Abstract
The management of major bleeding in patients treated with direct oral anticoagulants (DOACs) is still not well established. START-Events, a branch of the START registry (Survey on anTicoagulated pAtients RegisTer) (NCT02219984), aims to describe the actual management of bleeding or recurrent thrombotic events in routine clinical practice. We here present the results of the management of bleeding patients. The START-Event registry is a prospective, observational, multicenter, international study. Baseline characteristics (demographic, clinical, risk factors) of patients, laboratory data at admission and during follow-up, site of bleeding, therapeutic strategies, and outcomes at the time of hospital discharge and after 6 months were recorded on a web-based case report form. Between January 2015 and December 2016, 117 patients with major bleeding events were enrolled. Non-valvular atrial fibrillation (NVAF) was the indication for treatment in 84% (62% males); 53 patients had intracranial bleeding (13 fatal), 42 had gastrointestinal bleeding (1 fatal), and 22 had bleeding in other sites. Therapeutic interventions for the management of bleeding were performed in 71% of patients. Therapeutic strategies with/without surgery or invasive procedures included: fluid replacement or red blood cells transfusion, prothrombin complex concentrates (3 or 4 factors), antifibrinolytic drugs, and the administration of idarucizumab. Creatinine, blood cell count, and PT/aPTT were the most frequent tests requested, while specific DOAC measurements were performed in 23% of patients. Mortality during hospitalization was 11.9%, at 6-month follow-up 15.5%. Our data confirm a high heterogeneity in the management of bleeding complications in patients treated with DOACs.
Similar content being viewed by others
Introduction
In the past few years, direct oral anticoagulants (DOACs) have been introduced in clinical practice for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation (NAVF), and for the prevention and treatment of venous thromboembolism (VTE) [1].
At present, available drugs include dabigatran, a selective anti-factor IIa molecule and three direct factor Xa inhibitors: apixaban, edoxaban, and rivaroxaban. In phase III clinical studies, all these agents have shown non-inferiority or superiority compared with vitamin K antagonists (VKA) in terms of efficacy and safety [2,3,4,5,6].
Due to their pharmacological characteristics (i.e., rapid onset of action, short half-life, predictable anticoagulant effect in standard conditions, low food/drug interactions without any important need for restrictions, metabolism, and elimination), the DOACs allow fixed dose administration, and do not require laboratory monitoring [7, 8].
However, the measurement of the activity of the DOACs provides clinically useful information in a number of special conditions such as in the case of bleeding or thromboembolic complications while on treatment to evaluate a correlation between events and over/under treatment, and to address specific treatment approaches [9,10,11,12,13].
Major bleeding during anticoagulant treatment remains a crucial issue, with estimated incidences ranging from 2 to 3% in clinical trials [6] to up to 4% in observational post-marketing studies [14]. Yet, the optimal management of bleeding complications on DOACs therapy is still poorly defined given that the limited evidence to support different therapeutic approaches. Reversal agents are still under investigation, and currently only idarucizumab [15], the specific antidote for dabigatran, is available in the market. Andexanet alfa, the reversal agent for direct and indirect factor Xa inhibitors, is still under investigation [16, 17], whereas more preliminary data are available for ciraparantag, a universal antidote [18]. Similarly, the efficacy and safety of the administration of procoagulant factors, which are suggested by international guidelines [8, 11] for patients on direct Factor Xa inhibitors, is uncertain [19].
START-SSC Events, a branch of the START registry (Survey on anTicoagulated pAtients RegisTer) (NCT02219984) [20] promoted through the Scientific and Standardization Committee (SSC) Control of Anticoagulation of the International Society of Thrombosis and Haemostasis, aims to describe the actual management of bleeding or recurrent thrombotic events in patients treated with the DOACs in routine clinical practice. In this study, we describe the management of major bleeding with respect to therapeutic strategies (medical therapies, surgery, or interventional procedures), laboratory testing, and other supportive measures, and we describe the adherence to currently available guidelines and recommendations in clinical practice.
Methods
Patients
START-SSC Events is a prospective, observational, multicenter, international registry that includes patients with acute complications during treatment with DOACs. The study was conducted in 15 centers among 7 different countries (Belgium, Brazil, Germany, Italy, Switzerland, USA, and Thailand). All participating centers are asked to report in the registry all available clinical and laboratory data collected in consecutive patients aged more than 18 years presenting with major bleeding or thromboembolic complications. In this article, we only report data on patients presenting with major bleeding events.
