Abstract
Purpose
The purpose of this study was to determine the evolution of neurocognitive problems from therapy completion to long-term follow-up in survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only.
Methods
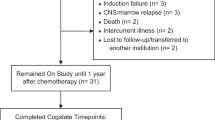
We evaluated whether attention problems observed at therapy completion evolve into long-term executive dysfunction in 158 survivors treated on a single institution protocol. Treatment data (high-dose intravenous methotrexate exposure [serum concentration] and triple intrathecal chemotherapy injections) were collected. Parent report of behavior and direct cognitive testing of survivors was conducted at end of therapy, and survivors completed neurocognitive testing when > 5 years post-diagnosis.
Results
At the end of chemotherapy, survivors (52% female; mean age 9.2 years) demonstrated higher frequency of impairment in sustained attention (38%) and parent-reported inattention (20%) compared to population expectations (10%). At long-term follow-up, survivors (mean age 13.7 years; 7.6 years post-diagnosis) demonstrated higher impairment in executive function (flexibility 24%, fluency 21%), sustained attention (15%), and processing speed (15%). Sustained attention improved from end of therapy to long-term follow-up (p < 0.001). Higher methotrexate AUC and greater number of intrathecal injections were associated with attention problems (p = 0.009, p = 0.002, respectively) at the end of chemotherapy and executive function (p < 0.001, p = 0.02, respectively) problems at long-term follow-up. Attention problems at the end of therapy were not associated with executive function problems at long-term follow-up (p’s > 0.05). The direct effect of chemotherapy exposure predicted outcomes at both time points.
Conclusions and Implications for Cancer Survivors
Survivors should be monitored for neurocognitive problems well into long-term survivorship, regardless of whether they show attention problems at the end of therapy. Treatment exposures are the best predictor of long-term complications.



Similar content being viewed by others
References
Iyer NS, Balsamo LM, Bracken MB, Kadan-Lottick NS. Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood. 2015;126(3):346–53. https://doi.org/10.1182/blood-2015-02-627414.
Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med. 2009;360(26):2730–41. https://doi.org/10.1056/NEJMoa0900386.
Cheung YT, Krull KR. Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci Biobehav Rev. 2015;53:108–20. https://doi.org/10.1016/j.neubiorev.2015.03.016.
Krull KR, Brinkman TM, Li C, Armstrong GT, Ness KK, Srivastava DK, et al. Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude lifetime cohort study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013;31(35):4407–15. https://doi.org/10.1200/jco.2012.48.2315.
Krull KR, Hockenberry MJ, Miketova P, Carey M, Moore IM. Chemotherapy-related changes in central nervous system phospholipids and neurocognitive function in childhood acute lymphoblastic leukemia. Leukemia & lymphoma. 2013;54(3):535–40. https://doi.org/10.3109/10428194.2012.717080.
Conklin HM, Krull KR, Reddick WE, Pei D, Cheng C, Pui CH. Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst. 2012;104(18):1386–95. https://doi.org/10.1093/jnci/djs344.
Jacola LM, Krull KR, Pui CH, Pei D, Cheng C, Reddick WE, et al. Longitudinal assessment of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia treated on a contemporary chemotherapy protocol. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(11):1239–47. https://doi.org/10.1200/jco.2015.64.3205.
Krull KR, Cheung YT, Liu W, Fellah S, Reddick WE, Brinkman TM, et al. Chemotherapy pharmacodynamics and neuroimaging and neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(22):2644–53. https://doi.org/10.1200/jco.2015.65.4574.
Kanellopoulos A, Andersson S, Zeller B, Tamnes CK, Fjell AM, Walhovd KB, et al. Neurocognitive outcome in very long-term survivors of childhood acute lymphoblastic leukemia after treatment with chemotherapy only. Pediatr Blood Cancer. 2016;63(1):133–8. https://doi.org/10.1002/pbc.25690.
Anderson P. Assessment and development of executive function (EF) during childhood. Child neuropsychology : a journal on normal and abnormal development in childhood and adolescence. 2002;8(2):71–82. https://doi.org/10.1076/chin.8.2.71.8724.
Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135–68. https://doi.org/10.1146/annurev-psych-113011-143750.
Romine CB, Reynolds CR. A model of the development of frontal lobe functioning: findings from a meta-analysis. Appl Neuropsychol. 2005;12(4):190–201. https://doi.org/10.1207/s15324826an1204_2.
