Abstract
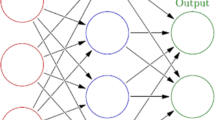
Emergency departments are characterized by the need for quick diagnosis under pressure. To select the most appropriate treatment, a series of rules to support decision-making has been offered by scientific societies. The effectiveness of these rules affects the appropriateness of treatment and the hospitalization of patients. Analyzing a sample of 1844 patients and focusing on the decision to hospitalize a patient after a syncope event to prevent severe short-term outcomes, this work proposes a new algorithm based on neural networks. Artificial neural networks are a non-parametric technique with the well-known ability to generalize behaviors, and they can thus predict severe short-term outcomes with pre-selected levels of sensitivity and specificity. This innovative technique can outperform the traditional models, since it does not require a specific functional form, i.e., the data are not supposed to be distributed following a specific design. Based on our results, the innovative model can predict hospitalization with a sensitivity of 100% and a specificity of 79%, significantly increasing the appropriateness of medical treatment and, as a result, hospital efficiency. According to Garson’s Indexes, the most significant variables are exertion, the absence of symptoms, and the patient’s gender. On the contrary, cardio-vascular history, hypertension, and age have the lowest impact on the determination of the subject’s health status. The main application of this new technology is the adoption of smart solutions (e.g., a mobile app) to customize the stratification of patients admitted to emergency departments (ED)s after a syncope event. Indeed, the adoption of these smart solutions gives the opportunity to customize risk stratification according to the specific clinical case (i.e., the patient’s health status) and the physician’s decision-making process (i.e., the desired levels of sensitivity and specificity). Moreover, a decision-making process based on these smart solutions might ensure a more effective use of available resources, improving the management of syncope patients and reducing the cost of inappropriate treatment and hospitalization.



Similar content being viewed by others
Notes
The tansigmoidal function has a logsigmoidal form with a codomain range from − 1 to + 1.
References
Cournane S, Conway R, Creagh D, Byrne DG, Silke B (2015) Consultant duration of clinical practice as a cost determinant of an emergency medical admission. Eur J Health Econ 2015(16):561–567. https://doi.org/10.1007/s10198-014-0619-z
Eriksen BO, Førde OH, Kristiansen IS et al (2000) Cost savings and health losses from reducing inappropriate admissions to a department of internal medicine. Int J Technol Assess Health Care 16(4):1147–1157
Lee A, Clarke B, Hazlett SC et al (2003) How to minimize inappropriate utilization of Accident and Emergency Departments: improve the validity of classifying the general practice cases amongst the A&E attendees. Health Policy 66(2):159–168. https://doi.org/10.1016/S0168-8510(03)00023-X
Casagranda I, Costantino G, Falavigna G, Furlan R, Ippoliti R (2016) Artificial Neural Networks and risk stratification models in Emergency Departments: the policy maker’s perspective. Health Policy 120(1):111–119
Weingart S, Wyer P (2006) Emergency medicine decision making: critical choices in chaotic environments. McGraw-Hill, New York
McDonagh MS, Smith DH, Goddard M (2000) Measuring appropriate use of acute beds. A systematic review of methods and results. Health Policy 53(3):157–184. https://doi.org/10.1016/s0168-8510(00)00092-0
Fellin G, Apolone G, Tampieri A et al (1995) Appropriateness of hospital use: an overview of Italian studies. Int J Qual Health Care 7(3):219–225
Propper C, Burgess S, Green K (2004) Does competition between hospitals improve the quality of care? Hospital death rates and the NHS internal market. J Public Econ 88(7–8):1247–1272
