Abstract
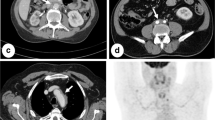
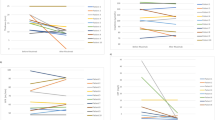
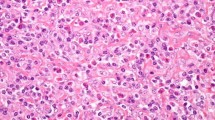
Idiopathic retroperitoneal fibrosis (IRF) is a rare disease characterized by fibro-inflammatory reaction surrounding ureters and other inner organs with possible secondary renal involvement. Symptoms are aspecific and recurrent phases of activity are generally associated with elevation of inflammatory indices. 18F-FDG-PET is nowadays an important tool for the detection of this disease, allowing differentiation between metabolically active tissue and fibrotic one. The purpose of this study was to investigate the role of 18F-FDG-PET in the management of IRF and to evaluate possible correlations between biochemical parameters and PET/CT findings of disease activity. We enrolled seven consecutive patients with IRF (in five histology proved the disease) observed from 2003 to 2012 (5 M:2 F, mean age 53.8 years, range 44–86 years). All patients presented with fever as first symptom; two had obstructive renal failure requiring hemodialysis; one underwent monolateral nephrectomy for parenchyma infiltration; six presented ureteral involvement; three underwent ureteral stent placement. For each patient, during a mean total follow-up of 26.5 months we evaluated serum creatinine, BUN, Hb, RBCs, WBCs, PLT, CRP, ESR. Periodic 18F-FDG-PET/CT scans (every 5.9 months—mean) were performed in all patients. Statistical evaluation was performed using “stepwise regression” analysis. Steroids and immunosuppressive agents induced a progressive normalization of PET/CT scans in all patients at the end of follow-up. Stepwise regression analysis showed that BUN, serum creatinine and CRP only if considered together, significantly correlated with SUV max (p value = 0.000003057). 18F-FDG-PET is a useful tool for clinical decision making in patient with IRF, allowing to evaluate the efficacy of the pharmacological treatment and to detect early recurrences, to modify the therapeutic approach. Acute phase reactants are not reliable alone for the management and the follow-up as they are often not concordant with metabolic assessment of the disease. In patients with ureteral involvement, CRP together with BUN and serum creatinine has a significant correlation with PET/CT results, and can help physicians in therapeutic approach, better than a single parameter.


Similar content being viewed by others
References
Vaglio A, Salvarani C, Buzio C (2006) Retroperitoneal fibrosis. Lancet 367:241–251
Marcolongo R, Tavolini IM, Lavender F et al (2004) Immunosuppressive therapy for idiopathic retroperitoneal fibrosis: a retrospective analysis of 26 cases. Am J Med 116:194–197
Yachoui R, Sehgal R, Carmichael B (2016) Idiopathic retroperitoneal fibrosis: clinicopathologic features and outcome analysis. Clin Rheumatol 35(2):401–407
Piccoli GB, Consiglio V, Arena V et al (2010) Positron emission tomography as a tool for the “tailored” management of retroperitoneal fibrosis: a nephro-urological experience. Nephrol Dial Transplant 25:2603–2610
Moroni G, Castellani M, Balzani A et al (2012) The value of 18F-FDG PET/CT in the assessment of active idiopathic retroperitoneal fibrosis. Eur J Nucl Med Mol Imaging 39:1635–1642
Ha YJ, Jung SJ, Lee KH, Lee SW, Lee SK, Park YB (2011) Retroperitoneal fibrosis in 27 Korean patients: single center experience. J Korean Med Sci 26:985–990
Nakajo M, Jinnouchi S, Fukukura Y et al (2007) The efficacy of whole-body FDG-PET or PET-CT for autoimmune pancreatitis and associated extrapancreatic autoimmune lesions. Eur J Nucl Med Mol Imaging 34:2088–2095
Wold S, Sjöström M, Eriksson L et al (2001) PLS-regression: a basic tool of chemometrics, Chemometrics and Intelligent Laboratory Systems 58(2):109–130, ISSN 0169-7439