Bhojwani D, Sabin ND, Pei D, Yang JJ, Khan RB, Panetta JC, et al. Methotrexate-induced neurotoxicity and leukoencephalopathy in childhood acute lymphoblastic leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(9):949–59. https://doi.org/10.1200/jco.2013.53.0808.
Conners CKS, M. Conners’ continuous performance test II (CPT II V. 5). North Tonawanda, NY: Multi-Health Systems Inc; 2000.
Conners C. Conners rating scales-revised: technical manual. New York: Multi-Health Systems. (Inc); 1997.
Delis DC, Kaplan, E. & Kramer, J.H. . Delis-Kaplan executive function system. San Antonio, TX: Psychological Corporation; 2001.
Wechsler D. Wechsler intelligence scale for children—fourth edition. San Antonio, TX: Harcourt Assessment, Inc; 2003.
Wechsler D. Wechsler adult intelligence scale—fourth edition. Pearson: San Antonio; 2008.
Meyers JE. MKR. Rey complex figure test and recognition trial: professional manual. Psychological Assessment Resources: Odessa, FL; 1995.
Lafayette Instrument Grooved Pegboard Test User Instructions. Lafayett IN: Lafatette Instrument@; 2002.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57(1):289–300.
Best JR, Miller PH. A developmental perspective on executive function. Child Dev. 2010;81(6):1641–60. https://doi.org/10.1111/j.1467-8624.2010.01499.x.
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121(1):65–94.
Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. Journal of the International Neuropsychological Society : JINS. 2007;13(2):298–311. https://doi.org/10.1017/s1355617707070324.
Klenberg L, Korkman M, Lahti-Nuuttila P. Differential development of attention and executive functions in 3- to 12-year-old Finnish children. Dev Neuropsychol. 2001;20(1):407–28. https://doi.org/10.1207/s15326942dn2001_6.
Duncan J, Owen AM. Common regions of the human frontal lobe recruited by diverse cognitive demands. Trends Neurosci. 2000;23(10):475–83.
Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. Journal of child psychology and psychiatry, and allied disciplines. 2006;47(3–4):296–312. https://doi.org/10.1111/j.1469-7610.2006.01611.x.
Reddick WE, Taghipour DJ, Glass JO, Ashford J, Xiong X, Wu S, et al. Prognostic factors that increase the risk for reduced white matter volumes and deficits in attention and learning for survivors of childhood cancers. Pediatr Blood Cancer. 2014;61(6):1074–9. https://doi.org/10.1002/pbc.24947.
Noble KG, Houston SM, Brito NH, Bartsch H, Kan E, Kuperman JM, et al. Family income, parental education and brain structure in children and adolescents. Nat Neurosci. 2015;18(5):773–8. https://doi.org/10.1038/nn.3983.
Acknowledgements
We thank Dr. Mary Relling, PharmD, St. Jude Children’s Research Hospital, and her lab that provide pharmacokinetic data, and Pia Banerjee, PhD, Joycelynn Butler, MS, William Lewis, MS, Adrienne Studaway, Med, Adrienne Studaway, Med, Cynthia Jones, MA, and Deborah Stewart, MA, all from Cognitive Neuroscience group, St. Jude Children’s Research Hospital, for providing technical support.
Funding
This study was funded by NIMH (R01-MH085849 to KR Krull), NCI (U01-CA195547 to MM Hudson/LL Robison), and American Lebanese Syrian Associated Charities.
Author information
Authors and Affiliations
Contributions
The following authors have made substantial contributions to the intellectual content of the paper, including conception/design (WL, YTC, DS, KRK), acquisition, analysis, or interpretation of data (WL, YTC, HMC, LMJ, DS, VGN, HZ, JGG, IH, LLR, CHP, MMH, KRK), drafting of the manuscript (WL, YTC, KRK), and critical revision of the manuscript for important intellectual content (WL, YTC, HMC, LMJ, DS, VGN, HZ, JGG, IH, LLR, CHP, MMH, KRK). Contributions also include statistical analysis (WL, DS) and obtaining funding (KRK, LLR, MMH). All authors have approved the final version of this manuscript. KRK had full access to all data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest including financial interests, activities, relationships, and affiliations and sources of funding and support.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
ESM 1
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Liu, W., Cheung, Y.T., Conklin, H.M. et al. Evolution of neurocognitive function in long-term survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only. J Cancer Surviv 12, 398–406 (2018). https://doi.org/10.1007/s11764-018-0679-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-018-0679-7