The study protocol of START-SSC Event registry was approved by the local ethics committees, and was conducted in accordance with the Declaration of Helsinki. Written informed consent was collected according to local practice.
Data collection
Baseline characteristics (age, gender, type of DOAC, clinical indication), laboratory findings at admission and during follow-up, site of bleeding, diagnostic procedures, therapeutic strategies, and outcomes at the time of hospital discharge and after 6 months were recorded on a web-based case report form (CRF). Information was collected by the local investigators, and central monitoring of the quality of data was performed at the coordinating center. Investigators were contacted in case of missing values or discrepancies. The 6-month follow-up visits were performed at the participating clinics or by phone contact. Laboratory tests included: blood cell count, liver enzymes (AST, ALT), renal function (creatinine clearance calculated using the Cockcroft–Gault formula), coagulation screening tests (PT and aPTT), and specific DOAC measurements. DOACs levels, expressed as drug concentration equivalent (ng/ml), were measured with diluted thrombin time (dTT) or ecarin chromogenic assay (ECA) calibrated for dabigatran and specific anti-factor X activated (FXa) assays calibrated for apixaban, edoxaban, and rivaroxaban [12, 21, 22]. All tests were performed locally, and each investigator made decision on whether to perform laboratory or not.
Major bleeding and outcomes
In this study, we adopted the criteria of the International Society on Thrombosis and Haemostasis, which defines major bleeding as fatal bleeding or symptomatic bleeding in critical area or organ, or bleeding causing a fall of hemoglobin level of 20 g/L (1.24 mmol/L or 2 g/dL) or more, or leading to transfusion of ≥ 2 units of whole blood or red cells [23].
Study outcomes during follow-up include mortality and disability. The Barthel index [24] was used to define disability, and dependence in activities of daily living was assessed by the local investigator at the time of hospital discharge and after 6 months. Disability [evaluated for intracranial hemorrhage (ICH) patients only] was defined by a score < 100 of Barthel index.
Guidelines
Routine strategies described in the study were compared with the recommendations of international guidelines. We referred to the guidelines published by European Heart Rhythm Association (EHRA) in 2016 [11]. In brief, the following procedures are recommended in case of major bleeding events: stop DOACs; provide patient stabilization (assessment of vital signs, fluid resuscitation, mechanical compression); identify the DOAC taken by the patient and the time of the last dose intake; check for blood cell count, renal and liver function, screening coagulation tests, or specific DOAC measurements; add symptomatic treatment (fluid replacement, blood transfusion); treat bleeding cause if possible (e.g., in case of gastrointestinal bleeding); consider possible surgical intervention or invasive procedures; add oral charcoal if the DOAC was recently ingested; and consider the use of a specific antidote or by pass hemostatic agents [prothrombin complex concentrates (PCC), 4 factors if available, or activated prothrombin complex concentrates (aPCC), or rFVIIa].
Statistical analysis
Descriptive analysis was performed. Continuous variables are expressed as median and interquartile (IQR) or as median and range. Categorical variables are expressed as frequencies and percentages. The SPSS software for Windows, version 22 (SPSS Inc, Chicago, IL), was used for data processing.
Results
Patient characteristics
Between January 1, 2015 and December 31, 2016, 117 patients with major bleeding on DOACs were enrolled in the study: 32 patients were on apixaban (63 and 37% taking 5 or 2.5 mg twice-daily, respectively), 32 on dabigatran (75 and 25% taking 150 or 110 mg twice daily, respectively), 51 on rivaroxaban (61 and 39% taking 20 or 15 mg once-daily, respectively), and two on edoxaban (both taking 60 mg once-daily). The patient baseline characteristics, sites of major bleeding and outcomes are summarized in Table 1. NVAF was the main clinical indication (84%). Overall, 42% of patients who experienced major bleeding complications were on low-dose NOAC treatment, 11% were treated concomitantly with antiplatelet drugs, and 30% were previously shifted from AVK to DOACs. Time of last dose intake was available in 49% of patients and varied from 4 to 12 h.
