Abstract
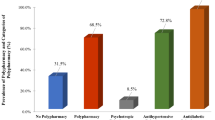
This study aimed at verifying the role of polypharmacy as an independent risk factor for adverse health outcomes in older emergency department (ED) patients. This was a large (n = 2057) sample of older ED patients (≥65 years) participating in an observational cohort study. Polypharmacy and excessive polypharmacy were defined as having 6–9 drug prescriptions and 10 or more drug prescriptions in the last 3 months, respectively. The total number of medication prescriptions was also available. Outcome measures were in-hospital mortality; 30-day ED return; ED revisit, hospital admission, and mortality at 6 months. Logistic and Cox regression models as well as receiver operating characteristic curves using the Youden index and the area under the curve were calculated. Polypharmacy and excessive polypharmacy were present in 624 (30.3 %) and 367 (17.8 %) subjects, respectively. The mean number of prescriptions in the last 3 months was 5.7 (range 0–25) drugs. Polypharmacy and, particularly, excessive polypharmacy were constantly and independently associated with worse outcomes. A cut-off of 6 had the highest value of the Youden Index in predicting the majority of the adverse outcomes considered. Polypharmacy and excessive polypharmacy are independent risk factors for adverse health outcomes after an ED visit. Further studies are needed to clarify whether drug related issues (such as non-compliance, inappropriate or suboptimal prescribing, adverse drug reactions, and drug–drug or drug–disease interactions) or underlying multimorbidity and disease severity, as well as clinical complexity and frailty, are responsible for the negative outcomes associated with polypharmacy.
Similar content being viewed by others
References
Salvi F, Morichi V, Grilli A et al (2007) Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Intern Emerg Med 2:292–301. doi:10.1007/s11739-007-0081-3
Caplan GA, Brown A, Croker WD, Dooland J (1998) Risk of admission within 4 weeks of discharge from the emergency department—the DEED study. Discharge of elderly from the emergency department. Age Ageing 27:697–702. doi:10.1093/ageing/27.6.697
Hastings SN, Schmader KE, Sloane RJ et al (2007) Adverse health outcomes after discharge from the emergency department—incidence and risk factors in a veteran population. J Gen Intern Med 22:1527–1531. doi:10.1007/s11606-007-0343-9
Hastings SN, Whitson HE, Purser JL et al (2009) Emergency department discharge diagnosis and adverse health outcomes in older adults. J Am Geriatr Soc 57:1856–1861. doi:10.1111/j.1532-5415.2009.02434.x
Hastings SN, Oddone EZ, Fillenbaum G et al (2008) Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care 46:771–777. doi:10.1097/MLR.0b013e3181791a2d
Hastings SN, Horney C, Landerman LR et al (2010) Exploring patterns of health service use in older emergency department patients. Acad Emerg Med 17:1086–1092. doi:10.1111/j.1553-2712.2010.00870.x
Hastings SN, Purser JL, Johnson KS et al (2008) Frailty predicts some but not all adverse outcomes in older adults discharged from the Emergency Department. J Am Geriatr Soc 56:1651–1657. doi:10.1111/j.1532-5415.2008.01840.x
Salvi F, Morichi V, Grilli A et al (2012) Screening for frailty in elderly emergency department patients by using the Identification of Seniors At Risk (ISAR). J Nutr Health Aging 16:313–318. doi:10.1007/s12603-011-0155-9
Hajjar ER, Cafiero AC, Hanlon JT (2007) Polypharmacy in elderly patients. Am J Geriatr Pharmacother 5:345–351. doi:10.1016/j.amjopharm.2007.12.002
Patterson SM, Hughes C, Kerse N et al (2012) Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 5:CD008165. doi:10.1002/14651858.CD008165.pub2
