Abstract
Purpose
To examine the prevalence of comorbidities and the association of these comorbidities with demographics, tumor characteristics, treatments received, overall survival, and causes of death in a population-based cohort of colorectal cancer (CRC) patients.
Methods
Adult patients with stage I–III CRC diagnosed between 2004 and 2015 were included. Comorbidities were captured using Charlson comorbidity index. Causes of death were categorized using International Classification of Diseases, tenth revision codes. Patients were categorized into five mutually exclusive comorbid groups (cardiovascular disease alone, diabetes alone, cardiovascular disease plus diabetes, other comorbidities, or no comorbidities). Data were analyzed using descriptive statistics, Kaplan-Meier survival analyses, and Cox proportional hazards models.
Results
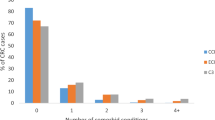
There were 12,265 patients. Mean follow-up was 3.8 years. Approximately one third of patients had a least one comorbidity, with cardiovascular disease and diabetes being most common. There were statistically significant differences across comorbid groups on treatments received and overall survival. Those with comorbidity had lower odds of treatment and greater risk of death than those with no comorbidity. Those with cardiovascular disease plus diabetes fared the worst for prognosis (median overall survival 3.3 [2.8–3.7] years; adjusted HR for death, 2.27, 95% CI 2.0–2.6, p < .001). Cardiovascular disease was the most common cause of non-CRC death.
Conclusions
CRC patients with comorbidity received curative intent treatment less frequently and experienced worse outcomes than patients with no comorbidity. Cardiovascular disease was the most common cause of non-cancer death.
Implications for Cancer Survivors
Management of comorbidities, including healthy lifestyle coaching, at diagnosis and into survivorship is an important component of cancer care.

Similar content being viewed by others
References
Canadian Cancer Society/Statistics Canada. Canadian Cancer Statistics 2016. 2016.www.cancer.ca. Accessed 21 Mar 2018.
Sarfati D, Koczwara B, Jackson C. The impact of comorbidity on cancer and its treatment. CA Cancer J Clin. 2016;66(4):338–50. https://doi.org/10.3322/caac.21342.
Sogaard M, Thomsen R, Bossen K, Sorensen HT, Horgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013;5:3–29.
Canadian Institute for Health Information. Seniors and the health care system: what is the impact of multiple chronic conditions. 2011 www.cihi.ca. Accessed 4 Feb 2018.
Ostenfeld EB, Norgaard M, Thomsen RW, Iversen LH, Jacobsen JB, Sogaard M. Comorbidity and survival of Danish patients with colon and rectal cancer from 2000–2011: a population-based cohort study. Clin Epidemiol. 2013;5(Suppl I):65–74. https://doi.org/10.2147/CLEP.S47154.
Statistics Canada. Table 102–0561. Leading causes of death, total population, by age group and sex, Canada. www5.statcan.gc.ca/cansim/a47. Accessed 29 Mar 2018.
Sarfati D, Tan L, Blakely T, Pearce N. Comorbidity among patients with colon cancer in New Zealand. N Z Med J. 2011;142:76–88.
Zafar SY, Abernethy AP, Abbott DH, Grambow SC, Marcello JE, Herndon JE, et al. Comorbidity, age, race and stage at diagnosis in colorectal cancer: a retrospective parallel analysis of two health systems. BMC Cancer. 2008;8:345.
Iversen LH, Norgaard M, Jacobsen J, Laruberg S, Sorensen HT. The impact of comorbidity on survival of Danish colorectal cancer patients from 1995-2006—a population-based cohort study. Dis Colon Rectum. 2009;52(1):71–8. https://doi.org/10.1007/DCR.0b013e3181974384.
Hahn EE, Gould MK, Munoz-Plaza CE, Lee JS, Parry C, Shen E. Understanding comorbidity profiles and their effect on treatment and survival in patients with colorectal cancer. J Natl Compr Cancer Netw. 2018;16(1):23–34. https://doi.org/10.6004/jnccn.2017.7026.
Erichsen R, Horvath-Puho E, Iversen LH, et al. Does comorbidity interact with colorectal cancer to increase mortality? A nationwide population-based cohort study. Br J Cancer. 2013;109:2005–13. https://doi.org/10.1038/bjc.2013.541.