Bleeding characteristics
Bleeding events occurred during the first 90 days of DOAC treatment in 45% of patients. The site of bleeding was intracranial in 53 patients (13 were fatal and one of them occurred in a patient treated concomitantly with ticagrelor and rivaroxaban), gastrointestinal in 42 (1 fatal), and 22 patients had major bleeding in other sites (Table 1). Of all bleeding events, 94 (80.4%) were spontaneous while 23 (19.6%) were post-traumatic. Within post-traumatic complications, we observed: 14/53 ICH (12 subdural, 1 lobar, and 1 deep), 2/42 gastrointestinal ,and 7/7 muscular hematoma. In Table 2, the cases in whom it was possible to calculate whether the drug administered was under- or over-dosed are shown.
Bleeding management
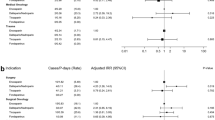
The therapeutic strategies used for bleeding management are reported in Table 3. In summary: among the 117 patients, no therapeutic intervention was adopted in 34 (29%), while the other 83 patients (71%), received one or more than one of the therapies listed in Table 3. Idarucizumab 5gr/IV was administered in 3 out of 51 patients treated with dabigatran (5.8%): two with ICH and one with retroperitoneal hemorrhage. Management strategies for bleeding were considered to be adherent with what suggested by current international guidelines (10) in nearly 70% of them (see Table 3).
Laboratory findings
Table 4 shows the available data regarding the median levels (and range) measured before and after intervention (when available). Specific DOAC measurements, expressed as drug concentration equivalent (ng/mL), were available in only 23% of cases pre-treatment and 10% post-treatment. In only one patient with post-traumatic subdural ICH, plasma concentration of dabigatran was measured before (188 ng/mL) and after (3 ng/mL) the administration of idarucizumab. The available individual results of specific drug measurements performed before and after intervention are shown in Table 5.
Outcomes at hospital discharge and at 6 months
Outcomes are summarized in Table 1. During hospitalization, 14 bleedings had a fatal outcome [11.9% of the total population: 13 ICH and 1 gastrointestinal (GI) bleeding], which occurred within 3 days after the acute event. At hospital discharge, 74% of all patients had complete resolution of signs of bleeding. When we consider ICH patients only, we observed complete resolution of symptoms in 24/53 patients (45.2%) and residual disability in 16/53 (30%).
At 6 months, among the 102 patients discharged, the complete resolution of symptoms was recorded in 85% of them. Four patients (two ICH, one GI, and one retroperitoneal bleeding) died because of later thrombotic complication. In particular, we registered three acute myocardial infarctions (AMI): one in a patient with ICH treated with prophylactic dose of LMWH, who developed pneumonia, one with retroperitoneal bleeding treated with low-dose dabigatran, and the third in a patient with GI bleeding and femoral fracture who suffered an AMI during treatment with low-dose apixaban. In addition, there was one sudden death in a patient with ICH who did not restart anticoagulation. The overall mortality of the entire cohort was 15.5%.
During follow-up, after the temporary interruption of DOACs, 38 patients (37% of survivors) restarted anticoagulation with the same drug, four patients (3.9%) shifted to another DOAC, two (2%) did not restart anticoagulation, and among the remaining patients 35 (35%) were treated with prophylactic doses of low molecular weight heparin, whereas 22 received VKA (22%). Only one patient with NVAF restarted antithrombotic therapy with low dose of aspirin. In one patient with VTE, a vena cava filter was implanted, and in another case, the anticoagulant treatment was interrupted and intermittent pneumatic compression was adopted. Overall, 2/99 (2%) of patients who restarted anticoagulant therapy had recurrent bleeding, and 3/99 (3%) experienced thrombotic events; among those who did not restart anticoagulant therapies, no one had recurrent bleeding events and 1/2 (50%) had thrombotic events, respectively.
Among the 22 patients who restarted anticoagulation with VKA, 13 (58%) had previously suffered GI bleeding and 2 (9%) ICH. Among the 42 patients who restarted anticoagulation with the DOACs, 14 (33%) had suffered GI bleeding and 11 (26%) ICH. No patients who resumed anticoagulation with VKA suffered major bleeding recurrence during 6 months of follow-up, whereas a recurrent major bleeding occurred in two patients who received DOACs (one was subsequently shifted to LMWH at prophylactic regimen, the other to VKA).
