Abstract
Objective
To assess whether instillation of lidocaine gel both before and after flexible cystoscopy is more effective at reducing post procedural symptoms than instillation of lidocaine gel pre flexible cystoscopy alone. We hypothesise that inadequate urethral dwell time and dilution of lidocaine gel by the irrigation fluid during flexible cystoscopy limits its anaesthetic efficacy. Only one other study has attempted to reduce bothersome urinary symptoms through an intervention after flexible cystoscopy.
Methods
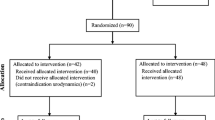
This was a randomised controlled trial in which patients were randomised 1:1 to receive lidocaine gel pre and post flexible cystoscopy (treatment) or lidocaine gel pre flexible cystoscopy only (control). Patient-reported outcome measures were used to assess symptoms and quality of life prior to cystoscopy, on day 2 and day 7 post cystoscopy.
Result
Fifty patients were divided equally between the treatment and control groups. There were no significant differences in baseline characteristics between the groups (p = 1.000). An overall symptoms variable was measured, though no significant difference was found in the distribution of responses between the groups at baseline, 2 or 7 days after the flexible cystoscopy (p = 0.423, 0.651,0.735). In the treatment group, 1 patient (4.0%) presented to a doctor for review following flexible cystoscopy, and 4 patients (16.0%) presented in the control group (p = 0.349).
Conclusion
Initial study results suggest that post-operative lidocaine does not significantly limit the exacerbation of urinary symptoms following flexible cystoscopy; however, our results are not powered to detect a small difference. We do not recommend a change in practice based on our results.
Similar content being viewed by others
Introduction
Flexible cystoscopy is one of the most important diagnostic tools available to the urologist. The technique of using a flexible fibre optic camera to visualise bladder mucosa was first described by Harry Wilbur in 1981, using a pre-existing choledochoscope [1]. The first dedicated flexible cystoscope was presented by Clare Fowler in Dublin, at the 1984 BAUS Annual Scientific Meeting at the Royal College of Surgeons in Ireland [1]. Since then, flexible cystoscopy has become the gold-standard first-line investigation in detecting bladder cancer and is one of the most commonly performed urological procedures [2]. Flexible cystoscopy is usually performed in the ambulatory setting using topical local anaesthetic lubricating gel and takes only a matter of minutes to perform. It represents a cheaper, faster, more readily available alternative to rigid cystoscopy and eliminates the need for admission to hospital and a general anaesthetic.
Despite the well-described advantages of flexible cystoscopy, it has some limitations also, with patients often experiencing troublesome post-procedural sequelae. Common symptoms after flexible cystoscopy include dysuria, urgency and frequency of urination, haematuria and suprapubic pain [3]. A recent survey highlighted the reduction of pain associated with flexible cystoscopy as a research priority for patients [4].
The use of primitive urethral lubricants such as olive oil has been reported for centuries, and the addition of local anaesthetic agents to improve tolerability of flexible cystoscopy has been debated for well over 100 years. Cocaine was the first product used for urethral anaesthesia in 1884 [5]. Since then, silicone, tetracaine, dyclonine, tripelennamine and most recently lidocaine have been used for this purpose [6]. There remains no consensus still on optimum agent, dwell time, quantity and instillation rate, and the product used various widely between different institutions [7].
Lidocaine gel is commonly administered as a lubricant prior to flexible cystoscopy due to its well-recognised anaesthetic and antiseptic properties. Despite its widespread acceptance and use amongst the urological community, numerous trials have failed to show that lidocaine gel is significantly better at reducing the symptoms experienced following cystoscopy than other lubricants which do not contain anaesthetic [8,9,10,11,12,13]. Indeed, three meta-analyses identified in a search of the literature on the topic have yielded conflicting results as to the benefit of using lidocaine gel for flexible cystoscopy [8, 9, 14]. The era of evidence-based medicine has seen a migration away from simply doing things because they have been done previously towards performing interventions that are proven to be of benefit for patients.
Although lidocaine gel has a low side effect profile and is generally well tolerated, should we be routinely using it for urethral anaesthesia without good evidence to support its use? Should we be searching for novel methods to improve tolerability of flexible cystoscopy? Or, should we look to use this well-known anaesthetic in a more effective way?