Meldon SW, Mion LC, Palmer RM et al (2003) A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department. Acad Emerg Med 10:224–232. doi:10.1197/aemj.10.3.224
Hastings SN, Schmader KE, Sloane RJ et al (2008) Quality of pharmacotherapy and outcomes for older veterans discharged from the emergency department. J Am Geriatr Soc 56:875–880. doi:10.1111/j.1532-5415.2008.01648.x
Shah BM, Hajjar ER (2012) Polypharmacy, adverse drug reactions, and geriatric syndromes. Clin Geriatr Med 28:173–186. doi:10.1016/j.cger.2012.01.002
Gnjidic D, Hilmer SN, Blyth FM et al (2012) Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 65:989–995. doi:10.1016/j.jclinepi.2012.02.018
Jyrkkä J, Enlund H, Korhonen MJ et al (2009) Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging 26:1039–1048. doi:10.2165/11319530-000000000-00000
Salvi F, Morichi V, Lorenzetti B et al (2012) Risk stratification of older patients in the emergency department: comparison between the Identification of Seniors At Risk and Triage Risk Screening Tool. Rejuv Res 15:288–294. doi:10.1089/rej.2011.1239
Salvi F, Morichi V, Grilli A et al (2008) A geriatric emergency service for acutely ill elderly patients: pattern of use and comparison with a conventional emergency department. J Am Geriatr Soc 56:2131–2138. doi:10.1111/j.1532-5415.2008.01991.x
Di Bari M, Salvi F, Roberts AT et al (2012) Prognostic stratification of elderly patients in the emergency department: a comparison between the “Identification of Seniors At Risk” and the “Silver Code”. J Gerontol A Biol Sci Med Sci 67:544–550. doi:10.1093/gerona/glr209
Di Bari M, Balzi D, Roberts AT et al (2010) Prognostic stratification of older persons based on simple administrative data: development and validation of the “Silver Code”, to be used in emergency department triage. J Gerontol A Biol Sci Med Sci 65:159–164. doi:10.1093/gerona/glp043
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF (2008) Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J 50:419e30. doi:10.1002/bimj.200710415
Chung MK, Bartfield JM (2002) Knowledge of prescription medications among elderly emergency department patients. Ann Emerg Med 39:605–608. doi:10.1067/mem.2002.122853
Banerjee A, Mbamalu D, Ebrahimi S et al (2011) The prevalence of polypharmacy in elderly attenders to an emergency department—a problem with a need for an effective solution. Int J Emerg Med 4:22. doi:10.1186/1865-1380-4-22
Rogers S, Wilson D, Wan S et al (2009) Medication-related admissions in older people: a cross-sectional, observational study. Drugs Aging 26:951–961. doi:10.2165/11316750-000000000-00000
Salvi F, Marchetti A, D’Angelo F et al (2012) Adverse drug events as cause of hospitalization in older adults. Drug Saf 35(Suppl. 1):29–45. doi:10.1007/BF03319101
Bouvy JC, De Bruin ML, Koopmanschap MA (2015) Epidemiology of adverse drug reactions in Europe: a review of recent observational studies. Drug Saf 38:437–453. doi:10.1007/s40264-015-0281-0
Budnitz DS, Pollock DA, Weidenbach KN et al (2006) National surveillance of emergency department visits for outpatient adverse drug events. JAMA 296:1858–1866. doi:10.1001/jama.296.15.1858
Budnitz DS, Lovegrove MC, Shehab N, Richards CL (2011) Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 365:2002–2012. doi:10.1056/NEJMsa1103053
Richardson K, Ananou A, Lafortune L et al (2011) Variation over time in the association between polypharmacy and mortality in the older population. Drugs Aging 28:547–560. doi:10.2165/11592000-000000000-00000
Nobili A, Licata G, Salerno F et al (2011) Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. Eur J Clin Pharmacol 67:507–519. doi:10.1007/s00228-010-0977-0
Díez-Manglano J, Giménez-López M, Carcés-Horna V et al (2015) Excessive polypharmacy and survival in polypathological patients. Eur J Clin Pharmacol 71:733–739. doi:10.1007/s00228-015-1837-8
