Abstract
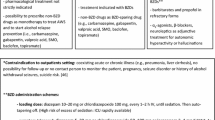
The chronic use of alcohol can lead to the onset of an alcohol use disorder (AUD). About 50% of subjects with an AUD may develop alcohol withdrawal syndrome (AWS) when they reduce or discontinue their alcohol consumption and, in 3–5% of them, convulsions and delirium tremens (DTs), representing life-threatening complications, may occur. Unfortunately, few physicians are adequately trained in identifying and treating AWS. The Italian Society on Alcohol has, therefore, implemented a task force of specialists to draw up recommendations for the treatment of AWS with the following main results: (1) while mild AWS may not require treatment, moderate and severe AWS need to be pharmacologically treated; (2) out-patient treatment is appropriate in patients with mild or moderate AWS, while patients with severe AWS need to be treated as in-patients; (3) benzodiazepines, BDZs are the “gold standard” for the treatment of AWS and DTs; (4) alpha-2-agonists, beta-blockers, and neuroleptics may be used in association when BDZs do not completely resolve specific persisting symptoms of AWS; (5) in the case of a refractory form of DTs, the use of anaesthetic drugs (propofol and phenobarbital) in an intensive care unit is appropriate; (6) alternatively to BDZs, sodium oxybate, clomethiazole, and tiapride approved in some European Countries for the treatment of AWS may be employed for the treatment of moderate AWS; (7) anti-convulsants are not sufficient to suppress AWS, and they may be used only in association with BDZs for the treatment of refractory forms of convulsions in the course of AWS.


Similar content being viewed by others
References
World Health Organization (WHO) (2014) Global status report on alcohol and health. World Health Organization, Geneva
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5, 5th edn. The American Psychiatric Association, Washington, DC
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS (2015) Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry 72:757–766
de Wit M, Jones DG, Sessler CN, Zilberberg MD, Weaver MF (2010) Alcohol-use disorders in the critically ill patient. Chest 138:994–1003
Rehm J, Mathers C, Popova S et al (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373:2223–2233
Schuckit MA (2014) Recognition and management of withdrawal delirium (delirium tremens). N Engl J Med 371:2109–2113
Istituto Superiore di Sanità (2002) National programme of guidelines. Istituto Superiore di Sanità, Rome
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J et al (2011) GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol 64:1277–1282
Schünemann HJ, Jaeschke R, Cook D, Bria W, El-Solh A, Ernst A et al (2006) An official ATS statement: grading the quality of evidence and strength of recommendations in ATS guidelines and recommendations. Am J Respir Crit Care Med 174:605–614
Reus VI, Fochtmann LJ, Bukstein O et al (2018) The American Psychiatric Association practice guideline for the pharmacological treatment of patients with alcohol use disorder. Am J Psych 175:86–90
Pilling S, Yesufu-Udechuku A, Taylor C, Drummond C, Guideline Development Group (2011) Diagnosis, assessment, and management of harmful drinking and alcohol dependence: summary of NICE guidance. BMJ 342:d700
Rolland B, Paille F, Gillet C, Rigaud A, Moirand R, Dano C, Dematteis M, Mann K, Aubin HJ (2016) Pharmacotherapy for alcohol dependence: the 2015 recommendations of the French alcohol society, issued in partnership with the european federation of addiction societies. CNS Neurosci Ther 22:25–37
Soyka M, Kranzler HR, Hesselbrock V, Kasper S, Mutschler J, Möller HJ, WFSBP Task Force on Treatment Guidelines for Substance Use Disorders (2017) Guidelines for biological treatment of substance use and related disorders, part 1: alcoholism, first revision. World J Biol Psychiatry 18:86–119
Schuckit MA (2006) Drug and alcohol abuse. A clinical guide to diagnosis and treatment, 6th edn. Springer, New York
Vonghia L, Leggio L, Ferrulli A et al (2008) Alcohol acute intoxication. Eur J Int Med 19:561–567
Tabakoff B, Hoffman PL (2013) The neurobiology of alcohol consumption and alcoholism: an integrative history. Pharmacol Biochem Bheav 113:20–37