We hypothesise that inadequate urethral dwell time and dilution of lidocaine gel by the irrigation fluid during flexible cystoscopy limits its anaesthetic efficacy, and that it may be more beneficial to administer the gel after the person has emptied their bladder following the procedure. The aim of this study is to investigate whether administration of lidocaine gel both before and after flexible cystoscopy can reduce post procedure symptoms.
Methods
This was a prospective randomised controlled trial. Ethical approval was obtained from the Tallaght University Hospital/St James Hospital Joint Research and Ethics Committee (2019-01 List 3 (02)). All patients undergoing flexible cystoscopy in Tallaght University Hospital between September and December 2019 were considered for enrolment in the study. Exclusion criteria included the presence of microbiological evidence of urinary tract infection on urinalysis, intellectual disability and the presence of an indwelling urethral catheter.
Patients were given a patient information leaflet explaining the purpose of the study and an information booklet explaining the procedure to read in the waiting room. Patients who agreed to take part in the trial were then counselled and consented by the doctor performing the procedure, and a written consent form was included in the patient’s chart.
Patients were randomised into 2 groups using a simple computerised randomisation tool. The treatment arm received intra-urethral lidocaine gel pre and post flexible cystoscopy. The control arm received intra-urethral lidocaine gel pre flexible cystoscopy only. The control arm represents current accepted practice in our institution. The lubricating gel used in all subjects was a pre-loaded syringe (11 ml men, 6 ml women) containing 2% lidocaine and 0.05% chlorhexidine. The external genitalia were sterilised using a chlorhexidine-based solution, and warm saline was used for irrigation. A 15.5-fr flexible cystoscope was used in all procedures. Flexible cystoscopies in the trial were performed by 5 urology trainees and 1 consultant urologist. All operators had significant experience in performing flexible cystoscopy before the trial commenced.
All patients had pre-procedural 2% lidocaine gel inserted urethrally in the same fashion: slow steady push with milking of the gel down the male urethra. Urethral dwell time prior to commencement of cystoscopy was 30 s, with pinching of the urethral meatus to retain the gel. Following the procedure, both study arms were instructed to empty their bladder. The treatment arm were instructed to return to the examination table following bladder emptying where they had 2% lidocaine gel inserted again in the same fashion as before the procedure. Patients were given wound pads to prevent soiling of undergarments after leaving the cystoscopy suite.
All participants completed validated symptom and quality of life questionnaires prior to cystoscopy, on day 2 and day 7 post cystoscopy (Fig. 1). The 14-point UTISA questionnaire assessed 7 of the most common symptoms experienced by patients following flexible cystoscopy in terms of severity and bothersomeness. Symptoms assessed were frequency of urination, urinary urgency, dysuria, haematuria, suprapubic discomfort, low back pain and incomplete bladder emptying. Each symptom was evaluated using a Likert-type response scale. The severity response options were ‘did not have’, ‘mild’, ‘moderate’ and ‘severe’ (scored 0-3), and the bothersome response options were ‘not at all’, ‘a little’, ‘moderately’ and ‘a lot’(scored 0–3) [15].
A data collection sheet was completed by the performing urologist following cystoscopy, noting patient demographics, study arm, findings at cystoscopy, first cystoscopy or repeat procedure and whether and intervention was performed, e.g. removal of ureteric stent.
Results
The total sample size in this study was 50, with 25 participants in the treatment arm and 25 participants in the control arm. Because of the small sample size in each arm, a Kolmogorov-Smirnov test was performed to assess the normality of the variables. For normal variables, an independent-samples t test was performed to investigate any differences in the mean of the variables between the two trial arms, while for non-normal variables, the non-parametric Mann-Whitney test was performed. To investigate the association between categorical variables with only two levels, the Fisher’s exact test was used.
The significance level of the tests was initially set to 5%; however, as multiple tests have been performed for some variables, a Bonferroni correction was used to avoid the multiple comparison problem, by diving the significance level by the total number of tests, hence using a new threshold. Analysis was done in SPSS V.25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).
The mean (sd) age of the participants in the treatment and control groups was 61.96 (12.93) and 61.96 years (17.81), respectively. The indications for flexible cystoscopy are shown in Table 1, along with the number of first time or repeat procedures.
An independent-samples t test revealed no significance difference between the mean age of the two groups, with a p value = 1.000. In the treatment group, out of 25 participants, 8 (32.0%) were females, while this was 6 (24.0%) in the control group; however, the Fisher’s exact test showed no significant difference in the distribution of gender between the two groups, with a p value = 0.754 (Table 1).
