted to Phoebe Putney Health System, which serves over 40 counties and a population of approximately 825,000 in rural Southwest Georgia. The Augusta University institutional review board approved the study and waived the requirement for informed consent due to minimal risk. Patients were admitted to one of the three Phoebe Putney hospitals between March 2, 2020, and June 17, 2020, inclusive of those dates. All hospitalized patients ≥ 18 years of age with confirmed COVID-19 were included in this study.
Data were collected from the electronic medical records (Meditech and AthenaHealth). All patients were confirmed positive for COVID-19 by nasopharyngeal swab using a polymerase chain reaction (PCR) test. Patients were considered to have confirmed infection if the initial test result was positive or if a repeat test was positive. Repeat tests were performed on inpatients during hospitalization shortly after initial test results were available if there was a high clinical pretest probability of COVID-19 or if the initial negative test result had been judged likely to be a false-negative due to poor sampling technique. Transfers from one in-system hospital to another were merged and considered as a single visit.
We collected data on demographics, insurance, baseline comorbidities, tobacco use, alcohol use, illicit drug use, home medications, symptoms on presentation, vitals, laboratory tests, electrocardiogram, presenting disease severity, need for intensive care unit (ICU) admission, need for mechanical ventilation, new requirement for dialysis, length of stay (LOS), discharge status, and mortality. Severe COVID-19 on presentation was defined as patients presenting with either severe pneumonia, septic shock, or acute respiratory distress syndrome (ARDS). Comorbidities included hypertension (HTN), diabetes mellitus (DM), coronary artery disease (CAD), congestive heart failure (CHF), chronic kidney disease (CKD), cerebrovascular accident (CVA, or transient ischemic attack (TIA)), dementia, and immunosuppression. All comorbidities except immunosuppression were adjudicated based on the 10th version of the International Classification of Diseases (ICD-10). Patients were considered immunosuppressed if they had been on chronic steroids or other immunosuppressive therapy. To calculate the LOS, the difference between actual admission and discharge/death times were used.
Patients were divided into two groups, those with and without AMS on presentation. In this study, patients were included in the AMS group if their admitting physician included AMS as one of the chief complaints in their initial hospital visit. While AMS can include a variety of symptoms (including confusion, disorientation, unusual behavior, new-onset memory loss, for example), the determination was left to the admitting physician’s discretion. Continuous variables were reported as median and interquartile range (IQR), whereas categorical variables were reported as numbers and percentages. For bivariate analyses, continuous variables were analyzed using the Mann–Whitney–Wilcoxon nonparametric test, categorical variables were analyzed using Pearson chi-square test, and Bonferroni adjusted p values are reported. We used AIC (Akaike information criteria)-based stepwise multiple logistic regression of AMS onto the demographic and history variables to determine independent predictors of AMS. To assess the effect of AMS on mortality and other secondary clinical outcomes, we used similar AIC-based stepwise multiple logistic and linear regression of each outcome on the aforementioned demographics, comorbidities, presenting signs and symptoms, and AMS. We report all results of our analysis that have p-values less than 0.05. All statistical analysis was performed using the Statistical Analysis Software (SAS) version 9.4 (Cary, NC, USA) and R version 3.6.0.
All authors reviewed the manuscript and took responsibility for accuracy and completeness of the data presented.
Results
Out of 710 patients hospitalized for COVID-19 during the study period, 73 (10.3%) presented with AMS as one of their chief complaints. The majority of the population were African American (83.4%). Baseline characteristics of the two groups (with and without AMS) are presented in Table 1. Patients presenting with AMS were older than patients without AMS (median age 74 years vs. 62 years; p < 0.001) and patients with AMS were more likely to be ≥ 70 years old (63.0% in AMS vs. 30.6% in non-AMS, p < 0.001). There was no significant difference in ethnicity or BMI ranges (non-obese, obese, morbidly obese) between the two groups. Hypertension was more common in the AMS group (93.2% vs. 77.1%; p = 0.016). Chronic kidney disease was more common in the AMS group (35.6% vs. 14.3%; p < 0.001), as was diabetes (58.9% vs. 41.3%; p = 0.044). Additionally, a history of CVA or TIA was more common in the AMS group (36.1% vs. 10.8%; p < 0.001). Also, prevalence of dementia was higher in the AMS group (33.3% vs. 5.9%; p < 0.001). Congestive heart failure and COPD were also not different between the two groups.