Dasgupta P, Youlden DR, Baade PD. An analysis of competing mortality risks among colorectal cancer survivors in Queensland, 1996-2009. Cancer Causes Control. 2013;24:897–909. https://doi.org/10.1007/s10552-013-0166-4.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening of the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–0. https://doi.org/10.1016/j.jclinepi.2001.22.008.
Statistics Canada. Ethnocultural portrait of Canada highlight tables, 2016 census. http://www12.statcan.ca/english/census16/data/highlights/ethnic/index.cfm?Lang. Accessed 31 Mar 2011.
Statistics Canada. Table 206–0021. Income statistics by economic family type and income source, Canada, provinces and selected census metropolitan areas (CMAs). www5.statcan.gc.ca/cansim/a47. Accessed 17 Feb 2018.
Collaborative Stage Data Collection System. About collaborative stage. Retrieved from www.cancerstaging.org/cstage/about/Pages. Accessed 4 Feb 2018.
Preen DB, Holman CDJ, Spilsbury K, Semmens JB, Brameld KJ. Length of comorbidity lookback period affect regression model performance of administrative health data. J Clin Epidemiol. 2006;59:940–6. https://doi.org/10.1016/j.jclinepi.2005.12.013.
Deyo R, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Alberta Health Services. Early stage colon cancer treatment. 2017. www.albertahealthservices.ca/cancerguidelines. Accessed 17 Mar 2018.
BC Cancer Agency. BC Cancer Agency drug manual: fluorouracil. 2015. www.bccanceragency.bc.ca/drug-database-site. Accessed 4 Feb 2018.
BC Cancer Agency. BC Cancer Agency drug manual: oxaliplatin. 2015. Retrieved from www.bccanceragency.bc.ca/drug-database-site. Accessed 4 Feb 2018.
WHO. Classification of Disease: ICD-10 online version. 2016. Accessed 10 Oct 2017.
Kleinbaum DG, Klein M. Survival analysis: a self learning text. Statistics for biology and health. 3rd ed. New York: Springer; 2013.
Public Health Agency of Canada. How healthy are Canadian? A trend analysis of the health of Canadians from a healthy living and chronic disease perspective. 2016. https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html. Accessed 10 Mar 2018.
Cho H, Mariotto AB, Mann BS, Klabunde CN, Feuer EJ. Assessing non-cancer related health status of US cancer patients: other-cause survival and comorbidity prevalence. Am J Epidemiol. 2013;178(3):339–49. https://doi.org/10.1093/aje/kws580.
Sarfati D, Gurney J, Lim BT, et al. Identifying important comorbidity among cancer populations using administrative data: prevalence and impact on survival. Asia Pac J Clin Oncol. 2013;12(1) https://doi.org/10.1111/ajco.12130. published online ahead of print December 19, 2013.
Hahn EE, Gould MK, Munoz-Plaza CE, Lee JS, Parry C, Shen E. Understanding comorbidity profiles and their effect on treatment and survival in patients with colorectal cancer. J Natl Compr Cancer Netw. 2018;16(1):23–34. https://doi.org/10.6004/jccn.2017.7026.
Janssen-Heijnen MLG, Houterman S, Lemmens VEPP, Louwman MWJ, Maas HAAM, Coebergh JWW. Prognostic impact of increasing age and comorbidity in cancer patients: a population-based approach. Crit Rev Oncol Hematol. 2005;55:231–40. https://doi.org/10.1016/j.critrevonc.2005.04.008.
Rodrigues G, Sanatani M. Age and comorbidity considerations related to radiotherapy and chemotherapy administration. Semin Radiat Oncol. 2012;22:227–83. https://doi.org/10.1016/jsemradonc.2012.05.004.
Cronin DP, Harlan LC, Potosky AL, Clegg LX, Stevens JL, Mooney MM. Patterns of care for adjuvant therapy in a random population-based sample of patients diagnosed with colorectal cancer. Am J Gastroenterol. 2006;101:2308–18. https://doi.org/10.1111/j.1572-0241.2006.00775.x.
Sarfati D, Hill S, Blakely T, Robson B, Purdie G, Dennett E, et al. The effect of comorbidity on the use of adjuvant chemotherapy and survival from colon cancer: a retrospective cohort study. BMC Cancer. 2009;9:110. https://doi.org/10.1186/1471-2407-9-116.