Among the 42 patients with GI bleeding, cancer was diagnosed in 3 (7%, all colorectal cancer) who were previously asymptomatic. One patient with diagnosis of GI cancer, who had complete resolution of bleeding at hospital discharge, was lost to follow-up.
Discussion
The DOACs have been shown to be safe and effective drugs for the treatment of venous thromboembolism and stroke prevention in NVAF when compared to vitamin K antagonists. However, as for all anticoagulant drugs, major spontaneous or post-traumatic bleedings may occur during DOAC treatment. Due to the increasing prevalence of patients who are treated with DOACs in the general population, major bleedings will become a relatively frequent event in the emergency departments with an urgent need for improving diagnostic and therapeutic tools, and specific strategies related to the site of bleeding, type of drugs, anticoagulant levels, necessity of surgical, or interventional procedures [11, 25].
Since patients are admitted to emergency departments after variable hours from the last DOAC dose intake and may present with several comorbidities, anticoagulant activity may not be exclusively predictable on the basis of the drug half-life and the evaluation of renal function, also because of the high inter–intra plasma level variability [26].
This study aims to describe how clinicians manage, at present, major bleeding complications in patients treated with DOACs. In the study, 117 patients with major bleedings are included, prevalently ICH and GI (45.3 and 35.9%, respectively) occurring in elderly NAVF or VTE patients. Most deaths in ICH patients (13/14; 92.8%) occur within the first 72 h from hospital admission. ICH-related mortality is 26.4%, similar to what is recently reported in the literature [27]. As shown in previous studies [27,28,29], ICH mortality in DOACs seems lower than in AVK, but, in any case, it concerns nearly one-fourth of total ICH in DOAC-treated patients.
In this study, we observe that nearly 50% of the total population received no treatment or symptomatic support only. Among ICH patients, nearly 30% were solely managed with interruption of DOAC administration and clinical monitoring.
The high mortality and disability rates associated to ICH bleeding strongly indicate a need for a rapid normalization of hemostasis. An approach only based on the evaluation of renal function and drug half-life may not guarantee a rapid normalization of hemostasis. We observe that symptomatic treatment is prevalently used in extra-cerebral bleedings, whereas PCCs, antifibrinolytic agents, and antidotes are mainly used in ICH bleedings. Fresh frozen plasma was used as symptomatic treatment in 22.2% of patients, all of them with extracranial bleedings, and three patients received vitamin K, which is not useful to reverse a DOAC activity.
More than 30% of the included patients were not treated in accordance with the international guidelines, mainly because they did not receive any specific treatment except for clinical surveillance (see Table 3). The therapeutic approaches among the study patients vary even when the site and severity of bleeding were the same, suggesting the absence of universally applied protocols.
During the 6-month follow-up, four deaths were observed due to thrombotic complications and accounting for the 3.9% of the total deaths. Bleeding case fatality rate is 11.9% and death occurred in 15.4% of the total population.
Only toward the end of our observational study was idarucizumab licensed in European countries. This explains why only 3 out of 53 dabigatran-treated patients received the reversal agent. We observe that only in one case, the antidote was administered after DOAC-specific measurement, opening the question about the risk of its overuse [30,31,32].
Clinicians requested laboratory tests, including blood cell count and screening coagulation test, in nearly 80% of patients, whereas specific DOAC measurements were obtained in only 23% of them, indicating that bleeding treatments were administered independently from objectively defined hemostatic assessment. This observation opens the question about the importance of laboratory testing in emergency clinical conditions to address appropriate treatments. As previously shown [21], global coagulation tests such as PT and aPTT are not useful to quantify DOAC activity, while specific tests (anti-Xa, dTT, ecarin test) are available and easily adaptable on most commercial coagulation platform. Despite the increasing consensus on the need for DOAC measurement in specific clinical conditions, our study shows a low rate of specific drug measurements in emergency situations, highlighting an urgent need for their implementation in each hospital.
In general, the approach to major bleeding in anticoagulated patients should be based on two main cornerstones: (1) symptomatic treatment of blood loss and treatment of the anatomical cause of bleeding and (2) reversal of the hemostatic impairment due to the anticoagulant drug, if present. In this perspective, laboratory testing and specific drug measurements should guide the management of patients.