Shpilenya LS, Muzychenko AP, Gasbarrini G, Addolorato G (2002) Metadoxine in acute alcohol intoxication. A double-blind, randomized, placebo-controlled study. Alcohol Clin Exp Res 26:340–346
Pianca TG, Sordib AO, Hartmannb TC, von Diemen L (2017) Identification and initial management of intoxication by alcohol and other drugs in the pediatric emergency room. J Pediatr 93:46–52
Lamminpää A (1994) Acute alcohol intoxication among children and adolescent. Eur J Pediatr 153:868–872
Grüne B, Piontek D, Pogarell O, Grübl A, Groß C, Reis O, Zimmermann US, Kraus L (2017) Acute alcohol intoxication among adolescents-the role of the context of drinking. Eur J Pediatr 176:31–39
Ministry of Health (2017) Annual Report of the Ministry of Health to the Parliament about the interventions on alcohol related problems
Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM (2010) Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 304:527–535
Arnaud N, Diestelkamp S, Wartberg L, Sack PM, Daubmann A, Thomasius R (2017) Short to midterm effectiveness of brief motivational intervention to reduce alcohol use and related problems for alcohol intoxicated children and adolescents in pediatric emergency department: a randomized controlled trial. Acad Emerg Med 24:186–200
Wiese JG, Shlipak MG, Browner WS (2000) The alcohol hangover. Ann Intern Med 132:897–902
Penning R, McKinney A, Verster JC (2012) Alcohol Hangover symptoms and their contribution to the overall hangover severity. Alcohol Alcohol 47:248–252
Jayawardena R, Thejani T, Ranasinghe P, Fernando D, Verster JC (2017) Intervention for treatment of alcohol hangover: systematic review. Hum Psychopharm. https://doi.org/10.1002/hup.2600
Koob GF, Le Moal M (2006) Alcohol. In: Koob GF, Le Moal M (eds) Neurobiology of addiction. Oxford Academic Press, Oxford, pp 173–241
Mayo-Smith MF (1997) Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 278:144–151
Amato L, Minozzi S, Davoli M (2011) Efficacy and safety of pharmacological interventions for the treatment of the Alcohol Withdrawal Syndrome. Cochrane Database Syst Rev 6:CD008537
Mirijello A, D’Angelo C, Ferrulli A, Vassallo G, Antonelli M, Caputo F, Leggio L, Gasbarrini A, Addolorato G (2015) Identification and management of alcohol withdrawal syndrome. Drugs 75:353–365
Jesse S, Bråthen G, Ferrara M, Keindl M, Ben-Menachem E, Tanasescu R, Brodtkorb E, Hillbom M, Leone MA, Ludolph AC (2017) Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurol Scand 135:4–16
Mayo-Smith MF, Beecher LH, Fischer TL et al (2004) Management of alcohol withdrawal delirium. An evidence-based practice guideline. Arch Intern Med 164:1405–1412
Galvin R, Bråthen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA (2010) EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol 17:1408–1418
Attilia F, Perciballi R, Rotondo C, Capriglione I, Iannuzzi S, Attilia ML, Coriale G, Vitali M, Cereatti F, Fiore M, Ceccanti M, interdisciplinary study group CRARL, SITAC, SIPAD, SITD, SIPD (2018) Alcohol withdrawal syndrome: diagnostic and therapeutic methods. Sindrome astinenziale da alcol: processi diagnostici e terapeutici. Riv Psichiatr 53:118–122
Long D, Long B, Koyfman A (2017) The emergency medicine management of severe alcohol withdrawal. Am J Emerg Med 35:1005–1011
Agabio R (2005) Thiamine administration in alcohol-dependent patients. Alcohol Alcohol 40:155–156
Sarai M, Tejani AM, Chan AH, Kuo IF, Li J (2013) Magnesium for alcohol withdrawal. Cochrane Database Syst Rev 6:CD008358
Espay AJ (2014) Neurologic complications of electrolyte disturbances and acid-base balance. Handb Clin Neurol 119: 365–382
Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM (1989) Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 84:1353–1357
Perry EC (2014) Inpatient management of acute alcohol withdrawal syndrome. CNS Drugs 28:401–410
Muncie HL Jr, Yasinian Y, Oge’ L (2013) Outpatient management of alcohol withdrawal syndrome. Am Fam Phys 88:589–595
Caputo F, Bernardi M (2010) Medications acting on the GABA system in the treatment of alcoholic patients. Curr Pharm Des 16:2118–2125
Muzyk AJ, Leung JG, Nelson S et al (2013) The role of diazepam loading for the treatment of alcohol withdrawal syndrome in hospitalized patients. Am J Addict 22:113–118