Hilmer SN, Gnjidic D (2009) The effects of polypharmacy in older adults. Clin Pharmacol Ther 85:86–88. doi:10.1038/clpt.2008.224
Wierenga PC, Buurman BM, Parlevliet JL et al (2012) Association between acute geriatric syndromes and medication-related hospital admissions. Drugs Aging 29:691–699. doi:10.2165/11632510-000000000-00000
Gnjidic D, Hilmer SN, Blyth F et al (2012) High risk prescribing and incidence of frailty among older community-dwelling men. Clin Pharmacol Ther 91:521–528. doi:10.1038/clpt.2011.258
Pasina L, Djade CD, Tettamanti M et al (2014) Prevalence of potentially inappropriate medications and risk of adverse clinical outcome in a cohort of hospitalized elderly patients: results from the REPOSI Study. J Clin Pharm Ther 39:511–515. doi:10.1111/jcpt.12178
Fried TR, O’Leary J, Towle V et al (2014) Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc 62:2261–2272. doi:10.1111/jgs.13153
Morandi A, Bellelli G, Vasilevskis EE et al (2013) Predictors of rehospitalization among elderly patients admitted to a rehabilitation hospital: the role of polypharmacy, functional status, and length of stay. J Am Med Dir Assoc 14:761–767. doi:10.1016/j.jamda.2013.03.013
Sganga F, Landi F, Ruggiero C et al (2015) Polypharmacy and health outcomes among older adults discharged from hospital: results from the CRIME study. Geriatr Gerontol Int 15:141–146. doi:10.1111/ggi.12241
Cherubini A, Eusebi P, Dell’Aquila G et al (2012) Predictors of hospitalization in Italian nursing home residents: the ULISSE project. J Am Med Dir Assoc 13:84.e5–84.e10. doi:10.1016/j.jamda.2011.04.001
Payne RA, Abel GA, Avery AJ et al (2014) Is polypharmacy always hazardous? A restrospective cohort analysis using linked electronic health records from primary and secondary care. Br J Clin Pharmacol 77:1073–1082. doi:10.1111/bcp.12358
LaMantia MA, Platts-Mills TF, Biese K et al (2010) Predicting hospital admission and returns to the emergency department for elderly patients. Acad Emerg Med 17:252–259. doi:10.1111/j.1553-2712.2009.00675.x
Warburton RN, Parke B, Church W et al (2004) Identification of seniors at risk: process evaluation of a screening and referral program for patients aged > or =75 in a community hospital emergency department. Int J Health Care Qual Assur Inc Leadersh Health Serv 17:339–348. doi:10.1108/09526860410557598
Salvi F, Belluigi A, Cherubini A (2013) Predictive validity of different modified versions of the Identification of Seniors At Risk. J Am Geriatr Soc 61:462–464. doi:10.1111/jgs.12130
Mannucci PM, Nobili A, Investigators REPOSI (2014) Multimorbidity and polypharmacy in the elderly: lessons from REPOSI. Intern Emerg Med 9:723–734. doi:10.1007/s11739-014-1124-1
McCusker J, Cardin S, Bellavance F, Belzile E (2000) Return to the emergency department among elders: patterns and predictors. Acad Emerg Med 7:249–259. doi:10.1111/j.1553-2712.2000.tb01070.x
McCusker J, Bellavance F, Cardin S et al (2000) Prediction of hospital utilization among elderly patients during the 6 months after an emergency department visit. Ann Emerg Med 36:438–445. doi:10.1067/mem.2000.110822
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The study protocol was approved by the INRCA Ethics Committee (Ancona, Italy). Each participant gave Informed consent to participate to the study.
Rights and permissions
About this article
Cite this article
Salvi, F., Rossi, L., Lattanzio, F. et al. Is polypharmacy an independent risk factor for adverse outcomes after an emergency department visit?. Intern Emerg Med 12, 213–220 (2017). https://doi.org/10.1007/s11739-016-1451-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1451-5