Patients presenting with severe disease on admission did not differ between the two groups. Patients with AMS were less likely to present with shortness of breath than the patients who did not have AMS (16.4% vs. 59.3%, p < 0.001). Patients with AMS were also less likely to present with cough (17.8% vs. 42.9%, p < 0.001), fever (28.8% vs. 45.2%, p = 0.007), and abdominal symptoms, including nausea, vomiting, diarrhea, and abdominal pain (6.8% vs. 21.2%, p = 0.004) (Table 2).
The AIC-based stepwise logistic regression analysis showed that patients with age ≥ 70 years (OR 2.570; CI 1.4–4.7, p = 0.002), CKD (OR 2.515; CI 1.3–4.7, p = 0.004), history of CVA/TIA (OR 3.063; CI 1.6–5.7, p < 0.001), and history of dementia (OR 6.536; CI 3.2–12.18, p < 0.001) were more likely to present with AMS (Table 3).
The association of AMS, demographics, and comorbidities with the in-hospital outcomes (in-hospital mortality, need for ICU admission, need for mechanical ventilation, need for new dialysis, and length of hospital stay) in COVID-19 patients was assessed. Altered mental status was a significant predictor of in-hospital mortality (30.1% in AMS vs. 14.8% in non-AMS; OR 2.139; CI 1.1–3.9, p = 0.019). Altered mental status was also a significant predictor of need for ICU admission (43.8% in AMS vs. 40.2% in non-AMS; OR 2.593; CI 1.5–4.4, p < 0.001) and mechanical ventilation (27.4% in AMS vs. 18.5% in non-AMS; OR 2.060; CI 1.1–3.8, p = 0.023). The need for new dialysis was numerically higher in the AMS group but not statistically significant (19.2% in AMS vs. 8.3% in non-AMS; OR 2.047, CI 0.9–4.3, p = 0.065). Additionally, those with AMS were more likely to be discharged to another facility (vs. being discharged home) compared to those without AMS (51.0% in AMS vs. 19.9% in non-AMS; OR 2.749, CI 1.53–5.1, p < 0.001) (Table 4). Patients in the AMS group also had an increased length of stay in the hospital; however, this difference was significant only in survivors. Those in the AMS group that survived their hospitalization stayed approximately 4.67 days longer (standard error 1.584, p = 0.003).
Predictors of in-hospital mortality, other than AMS, included age ≥ 70 years (OR 2.343, CI 1.5–3.7, p < 0.001), immunosuppression (OR 5.998, CI 2.5–14.2, p < 0.001), severe disease on presentation (OR 6.690, CI 4.0–11.6, p < 0.001), male gender (OR 1.824, CI 1.2–2.9, p = 0.010), CKD (OR 2.203, CI 1.2–4.1, p = 0.015), and diabetes (OR 1.791, CI 1.3–2.8, p = 0.013). Severe COVID-19 on presentation was also an independent predictor of ICU admission, (OR 3.203, CI 2.2–4.7, p < 0.001). Other independent predictors of mechanical ventilation included severe disease on presentation (OR 5.427, CI 3.4–8.9, p < 0.001), morbid obesity (OR 2.056, CI 1.2–3.6, p = 0.010), and diabetes (OR 1.553, CI 1.0–2.3, p = 0.035). Additional predictors of new dialysis included history of CVA/TIA (OR 2.402, CI 1.2–4.6, p = 0.009), and male gender (OR 1.872, CI 1.1–3.3, p = 0.024). Predictors of discharge to any facility (other than home), included age ≥ 70 years (OR 2.062, CI 1.4–3.0, p < 0.001), male gender (OR 1.868, CI 1.3–2.7, p < 0.001), severe COVID-19 on presentation (OR 3.179, CI 2.2–4.6, p < 0.001), and dementia (OR 2.286, CI 1.2–4.3, p = 0.011). Patients of African American race were twice as likely to be discharged home (OR 0.534, CI 0.3–0.9, p = 0.008). Additional predictors of longer length of stay among survivors included severe COVID-19 on presentation (estimate = 5.6, SE = 0.89, p < 0.001) and history of CAD (estimate = 3.455, SE = 1.6, p = 0.031).