Schmidt KJ, Doshi MR, Holzhausen JM, Natavio A, Cadiz M, Winegardner JE (2016) Treatment of severe alcohol withdrawal. Ann Pharmacother 50:389–401
Mo Y, Thomas MC, Karras GE (2016) Barbiturates for the treatment of alcohol withdrawal syndrome: a systematic review of clinical trials. J Crit Care 32:101–107
Dixit D, Endicott J, Burry L, Ramos L, Yeung SY, Devabhakthuni S, Chan C, Tobia A, Bulloch MN (2016) Management of acute alcohol withdrawal syndrome in critically ill patients. Pharmacotherapy 36:797–822
Liang C, Chen J, Gu W, Wang H, Xue Z (2011) Chronic alcoholism increases the induction dose of propofol. Acta Anaesthesiol Scand 55:1113–1137
Wong A, Benedict NJ, Lohr BR, Pizon AF, Kane-Gill SL (2015) Management of benzodiazepine-resistant alcohol withdrawal across a healthcare system: benzodiazepine dose-escalation with or without propofol. Drug Alchol Depend 154:296–299
Brotherton AL, Hamilton EP, Kloss HG, Hammond DA (2016) Propofol for treatment of refractory alcohol withdrawal syndrome: a review of the literature. Pharmacotheraphy 36:433–442
Rosenson J, Clements C, Simon B et al (2013) Phenobarbital for acute alcohol withdrawal: a prospective randomized double-blind placebo-controlled study. J Emerg Med 44:592–598
Agence nationale de sècuritè du mèdicament (ANSM) (2017) Recommandation temporaire d'utilisation (RTU) du balcofene dans la prise en charge des patients alcoolo-dependants
Agabio R, Carai AM, Gessa GL, Colombo G (2010) Gamma-hydroxybutyric acid (GHB). In: Koob GF, Le Moal M, Thompson RF (eds) Encyclopedia of behavioral neuroscience. Oxford Academic Press, Oxford, pp 76–83
Snead OC, Gibson KM (2005) Gamma-hydroxybutyric acid. N Engl J Med 352:2721–2732
Leone MA, Vigna-Taglianti F, Avanzi G et al (2010) Gamma-hydroxybutyrate (GHB) for treatment of alcohol withdrawal and prevention of relapses. Cochrane Database Syst Rev 2:CD006266
Skala K, Caputo F, Mirijello A et al (2014) Sodium oxybate in the treatment of alcohol dependence: from the alcohol withdrawal syndrome to the alcohol relapse prevention. Exp Opin Pharmacother 15:245–257
Keating GM (2014) Sodium oxybate: a review of its use in alcohol withdrawal syndrome and in maintenance of abstinence in alcohol dependence. Clin Drug Investig 34:63–80
Gessa GL, Agabio R, Carai M, Lobina C, Pani M, Reali R, Colombo G (2000) Mechanism of the anti-alcohol effect of gamma hydroxybutyric acid (GHB). Alcohol 20:271–276
Addolorato G, Balducci G, Capristo E et al (1999) Gamma-hydroxybutyric acid (GHB) in the treatment of alcohol withdrawal syndrome: a randomized comparative study versus benzodiazepine. Alcohol Clin Exp Res 23:1596–1604
Caputo F, Skala K, Mirijello A, Ferrulli A, Walter H, Lesch O, Addolorato G (2014) Sodium oxybate in the treatment of alcohol withdrawal syndrome: a randomized double-blind comparative study versus oxazepam. The GATE 1 trial. CNS Drugs 28:743–752
Addolorato G, Leggio L (2010) Safety and efficacy of baclofen in the treatment of alcohol-dependent patients. Curr Pharm Des 16:2113–2117
Agabio R, Colombo G (2014) GABAB receptor ligands for the treatment of alcohol use disorder: preclinical and clinical evidence. Front Neurosci 8:140
Agabio R, Leite-Morris K, Addolorato G, Colombo G (2016) Targeting the GABAB receptor for the treatment of alcohol use disorder. In: Colombo G (ed) GABAB receptor. Springer, Cham
Addolorato G, Leggio L, Abenavoli L, Agabio R, Caputo F, Capristo E, Colombo G, Gessa GL, Gasbarrini G (2006) Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs diazepam. Am J Med 119:13–18
Liu J, Wang LN (2017) Baclofen for alcohol withdrawal. Cochrane Datatabase Syst Rev 8:008502
Nimmerrichter AA, Walter H, Gutierrez-Lobos KE, Lesch OM (2002) Double blind controlled trial of gamma-hydroxybutyrate and clomethiazole in the treatment of alcohol withdrawal. Alcohol Alcohol 37:67–73
Hillemacher T, Weinland C, Heberlein A, Wilhelm J, Bayerlein K, Kornhuber J, Frieling H, Bleich S (2008) Treatment with clomethiazole is associated with lower rates of premature discharge during alcohol withdrawal. Pharmacopsychiatry 41:134–137
Scatton B, Cohen C, Perrault G et al (2001) The preclinical pharmacologic profile of tiapride. Eur Psychiatry 16:29s–34s