In the treatment group, 1 patient (4.0%) presented to a doctor for review following flexible cystoscopy compared with 4 patients (16.0%) in the control group. However, the difference was not significant according to the Fisher’s exact test with a p value of 0.349. In addition, the same proportion of participants in each group were prescribed antibiotics, with no significant difference between the proportions (p = 0.349) (Table 1).
Symptom questionnaire
A symptom questionnaire was given to participants in the two groups at baseline, and also 2 and 7 days after the flexible cystoscopy. The severity and bothersomeness of 7 symptoms were measured, namely, frequency, urgency, dysuria, incomplete bladder emptying, supra-pubic tenderness, low back pain and haematuria, using a series of questions each with 4 categories, coded as below (severity/bothersomeness):
-
0: Did not have the symptom/Not at all
-
1: Mild/A little
-
2: Moderate/Moderately
-
3: Severe/A lot
A series of Mann-Whitney’s tests were performed to assess any differences in the distribution of the responses at each time point (baseline, 2 days and 7 days after the flexible cystoscopy) between the two groups. As a result, 3 tests were carried out for each symptom. Therefore, a new threshold was calculated using a Bonferroni correction, by dividing the initial significance level of 5% (0.05) by 3, yielding a threshold of 0.017; hence, any p value < 0.017 was considered significant. However, no significant difference was found between the treatment group and control group as the p values were mostly quite large. The results for symptoms severity are shown on Table 2, and for symptoms bothersome on Table 3.
An overall symptoms variable was also measured, though no significant difference was found in the distribution of responses between the groups at baseline, 2 or 7 days after the flexible cystoscopy with p values of 0.423, 0.651 and 0.735 respectively.
Discussion
Numerous novel techniques to reduce urinary symptoms following flexible cystoscopy have been attempted, including trans-cutaneous electrical nerve stimulation, pre-cystoscopy patient education videos, viewing the procedure in real time, listening to music during the process, increasing the hydrostatic pressure of irrigation fluid, inhalation of nitrous oxide and most recently urination during cystoscopy to relax the external sphincter. However, the use of topical local anaesthetic lubricating gel has been the mainstay and most widely accepted method used to try and reduce adverse symptoms associated with flexible cystoscopy [16,17,18,19,20,21,22,23].
Flexible cystoscopy remains an uncomfortable procedure to undergo for patients [3, 24]. Most studies to date have focused on reducing pain experienced during flexible cystoscopy; however, our primary objective was to reduce the post-procedural symptoms experienced by patients. Dysuria is experienced by approximately 50% of patients, with a significant number also reporting urgency, frequency, suprapubic discomfort, and visible haematuria following flexible cystoscopy [3]. Approximately 6.6% of patients present to their GP as a result of bothersome symptoms and most are treated empirically for a urinary tract infection despite a true infection rate of only 2.7% [3]. This has significant implications for anti-microbial resistance and adverse drug reactions, whilst also increasing the economic cost associated with flexible cystoscopy.
Conceptually giving topical local anaesthetic to a mucosal surface should provide suitable analgesia as evidenced by the effectiveness of local anaesthetic sprays and lozenges in the oral cavity. However, consistent benefit has not been achieved with urethral application of local anaesthetic to date. We hypothesised that this observed phenomenon may be a result of incorrect timing of administration of topical anaesthetic to the urethra and that giving local anaesthetic following the procedure may allow more time for absorption and produce better results.
A search of the literature revealed only one other paper that attempted to reduce post-procedural symptoms through an intervention following cystoscopy. Wong et al. examined whether an oral bicarbonate-based solution (Ural®) administered for 2 days following flexible cystoscopy could reduce dysuria by alkalinising the urine. However, their study did not show a statistically significant reduction in post-operative symptoms [25].
Our trial demonstrated that instillation of lidocaine gel following flexible cystoscopy does not lead to a significant reduction in post-operative symptoms. Changes in the severity and bothersomeness of symptoms flowing flexible cystoscopy between the treatment and control groups were not statistically significant. Those in the treatment arm of our study were less likely to seek medical assistance for persistent bothersome lower urinary tract symptoms 1 week following cystoscopy; however, this was not statistically significant.