Chua CL, Palangkaraya A, Yong J (2010) A two-stage estimation of hospital quality using mortality outcome measure: an application using hospital administrative data. Health Econ 19:1404–1424. https://doi.org/10.1002/hec.1560
Ippoliti R, Falavigna G (2012) Efficiency of medical care industry: evidence from the Italian regional system. Eur J Oper Res 217(2012):643–652. https://doi.org/10.1016/j.ejor.2011.10.010
Quaglio GL, Karapiperis T, Van Woensel L et al (2013) Austerity and health in Europe. Health Policy 113(1):13–19. https://doi.org/10.1016/j.healthpol.2013.09.005
Ippoliti R, Falavigna G, Grosso F, Maconi A, Randi L, Numico G (2018) The economic impact of clinical research in an Italian public hospital: the malignant pleural mesothelioma case study. Int J Health Policy Manag 7(8):728–737. https://doi.org/10.15171/ijhpm.2018.13
De Vos P, Orduñez-García P, Santos-Peña M et al (2010) Public hospital management in times of crisis: lessons learned from Cienfuegos, Cuba (1996–2008). Health Policy 96(1):64–71. https://doi.org/10.1016/j.healthpol.2010.01.005
Ippoliti R, Allievi I, Falavigna G, Rizzi S, Moda G (2018) The sustainability of a community nurses programme aimed at supporting active ageing in mountain areas. Int J Health Plan Manag. https://doi.org/10.1002/hpm.2591 (forthcoming)
Costantino G, Falavigna G, Solbiati M, Furlan R, Ippoliti R (2017) Neural networks as a tool to predict syncope risk in the Emergency Department. Europace 19(11):1891–1895. https://doi.org/10.1093/europace/euw336
Costantino G, Sun B, Barbic F et al (2015) Syncope clinical management in the ED: a consensus from the first international workshop on syncope risk stratification in the ED. Eur Heart J. https://doi.org/10.1093/eurheartj/ehv378
Sun B, Costantino G, Barbic F et al (2014) Priorities for emergency department syncope research. Ann Emerg Med 64(6):649–655. https://doi.org/10.1016/j.annemergmed.2014.04.014
Quinn J, McDermott D, Stiell I, Kohn M, Wells G (2006) Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann Emerg Med 47(5):448–454
Costantino G, Furlan R (2013) Syncope risk stratification in the emergency department. Cardiol Clin 31(2013):27–38. https://doi.org/10.1016/j.ccl.2012.10.003
Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA (2004) Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med 43(2):224–232
Quinn J, McDermott D (2011) Electrocardiogram findings in emergency department patients with syncope. Acad Emerg Med 18(7):714–718
Dipaola F, Costantino G, Perego F et al (2010) San Francisco syncope rule, Osservatorio epidemiologico sulla sincope nel lazio risk score, and clinical judgment in the assessment of short-term outcome of syncope. Am J Emerg Med 2010(28):432–439
Constantino G, Perego F, Dipaola F et al (2008) Short and long-term prognosis of syncope, risk factors, and role of hospital admission. J Am Coll Cardiol 51(30):276–283
Del Rosso A, Ungar A, Maggi R et al (2008) Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: the EGSYS score. Heart 94:1620–1626
Efron B, Tibshirani RJ (1994) An introduction to the bootstrap. CRC Press, Boca Raton
Trichakis I, Nikolos I, Karatzas GP (2011) Comparison of bootstrap confidence intervals for an ANN model of a karstic aquifer response. Hydrol Process 25(18):2827–2836
Falavigna G (2008) New contents and perspectives in the risk analysis of enterprises. Int J Bus Perform Manag 10(2/3):136–173
Heckerling PS, Canaris GJ, Flach SD, Tape TG, Wigton RS, Gerber BS (2007) Predictors of urinary tract infection based on artificial neural networks and genetic algorithms. Int J Med Inform 76(4):289–296
Tenório JM, Hummel AD, Cohrs FM, Sdepanian VL, Pisa IT, de Fátima Marin H (2011) Artificial intelligence techniques applied to the development of a decision–support system for diagnosing celiac disease. Int J Med Inform 80(11):793–802