Discussion
This is the first study to show that AMS on presentation is an independent predictor of mortality in hospitalized COVID-19 patients. Results of our study indicate that AMS is also an independent predictor of need for ICU care, mechanical ventilation, increased LOS, and discharge to a facility other than home. A study by Mao et al. initially made the link between neurological symptoms and the severity of illness in COVID-19 patients [7]. Their findings showed that patients with severe disease (determined by respiratory status) were more likely to have neurological manifestations, including CNS manifestations (dizziness, headache, impaired consciousness, acute cerebrovascular disease, ataxia, seizure), peripheral nervous system manifestations (taste, smell, vision impairments), and skeletal muscle injury manifestations. While this study included neurological parameters that we did not evaluate, the connection they made between COVID-19 and neurological symptoms was important and encouraged further research to be done.
Another study has been published that looked at neurological complaints in patients hospitalized with COVID-19 infection in Louisiana [3]. We highlight some of the important differences between that study compared to our study. First, the sample size was much smaller than ours (n = 710 vs n = 250) and there were only 34 patients in their “neurological chief complaint” category. Their “neurological chief complaint” category included AMS, headache, lethargy, seizure, and syncope, whereas our study specifically focuses on AMS as the primary chief complaint of interest. Altered mental status was the most common neurological symptom and was a significant predictor of prolonged hospital stay, death, and intubation in that study. Also, their study did include patients who had a neurological complaint during hospitalization, whereas our study specifically looked at AMS at the time of initial presentation.
Our results illustrate the importance of AMS as a presenting symptom in COVID-19 patients. Regardless of patient comorbidities, AMS increases the risk of mortality by twofold. We found that the patients presenting with AMS are less likely to have other typical symptoms of COVID-19, like cough, dyspnea, fever, and GI symptoms. Primary care and emergency department physicians should keep this in mind and test patients that present with AMS for COVID-19 even if they do not present with the typical symptoms of COVID-19. Predictors of AMS included age ≥ 70 years, history of CKD, history of CVA/TIA, and history of dementia; patients with these comorbidities should be carefully assessed for changes in mental status if COVID-19 infection is suspected. Also, if patients with AMS are ≥ 70 years, morbidly obese, immunosuppressed, or have CKD, they are more likely to have worse outcomes. Patients presenting with AMS are twice as likely to die during their hospital stay, require transfer to the ICU, or require mechanical ventilation. Additionally, patients with AMS that survived hospitalization were much more likely to be discharged to a facility other than home. Patients with AMS were also more likely to require a longer hospital stay (up to 4.6 days longer on average). Therefore, if patients are COVID-19 positive and have AMS, they should be admitted to the hospital for thorough evaluation and treatment since their outcomes are much worse.
In the AMS group, 30 patients had only head computed tomography (CT) scans done, 7 patients had only brain magnetic resonance imaging (MRI) scans done, and 12 patients had both CT scans and MRI scans done during their hospitalization. None of the CT scans showed any acute abnormalities. Five of the MRI scans showed areas of restricted diffusion, representing likely infarcts. One MRI showed a variety of restricted foci within the deep cerebral white matter, suggesting hypotensive infarction or an embolic shower, along with bilateral symmetric foci involving the thalami and temporal poles. Another MRI showed subcentimeter areas of acute infarction within the cortex and subcortical white matter of the left parietal, left occipital, and bilateral posterior temporal lobes. One MRI showed acute ischemic infarction involving the right optic radiation. Another MRI showed foci of acute infarctions at the left parieto-occipital lobe junction and at the left parietal lobe gyrus. Another MRI showed small, acute ischemic infarcts within the right midbrain and right medulla. Out of the 5 abnormal MRIs, 3 likely contributed to the AMS. Acute infarction in the right optic radiation and midbrain should not cause AMS.