Large phase III clinical studies [2,3,4,5,6] and post-marketing analysis [33, 34] indicate that major bleeding with the DOACs is associated with a more favorable outcome than with the vitamin K antagonists. Nevertheless, in the present study, major bleeding during DOAC treatment accounts for 15% of deaths and 24% of disability, suggesting that all efforts should be done to improve the management of major bleeding in DOAC-anticoagulated patients.
This study has several limitations. The most important is the small number of patients with major bleeding included; this makes it necessary to be very cautious in evaluating the recorded results. Furthermore, the time span for inclusion of cases was large and differences in patient management during this interval time can be expected. Obviously, the design of the study did not allow the collection of any data on the prevalence of bleedings and on the effect of different DOACs.
We believe this experience highlights the following needs: (1) homogeneous and more structured guidelines; (2) available reversal agents; (3) DOAC-specific measurements, rapidly available in emergency; (4) specific training on anticoagulation reversal for emergency department physicians; and (5) available consultants expert on thrombosis and haemostasis, who may ensure upgraded, homogeneous, and probably more effective management of acute major bleeding complications in anticoagulated patients.
List of participating centers and number of enrolled patients
Sophie Testa, Oriana Paoletti, Haemostasis and Thrombosis Center, Ospedale di Cremona (20).
Jan Beyer-Westendorf, Dresden University Clinic (15).
Maurizio Paciaroni, Stroke Unit, Università di Perugia (14).
Peter Verhamme, UZ Gasdthuisberg, Leuven (11).
Daniela Poli, Elisa Grifoni, Thrombosis Centre, AOU Careggi, Firenze (8).
Walter Ageno, Giovanna Colombo, Medicina I Osp di Circolo, Università dell’Insubria, Varese (7).
Vittorio Pengo, Cardiology Clinic, Thrombosis Centre, Department of Cardiac, Thoracic and Vascular Sciences, University of Padua (7).
Marc Righini, Division of Angiology and Hemostasis Genèva University Hospital (7).
Piera Sivera, Ospedale Mauriziano Torino (7).
Ponlapat Rojnuckarin, Chulalongkorn University, Bangkok (5).
Wang Tzu-Fei, The Ohio State University (5).
Giuliana Guazzaloca, Ludovica Migliaccio, Angiology Blood Coagulation, University Hospital Sant’Orsola Malpighi Bologna (5).
Bruno Caramelli, University of Sao Paulo (3).
Michela Provisione, Medicina II Ospedale Busto Arsizio, Varese (2).
Alberto Tosetto, S. Bortolo Hospital, Vicenza (1).
References
Ageno W, Gallus AS, Wittkowsky A, ACCP et al (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e44S–e88S
Connolly SJ, Ezekowitz MD, Yusuf S, RE-LY Steering Committee and Investigators et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361:1139–1151
Patel MR, Mahaffey KW, Garg J et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365:883–891
Granger CB, Alexander JH, McMurray JJ, ARISTOTLE Committees Investigators et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992
Giugliano RP, Ruff CT, Braunwald E, ENGAGE AF-TIMI 48 Investigators et al (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369:2093–2104
Ruff CT, Giugliano RP, Braunwald E et al (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383:955–962
Eriksson BI, Quinlan DJ, Weitz JI (2009) Comparative pharmacodynamics and pharmacokinetics of oral direct thrombin and factor xa inhibitors in development. Clin Pharmacokinet 48:1–22
Prisco D, Ageno W, Becattini C et al (2017) Italian intersociety consensus on DOAC use in internal medicine. Intern Emerg Med 1:387–406
Pengo V, Crippa L, Falanga A et al (2011) Questions and answers on the use of dabigatran and prospectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Center (FCSA). Thromb Haemost 106:868–876
Baglin T (2013) The role of the laboratory in treatment with new oral anticoagulants. J Thromb Haemost 11 (Suppl 1):122–128
Heidbuchel H, Verhamme P, Alings M et al (2015) Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 17:1467–1507
Kitchen S, Gray E, Mackie I, Baglin T et al (2014) Measurement of non-coumarin anticoagulants and their effects on test of haemostasis: guidance from the British Committee for Standards in Haematology. Br J Haematol 166:830–841