Vaglio A, Maritati F (2016) J Am Soc Nephrol [Epub ahead of print]
Zhou HJ, Yan Y, Zhou B et al. (2015) Retroperitoneal fibrosis: a retrospective clinical data analysis of 30 patients in a 10-year period. Chin Med J (Engl) 20; 128(6):804–10
Labidi J, Ariba YB, Chargui S et al (2015) Retroperitoneal fibrosis: a retrospective review of clinical presentation, treatment and outcomes. Saudi J Kidney Dis Tranpl 26(4):816–822
Surcel C, Mirvald C, Pavelescu P et al (2015) Management of idiopathic fibrosis from the urologist’s perspective. Ther Adv Urol 7(2):85–99
Baker LR, Mallinson WJ, Gregory MC et al (1987) Idiopathic retroperitoneal fibrosis. A retrospective analysis of 60 cases. Br J Urol 60:497–503
Corradi D, Maestri R, Palmisano A et al (2007) Idiopathic retroperitoneal fibrosis: clinicopathologic features and differential diagnosis. Kidney Int 72(6):742–753
Koep L, Zuidema GD (1977) The clinical significance of retroperitoneal fibrosis. Surgery 81(3):250–257
Wagenknecht LV, Auvert J (1971) Symptoms and diagnosis of retroperitoneal fibrosis: analysis of 31 cases. Urol Int 26(3):185–195
Pipitone N, Vaglio A, Salvarani C (2012) Retroperitoneal fibrosis. Best Pract Res Clin Rheumatol 26:439–448
Pelkmans LG, Aarnoudse AJLH, Hendriksz TR, van Bommel EFH (2012) Value of acute-phase reactants in monitoring disease activity and treatment response in idiopathic retroperitoneal fibrosis. Nephrol Dial Transplant 27:2819–2825
Van Bommel EF, Jansen I, Hendriksz TR, Aarnoudse AL (2009) Idiopathic retroperitoneal fibrosis: prospective evaluation of incidence and clinicoradiologic presentation. Med (Baltimore) 88(4):193–201
Pipitone N, Versari A, Salvarani C (2008) Role of imaging studies in the diagnosis’ and the follow-up of large-vessel vasculitis: an update. Rheumatology 47:403–408
Salvarani C, Pipitone N, Versari A et al (2005) Positron emission tomography (PET): evaluation of chronic periaortitis. Arthritis Rheum 53:298–303
Vaglio A, Greco P, Versari A et al (2005) Post-treatment residual tissue in idiopathic retroperitoneal fibrosis: active residual disease or silent scar? A study using 18F-FDG-PET. Clin Exp Rheumatol 23:231–234
Van Bommel EF (2002) Retroperitoneal fibrosis. Neth J Med 60:231–242
Jansen I, Hendriksz TR, Han SH, Huiskes AW, van Bommel EF. (2010) 18F-fluorodeoxyglucose position emission tomography (FDG-PET) for monitoring disease activity and treatment response in idiopathic retroperitoneal fibrosis. Eur J Intern Med 21(3):216–21
Warnatz K, Keskin AG, Uhl M et al (2005) Immunosuppressive treatment of chronic periaortitis: a retrospective study of 20 patients with chronic periaortitis and a review of the literature. Ann Rheum Dis 64:828–833
Vaglio A, Palmisano A, Alberici F (2011) Prednisone versus tamoxifen in patients with idiopathic retroperitoneal fibrosis: an open-label randomised controller trial. Lancet 378(9788):338–46
Van Bommel EF, Pelkmans LG, van Damme H et al (2013) Long-term safety and efficacy of a tamoxifen-based treatment strategy for idiopathic retroperitoneal fibrosis. Eur J Intern Med jul 24(5):444–450
Acknowledgments
The authors thank for the statistical analysis Prof. Maurizio Maravalle, Department of Information Engineering, Computer Science and Mathematics, University of L'Aquila, 67100 Coppito (AQ), Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of retrospective study formal consent is not required.
Rights and permissions
About this article
Cite this article
Fofi, C., Prosperi, D., Pettorini, L. et al. Diagnosis and follow-up of idiopathic retroperitoneal fibrosis: role of 18F-FDG-PET/CT and biochemical parameters in patients with renal involvement. Intern Emerg Med 11, 809–816 (2016). https://doi.org/10.1007/s11739-016-1426-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1426-6