Ellenius J, Groth T (2000) Methods for selection of adequate neural network structures with application to early assessment of chest pain patients by biochemical monitoring. Int J Med Inform 57(2–3):181–202
Parmanto B, Deneault LG, Denault AY (2001) Detection of hemodynamic changes in clinical monitoring by time-delay neural networks. Int J Med Inform 63(1–2):91–99
Baxt WG, Shofer FS, Sites FD, Hollander JE (2002) A neural network aid for the early diagnosis of cardiac ischemia in patients presenting to the emergency department with chest pain. Ann Emerg Med 40(6):575–583
Harrison RF, Kennedy RL (2005) Artificial neural network models for prediction of acute coronary syndromes using clinical data from the time of presentation. Ann Emerg Med 46(5):431–439
Bektaş F, Eken C, Soyuncu S et al (2008) Artificial neural network in predicting craniocervical junction injury: an alternative approach to trauma patients. Eur J Emerg Med 15(6):318–323. https://doi.org/10.1097/MEJ.0b013e3282fce7af
Hornik K, Stinchcombe M, White H (1989) Multilayer feedforward networks are universal approximators. Neural Netw 2:359–366
Kim KJ (2003) Financial time series forecasting using support vector machines. Neurocomputing 55(1):307–319
Min JH, Lee YC (2005) Bankruptcy prediction using support vector machine with optimal choice of kernel function parameters. Expert Syst Appl 28(4):603–614
Patuwo E, Hu MY, Hung MS (1993) Two-group classification using neural networks. Decis Sci 24(4):825–845
Nath R, Rajagopalan B, Ryker R (1997) Determining the saliency of input variables in neural network classifiers. Comput Oper Res 24(8):767–773
Chauhan N, Ravi V, Karthik Chandra D (2009) Differential evolution trained wavelet neural networks: application to bankruptcy prediction in banks. Expert Syst Appl 36(4):7659–7665
Salchenberger LM, Cinar E, Lash NA (1992) Neural networks: a new tool for predicting thrift failures. Decis Sci 23(4):899–916
Olmeda I, Fernández E (1997) Hybrid classifiers for financial multicriteria decision making: the case of bankruptcy prediction. Comput Econ 10(4):317–335
Garson GD (1991) Interpreting neural-network connection weights. AI Expert 6(4):46–51
Kohonen T (1990) The self-organizing map. Proc IEEE 78(9):1464–1480
Falavigna G (2012) Financial ratings with scarce information: a neural network approach. Expert Syst Appl 39(2):1784–1792. https://doi.org/10.1016/j.eswa.2011.08.074 (ISSN: 0957-4174)
Reid MC, Lane DA, Feinstein AR (1998) Academic calculations versus clinical judgments: practicing physicians’ use of quantitative measures of test accuracy. Am J Med 104(4):374–380
Gardner M, Altman DG (2000) Statistics with confidence: confidence intervals and statistical guidelines. BMJ Books, London
McGee S (2002) Simplifying likelihood ratios. J Gen Intern Med 17(8):647–650. https://doi.org/10.1046/j.1525-1497.2002.10750.x
Henderson MC, Tierney LM, Smetana GW (2012) The patient history, 2nd edn. McGraw-Hill, New York, p 30 (ISBN 978-0-07-162494-7)
Kunene KN, Weistroffer HR (2008) An approach for predicting and describing patient outcome using multicriteria decision analysis and decision rules. Eur J Oper Res 185(3):984–997
West D, Mangiameli P, Rampal R, West V (2005) Ensemble strategies for a medical diagnostic decision support system: a breast cancer diagnosis application. Eur J Oper Res 162(2):532–551
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This is a retrospective analysis on anonymous data, previously collected by the hospitals, without formal ethical approval according to national law.
Informed consent
Patients’ informed consents have been collected by the hospitals before treatments and clinical procedures.
Rights and permissions
About this article
Cite this article
Falavigna, G., Costantino, G., Furlan, R. et al. Artificial neural networks and risk stratification in emergency departments. Intern Emerg Med 14, 291–299 (2019). https://doi.org/10.1007/s11739-018-1971-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1971-2