Tripodi A, Marongiu F, Moia M et al (2018) The vexed question of whether or not to measure levels of direct oralanticoagulants before surgery or invasive procedures. Intern Emerg Med. https://doi.org/10.1007/s11739-018-1854-6 (Epub ahead of print)
Beyer-Westendorf J, Förster K, Pannach S et al (2014) Rates, management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC registry. Blood 124:955–962
Pollack CV Jr, Reilly PA, Eikelboom J et al (2015) Idarucizumab for dabigatran reversal. N Engl J Med 373:511–520
Husted S, Verheugt FW, Comuth WJ (2016) Reversal strategies for NOACs: state of development, possible clinical applications and future perspectives. Drug Saf 39:5–13
Connolly SJ, Milling TJ Jr, Eikelboom JW, ANNEXA-4 Investigators et al (2016) Andexanet Alfa for acute major bleeding associated with factor Xa inhibitors. N Engl J Med 375:1131–1141
Ansell JE, Bakhru SH, Laulicht BE et al (2014) Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med 2014(371):2141–2142
Siegal DM, Cuker A (2014) Reversal of target-specific oral anticoagulants. Drug Discov Today 19:1465–1470
Antonucci E, Poli D, Tosetto A et al (2015) The Italian START-register on anticoagulation with focus on atrial fibrillation. PLoS One 10:e0124719
Testa S, Legnani C, Tripodi A et al (2016) Poor comparability of coagulation screening test with specific measurement in patients receiving direct oral anticoagulants: results from a multicenter/multiplatform study. J Thromb Haemost 14:2194–2201
Douxfils J, Mani H, Minet V et al (2015) Non-VKA oral anticoagulants: accurate measurement of plasma drug concentrations. Biomed Res Int 2015:345138
Schulman S, Kearon C (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3:692–694
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Marongiu F, Barcellona D (2018) Direct oral anticoagulants: what can we learn? Intern Emerg Med. https://doi.org/10.1007/s11739-018-1811-4 (Epub ahead of print)
Testa S, Legnani C, Pengo V et al (2015) Plasma levels of direct oral anticoagulants in real life patients with atrial fibrillation: results observed in four anticoagulation clinics. Tromb Res 137:178–183
Becattini C, Franco L, Beyer-Westendorf J et al (2017) Major bleeding with vitamin K antagonists or direct oral anticoagulants in real-life. Int J Cardiol 227:261–266
Veltkamp R, Rizos T, Horstmann S (2013) Intracerebral bleeding in patients on antithrombotic agents. Semin Thromb Hemost 39:963–971
Cucchiara B, Messe S, Sansing L et al (2008) Hematoma growth in oral anticoagulant related intracerebral hemorrhage. Stroke 39:2993–2996
Bauer KA (2015) Targeted anti-anticoagulants. N Engl J Med 373:569–571
Weitz JI, Eikelboom JW (2016) Urgent need to measure effects of direct oral anticoagulants. Circulation 134:186–188
Levy JH, Ageno W, Chan NC et al (2016) When and how to use antidotes for the reversal of direct oral anticoagulants: guidance from the SSC of the ISTH. J Thromb Haemost 14:623–627
Xu Y, Schulman S, Dowlatshahi D et al (2017) Direct oral anticoagulant- or warfarin-related major bleeding: characteristics, reversal strategies and outcomes from a multi-center observational study. Chest 152:81–91
Wilson D, Seiffge DJ, Traenka C et al (2017) Outcome of intracerebral hemorrhage associated with different oral anticoagulants. Neurology 88:1693–1700
Funding
The Arianna Anticoagulation Foundation supported the START Register and the study. The Foundation had no role in study design, collection, analysis, and interpretation of data, in writing the report, and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration, and its later amendments or comparable ethical standards.
Informed consent
All patients enrolled in the study have read and signed the informed consent.
Additional information
The study was promoted through the SSC Control of Anticoagulation of the International Society of Thrombosis and Haemostasis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Testa, S., Ageno, W., Antonucci, E. et al. Management of major bleeding and outcomes in patients treated with direct oral anticoagulants: results from the START-Event registry. Intern Emerg Med 13, 1051–1058 (2018). https://doi.org/10.1007/s11739-018-1877-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1877-z