The major limitation of our study is sample size. We aimed for a sample size of 200 patients which would be powered to detect a small effect. Unfortunately, efforts to recruit subjects were hampered by the curtailment of elective flexible cystoscopy at our institution due to the COVID-19 pandemic, and the trial was concluded prematurely. By including patients who had undergone flexible cystoscopy before, there is potential for bias reporting by comparing with their previous experiences.
Possible explanations for why lidocaine instilled following the flexible cystoscopy did not reduce post procedural symptoms include the following:
Gel properties
As mentioned, our lubricating gel contained 2% lidocaine and 0.05% chlorhexidine. A study by Jayathillake et al. suggests that chlorhexidine directly contributes to urinary urgency and dysuria flowing cystoscopy. Chlorhexidine precipitates in salt-based solutions such as saline which is commonly used for irrigation during flexible cystoscopy. Furthermore, intact mucosal membranes may be penetrated by chlorhexidine directly causing irritation [26, 27]. Alarmingly, there has been reports of anaphylactic shock following intra-urethral instillation of gel containing chlorhexidine [28]. Without strong evidence supporting its role in prevention of urinary tract infection post flexible cystoscopy and the potential for directly causing urinary symptoms and possibly life threatening adverse drug events, does this represent safe practice?
Leakage
We did not use penile clamps in our study to ensure lidocaine gel was retained within the urethra due to implications for patient convenience and time constraints of cystoscopy lists. There is potential that the gel leaked out of the urethra before it could be absorbed.
Origin of painful symptoms
Two studies have shown that the most painful part of flexible cystoscopy is when the cystoscope initially passes through the contracted external sphincter in the membranous urethra [12, 29]. This is potentially due to the abundance of afferent nerves in this area. Song et al. identified that the dorsal nerve of the penis and the terminal branch of the pudendal nerve innervate the membranous urethra in 53.3% of male cadavers [30]. Thus, a potentially more effective intervention would be to alter the site local anaesthetic is given perhaps in the form of a dorsal penile block.
Conclusion
Our initial study results suggest that post-operative lidocaine gel does not limit the exacerbation of urinary symptoms following flexible cystoscopy; however, our preliminary results are not powered to detect a small effect. Further assessment with a larger sample size is warranted to determine conclusively whether no benefit is gained from instillation of urethral local anaesthetic following flexible cystoscopy. However, currently, we do not recommend change of practise based on our results.
References
Surgeons) BBAoU. Available from: https://www.baus.org.uk/_userfiles/pages/files/Museum/24%20-%20Flexis.pdf.
Babjuk M, Burger M, Compérat EM et al (2019) European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ) - 2019 update. Eur Urol. 76(5):639–657
Burke DM, Shackley DC, O'Reilly PH (2002) The community-based morbidity of flexible cystoscopy. BJU Int. 89(4):347–349
Smith AB, Chisolm S, Deal A et al (2018) Patient-centered prioritization of bladder cancer research. Cancer. 124(15):3136–3144
Muhammad A, Malik MM (2020) Minimal invasive surgery under surface anesthesia (intraurethral) an historical review. J Univ Med Dent Coll 1
Tzortzis V, Gravas S, Melekos MM, de la Rosette JJ (2009) Intraurethral lubricants: a critical literature review and recommendations. J Endourol. 23(5):821–826
McFarlane N, Denstedt J, Ganapathy S, Razvi H (2001) Randomized trial of 10 mL and 20 mL of 2% intraurethral lidocaine gel and placebo in men undergoing flexible cystoscopy. J Endourol 15(5):541–544
Patel AR, Jones JS, Babineau D (2008) Lidocaine 2% gel versus plain lubricating gel for pain reduction during flexible cystoscopy: a meta-analysis of prospective, randomized, controlled trials. J Urol. 179(3):986–990
Aaronson DS, Walsh TJ, Smith JF et al (2009) Meta-analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU International. 104(4):506–510