Allain H, Dauzenberg PH, Maurer K, Schuck S, Bonhomme D, Gerard D (2000) Double blind study of tiapride versus haloperidol and placebo agitation and aggressiveness in elderly patients with cognitive impairment. Psychopharmacology 148:361–366
Peters DH, Faulds D (1994) Tiapride. A review of its pharmacology and therapeutic potential in the management of alcohol dependence syndrome. Drugs 47:1010–1032
Murphy DJ, Shaw GK, Clarke I (1983) Tiapride and chlormethiazole in alcohol withdrawal: a double-blind trial. Alcohol Alcohol 18:227–237
Soyka M, Morhart-Klute V, Horak M (2002) A combination of carbamazepine/tiapride in outpatient alcohol detoxification-results from an open clinical study. Eur Arch Psychiatry Clin Neurosci 252:197–200
Soyka M, Schmidt P, Franz M, Barth T, De Groot M, Kienast T et al (2006) Treatment of alcohol withdrawal syndrome with a combination of tiapride/carbamazepine: results of a pooled analysis in 540 patients. Eur Arch Psychiatry Clin Neurosci 256:395–401
Martinotti G, di Nicola M, Frustaci A, Romanelli R, Tedeschi D, Guglielmo R, Guerriero L, Bruschi A, De Filippis R, Pozzi G, Di Giannantonio M, Bria P, Janiri L (2010) Pregabalin, tiapride and lorazepam in alcohol withdrawal syndrome: a multi-centre, randomized, single-blind comparison trial. Addiction 105:288–299
Minozzi S, Amato L, Vecchi S, Davoli M (2010) Anticonvulsants for alcohol withdrawal. Cochrane Database Syst Rev 3:CD005064
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of alcohol-related liver disease. J Hepatol 69:154–181
Leggio L, Lee MR (2017) Treatment of alcohol use disorder in patients with alcoholic liver disease. Am J Med 130:124–134
Addolorato G, Mirijello A, Barrio P, Gual A (2016) Treatment of alcohol use disorders in patients with alcoholic liver disease. J Hepatol 65:618–630
Caputo F, Bernardi M, Zoli G (2011) Efficacy and safety of γ-hydroxybutyrate in treating alcohol withdrawal syndrome in an alcohol-dependent inpatient with decompensated liver cirrhosis: a case report. J Clin Psychopharmacol 31:140–141
Marengoni A, Onder G (2015) Guidelines, polypharmacy, and drug–drug interactions in patients with multimorbidity. BMJ. https://doi.org/10.1136/bmj.h1059
Guerzoni S, Pellesi L, Pini LA, Caputo F (2018) Drug-drug interactions in the treatment for alcohol use disorders: a comprehensive review. Pharmacol Res 133:65–76
Ozdemir M, Aktan Y, Boydag BS, Cingi MI, Musmul A (1998) Interaction between grapefruit juice and diazepam in humans. Eur J Drug Metab Pharmacokinet 23:55–59
Tanaka E, Misawa S (1998) Pharmacokinetic interactions between acute alcohol ingestion and single doses of benzodiazepines, and tricyclic and tetracyclic antidepressants—an update. J Clin Pharm Ther 23:331–336
Caputo F, Francini S, Stoppo M, Lorenzini F, Vignoli T, Del Re A, Comaschi C, Leggio L, Addolorato G, Zoli G, Bernardi M (2009) Incidence of craving for and abuse of gamma-hydroxybutyric acid (GHB) in different populations of treated alcoholics: an open comparative study. J Psychopharmacol 23:883–890
Thai D, Dyer JE, Benowitz NL, Haller CA (2006) GHB and ethanol effects and interactions in humans. J Clin Psychopharmacol 26:524–529
Pross N, Patat A, Vivet P, Bidaut M, Fauchoux N (2015) Pharmacodynamic interactionsof a solid formulation of sodium oxybate and ethanol in healthy volunteers. Br J Clin Pharmacol 80:480–492
Bonnet U, Lensing M, Specka M, Scherbaum N (2011) Comparison of two oral symptom-triggered pharmacological inpatient treatments of acute alcohol withdrawal: clomethiazole vs. clonazepam. Alcohol Alcohol 46:68–73
Lugoboni F, Mirijello A, Faccini M, Casari R, Cossari A, Musi G, Bissoli G, Quaglio G, Addolorato G (2014) Quality of life in a cohort of high-dose benzodiazepine dependent patients. Drug Alchol Depend 142C:105–109
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Statement of human and animal rights
The Italian Society on Alcohol has followed the Ethical Statements required for a review paper.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Caputo, F., Agabio, R., Vignoli, T. et al. Diagnosis and treatment of acute alcohol intoxication and alcohol withdrawal syndrome: position paper of the Italian Society on Alcohol. Intern Emerg Med 14, 143–160 (2019). https://doi.org/10.1007/s11739-018-1933-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1933-8