Gross CP, McAvay GJ, Guo Z, Tinetti ME. The impact of chronic illnesses on the use and effectiveness of adjuvant chemotherapy for colon cancer. Cancer. 2007;109(12):2410–9. https://doi.org/10.1002/cncr.22726.
Keating NL, Landrum MB, Klabunde CN, Fletcher RH, Rogers SO, Doucette WR, et al. Adjuvant chemotherapy for stage III colon cancer: do physicians agree about the importance of patient age and comorbidity. J Clin Oncol. 2008;26(15):2532–7. https://doi.org/10.1200/JCO.2007.15.9434.
Shayeb ME, Scarfe W, Yasui Y, Winget M. Reasons physicians do not recommend and patients refuse adjuvant chemotherapy for stage III colon cancer: a populations-based chart review. BMC Res Notes. 2012;5:269. https://doi.org/10.1186/1756-0500-5-2569.
Kutner JS, Vu KO, Prindiville SA, Byers TE. Patient age and cancer treatment decisions: patient and physician views. Cancer Pract. 2000;8(3):114–9.
Etzioni DA, El-Khoueiry AB, Beart RW. Rates and predictors of chemotherapy use of stage III colon cancer: a systematic review. Cancer. 2008;113(12):3289. https://doi.org/10.1002/cncr.23958.
Lemmens VEPP, Janssen-Heijnen MLG, Verheij CDGW, Houterman S, van Driel OJR, Coebergh JWW. Comorbidity leads to altered treatment and worse survival of elderly patients with colorectal cancer. Br J Surg. 2005;92:615–23. https://doi.org/10.1002/bjs.4913.
Sjodahl R, Rosell J, Starkhammar H. Causes of death after surgery for colon cancer—impact of other diseases, urgent admittance, and gender. Scand J Gastroenterol. 2013;48(10):1160–5. https://doi.org/10.3109/00365521.2013.828771.
van Erning RN, van Steenbergen LN, Lemmens VEPP, et al. Conditional survival for long-term colorectal cancer survivors in the Netherlands: who do best? Eur J Cancer. 2014;50:1731–9. https://doi.org/10.1016/j.ejca.2014.04.009.
Zaorsky NG, Churilla TM, Egleston BL, Fisher SG, Ridge JA, Horwitz EM, et al. Causes of death among cancer patients. Ann Oncol. 2017;28:400–7. https://doi.org/10.1093/annonc/mdw604.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133(11):1104–14. https://doi.org/10.1161/CIRCULATIONAHA.115.020406.
Weaver KE, Foraker RE, Alfano CM, Rowland JH, Arora NK, Bellizzi KM, et al. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecological cancers: a gap in survivor care? J Cancer Surviv. 2013;7:253–61. https://doi.org/10.1007/s11764-013-0267-9.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2013;173(6):676–82. https://doi.org/10.1093/aje/kwq433.
Extermann M. Measuring comorbidity in older cancer patients. Eur J Cancer. 2000;36:453–71.
Institute of Medicine and National Research Council. From cancer patient to cancer survivor: lost in transition. 2006. http://nap.edu/11468. Accessed 21 May 2018.
Funding
Dr. Cuthbert has postdoctoral salary support through the University of Calgary, Cumming School of Medicine Arnie Charbonneau Cancer Institute and O’Brien Institute for Public Health and the Canadian Institutes of Health Research. No additional funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Colleen Cuthbert: conceptualization, formal analysis, and writing, reviewing, and editing. Brenda Hemmelgarn: conceptualization, formal analysis, and writing, reviewing, and editing. Yuan Xu: data abstraction, reviewing, and editing. Winson Cheung: conceptualization, formal analysis, and writing, reviewing, and editing.
Corresponding author
Ethics declarations
This study received approval from the Health Research Ethics Board of Alberta (HREBA.CC-17-0034-REN1). Study findings are reported according to Strengthening of the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human subjects
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Cuthbert, C.A., Hemmelgarn, B.R., Xu, Y. et al. The effect of comorbidities on outcomes in colorectal cancer survivors: a population-based cohort study. J Cancer Surviv 12, 733–743 (2018). https://doi.org/10.1007/s11764-018-0710-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-018-0710-z