Akkoç A, Kartalmış M, Aydın C et al (2016) 2% Lidocaine gel or plain lubricating gel: which one should be used in male flexible cystoscopy? Turk J Urol. 42(2):92–96
Birch BRP, Ratan P, Morley R et al (1994) Flexible cystoscopy in men: is topical anaesthesia with lignocaine gel worthwhile? Br J Urol 73(2):155–159
Chen YT, Hsiao PJ, Wong WY et al (2005) Randomized double-blind comparison of lidocaine gel and plain lubricating gel in relieving pain during flexible cystoscopy. J Endourol. 19(2):163–166
Choong S, Whitfield HN, Mecanathan V et al (1997) A prospective, randomized, double-blind study comparing lignocaine gel and plain lubricating gel in relieving pain during flexible cystoscopy. Br J Urol 80(1):69–71
Raskolnikov D, Brown B, Holt SK et al (2019) Reduction of pain during flexible cystoscopy: a systematic review and meta-analysis. J Urol. 202(6):1136–1142
Clayson D, Wild D, Doll H et al (2005) Validation of a patient-administered questionnaire to measure the severity and bothersomeness of lower urinary tract symptoms in uncomplicated urinary tract infection (UTI): the UTI Symptom Assessment questionnaire. BJU Int 96(3):350–359
Hruby G, Ames C, Chen C et al (2006) Assessment of efficacy of transcutaneous electrical nerve stimulation for pain management during office-based flexible cystoscopy. Urology. 67(5):914–917
Gunendran T, Briggs RH, Wemyss-Holden GD, Neilson D (2008) Does increasing hydrostatic pressure ("bag squeeze") during flexible cystoscopy improve patient comfort: a randomized, controlled study. Urology. 72(2):255–258 discussion 8-9
Raheem OA, Mirheydar HS, Lee HJ et al (2015) Does Listening to music during office-based flexible cystoscopy decrease anxiety in patients: a prospective randomized trial. J Endourol. 29(7):791–796
Zhang ZS, Wang XL, Xu CL et al (2014) Music reduces panic: an initial study of listening to preferred music improves male patient discomfort and anxiety during flexible cystoscopy. J Endourol. 28(6):739–744
Patel AR, Jones JS, Angie S, Babineau D (2007) Office based flexible cystoscopy may be less painful for men allowed to view the procedure. J Urol. 177(5):1843–1845
Zhang ZS, Tang L, Wang XL et al (2011) Seeing is believing: a randomized controlled study from China of real-time visualization of flexible cystoscopy to improve male patient comfort. J Endourol. 25(8):1343–1346
Xie Y, Wang W, Yan W, Liu D, Liu Y (2020) Efficacy of urination in alleviating man's urethral pain associated with flexible cystoscopy: a single-center randomized trial. BMC Urol 20(1)
Berajoui MB, Aditya I, Herrera-Caceres J et al (2020) A prospective randomized controlled trial of irrigation "bag squeeze" to manage pain for patients undergoing flexible cystoscopy. J Urol. 204(5):1012–1018
Herr HW, Schneider M (2001) Outpatient flexible cystoscopy in men: a randomized study of patient tolerance. J Urol. 165(6 Pt 1):1971–1972
Wong LM, Huang JG, Yong TL et al (2011) Does sodium bicarbonate reduce painful voiding after flexible cystoscopy? A prospective, randomized, double-blind, controlled trial. BJU Int. 108(5):718–721
Jayathillake A, Mason DFC, Broome K, Tan G (2006) Chlorhexidine in urethral gel: does it cause pain at flexible cystoscopy? Urology. 67(4):670–673
Winrow MJ (1973) Metabolic studies with radiolabelled chlorhexidine in animals and man. J Periodontal Res Suppl. 12:45–48
Wicki J, Deluze C, Cirafici L, Desmeules J (1999) Anaphylactic shock induced by intraurethral use of chlorhexidine. Allergy. 54(7):768–769
Taghizadeh AK, El Madani A, Gard PR et al (2006) When does it hurt? Pain during flexible cystoscopy in men. Urol Int. 76(4):301–303
Song LJ, Lu HK, Wang JP, Xu YM (2010) Cadaveric study of nerves supplying the membranous urethra. Neurourol Urodyn. 29(4):592–595
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethics approval
Obtained by SJH/TUH Research Ethics Committee Secretariat (2019-01 List 3 (02)
Consent for publication
All authors consent to publication
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keane, K.G., Redmond, E.J., McIntyre, C. et al. Does instillation of lidocaine gel following flexible cystoscopy decrease the severity of post procedure symptoms? A randomised controlled trial assessing the efficacy of lidocaine gel post flexible cystoscopy. Ir J Med Sci 190, 1553–1559 (2021). https://doi.org/10.1007/s11845-020-02458-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02458-2