In the AMS group, 24 patients had some form of psychiatric illness documented, including depression (present in over half of this group), anxiety, bipolar disorder, panic disorder, adjustment disorder, and previous suicide attempts. Although mental health and psychiatric illnesses in this patient population could be a confounding factor in a patient presenting with AMS, we believe the AMS was more related to the acute viral infection.
Several limitations to our study should be noted. First, AMS is an extremely broad, nonspecific term that can be interpreted in a variety of ways. We used the data available to us, which primarily included an emergency department healthcare provider’s documentation of a patient’s presenting symptom. Therefore, some patients in the AMS group may be false positives, and some false negatives could have been inadvertently left out of the study. Additionally, our study population is that of a small, rural town in southwest Georgia and is predominantly African American; our results may be difficult to generalize to a larger, more diverse population. Also, the study only included patients that were admitted to the hospital, therefore we are unaware of how AMS may be a symptom in COVID-19 patients who were treated on an outpatient basis and had more mild disease. Also, the large number of independent tests performed, coupled with the model selection process, could potentially lead to spurious significance. Hence, the results of our study should not be interpreted as confirmatory but rather hypothesis generating. Finally, this was a retrospective study with data abstraction from the electronic medical record, and hence some data elements might not be accurately captured.
Conclusion
This study shows that among patients hospitalized with COVID-19 infection, AMS as a presenting symptom is an independent predictor of in-hospital mortality, need for ICU admission, need for mechanical ventilation, discharge to other facilities, and length of stay. Patients presenting with AMS are also less likely to have typical COVID-19 symptoms; hence, it is important to keep a high index of suspicion while evaluating and triaging these patients. Further studies are needed to confirm the findings of our study.
References
Johns Hopkins University. Coronavirus Resource Center. Available at https://coronavirus.jhu.edu/map.html. Accessed 31 October 2020
Wu Y, Xu X, Chen Z et al (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 87:18–22
Chachkhiani D, Soliman MY, Barua D et al (2020) Neurological complications in a predominantly African American sample of COVID-19 predict worse outcomes during hospitalization [published online ahead of print, 2020 Aug 25]. Clin Neurol Neurosurg 197:106173
Shah P, Owens J, Franklin J et al (2020) Demographics, comorbidities and outcomes in hospitalized Covid-19 patients in rural southwest Georgia. Ann Med 52(7):354–360. https://doi.org/10.1080/07853890.2020.1791356 (Epub 2020 Jul 13 PMID: 32620056)
Kumar A, Arora A, Sharma P et al (2020) Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr. 14(4):535–545. https://doi.org/10.1016/j.dsx.2020.04.044 (Epub 2020 May 6 PMID: 32408118; PMCID: PMC7200339)
Shahid Z, Kalayanamitra R, McClafferty B et al (2020) COVID-19 and older adults: what we know. J Am Geriatr Soc 68(5):926–929. https://doi.org/10.1111/jgs.16472
Mao L, Jin H, Wang M et al (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol 77(6):683–690
Acknowledgements
The authors would like to thank Jennifer Hill, Krista Barfield, and James Franklin for their help in data abstraction.
Author information
Authors and Affiliations
Contributions
All authors had access to the data and a role in manuscript creation.
Corresponding author
Rights and permissions
About this article
Cite this article
Kenerly, M.J., Shah, P., Patel, H. et al. Altered mental status is an independent predictor of mortality in hospitalized COVID-19 patients. Ir J Med Sci 191, 21–26 (2022). https://doi.org/10.1007/s11845-021-02515-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02515-4