Abstract
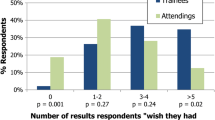
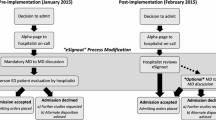
Transfers of care have been associated with adverse events. High quality sign-out may help mitigate this risk. The authors sought to characterize the clinical questions asked of physicians covering patients overnight and to determine the adequacy of current sign-out practice to anticipate inquiries. The authors conducted a prospective, self-report study of interns’ overnight experience at two hospitals. We collected data from novice interns (July 7–August 3, 2010) and experienced interns (March 2–March 29, 2011) in an Internal Medicine residency program. Interns recorded information about overnight inquiries regarding cross-covered patients. For each inquiry about a patient, the intern was asked to record what the situation was about, who initiated the contact, where the intern found the desired information, whether all required data was located, whether the call could have been anticipated by the primary team, if so, whether the call was anticipated, whether the sign-out was sufficient, the time required to address the question, and whether the patient was physically visited. Twenty-one interns (13 novice, 8 experienced) reported 167 overnight inquiries. Most were from nursing staff (87 %) about a wide range of topics, with orders (25 %) and plan of care (20 %) being most common. Trainees used the oral or written sign-out to answer 56 % of inquiries. The proportion of inquiries successfully anticipated (47 % overall) significantly decreased as the academic year progressed (AOR = 0.4, 95 % CI 0.2, 0.8). Trainees rely on sign-out to answer nearly half of overnight inquiries, but the quality of sign-out may decrease over the course of the academic year. The deterioration of sign-out quality from novice to experienced interns and the common use of sign-out as a reference by covering interns suggest continued education, support and oversight by supervising physicians may be beneficial.

Similar content being viewed by others
References
Horwitz LI, Krumholz HM, Green ML, Huot SJ (2006) Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med 166(11):1173–1177
Okie S (2007) An elusive balance—residents’ work hours and the continuity of care. N Engl J Med 356(26):2665–2667. doi:10.1056/NEJMp078085
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH (1994) Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med 121(11):866–872
Schuberth JL, Elasy TA, Butler J, Greevy R, Speroff T, Dittus RS, Roumie CL (2008) Effect of short call admission on length of stay and quality of care for acute decompensated heart failure. Circulation 117(20):2637–2644
Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS (2005) Residents report on adverse events and their causes. Arch Intern Med 165(22):2607–2613. doi:10.1001/archinte.165.22.2607
Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH (2008) Consequences of inadequate sign-out for patient care. Arch Intern Med 168(16):1755–1760
Accreditation Committee for Graduate Medical Education (2011) Common Program Requirements
Arora V, Kao J, Lovinger D, Seiden SC, Meltzer D (2007) Medication discrepancies in resident sign-outs and their potential to harm. J Gen Intern Med 22(12):1751–1755
Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM (2008) Adequacy of information transferred at resident sign-out (in-hospital handover of care): a prospective survey. Qual Saf Health Care 17(1):6–10
Anderson J, Shroff D, Curtis A, Eldridge N, Cannon K, Karnani R, Abrams T, Kaboli P (2010) The Veterans Affairs shift change physician-to-physician handoff project. Jt Comm J Qual Patient Saf 36(2):62–71
Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO (2005) Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 14(6):401–407. doi:10.1136/qshc.2005.015107
Arora VM, Johnson JK, Meltzer DO, Humphrey HJ (2008) A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care 17(1):11–14
DeRienzo CM, Frush K, Barfield ME, Gopwani PR, Griffith BC, Jiang X, Mehta AI, Papavassiliou P, Rialon KL, Stephany AM, Zhang T, Andolsek KM (2012) Handoffs in the era of duty hours reform: a focused review and strategy to address changes in the Accreditation Council for Graduate Medical Education Common Program Requirements. Acad Med 87(4):403–410. doi:10.1097/ACM.0b013e318248e5c2
Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM (2006) Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med 1(4):257–266
Wohlauer MV, Arora VM, Horwitz LI, Bass EJ, Mahar SE, Philibert I (2012) The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med 87(4):411–418. doi:10.1097/ACM.0b013e318248e766
Epley N, Keysar B, Van Boven L, Gilovich T (2004) Perspective taking as egocentric anchoring and adjustment. J Pers Soc Psychol 87(3):327–339. doi:10.1037/0022-3514.87.3.327
Solet DJ, Norvell JM, Rutan GH, Frankel RM (2005) Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med 80(12):1094–1099
Horwitz LI, Moin T, Green ML (2007) Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med 22(10):1470–1474
Horwitz LI, Schuster KM, Thung SF, Hersh DC, Fisher RL, Shah N, Cushing W, Nunes J, Silverman DG, Jenq GY (2012) An institution-wide handoff task force to standardise and improve physician handoffs. BMJ Qual Saf. doi:10.1136/bmjqs-2011-000658
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379. doi:10.1016/s0895-4356(96)00236-3
Chang VY, Arora VM, Lev-Ari S, D’Arcy M, Keysar B (2010) Interns overestimate the effectiveness of their hand-off communication. Pediatrics 125(3):491–496
Bump GM, Jovin F, Destefano L, Kirlin A, Moul A, Murray K, Simak D, Elnicki DM (2011) Resident sign-out and patient hand-offs: opportunities for improvement. Teach Learn Med 23(2):105–111. doi:10.1080/10401334.2011.561190
Helms AS, Perez TE, Baltz J, Donowitz G, Hoke G, Bass EJ, Plews-Ogan ML (2012) Use of an appreciative inquiry approach to improve resident sign-out in an era of multiple shift changes. J Gen Intern Med 27(3):287–291. doi:10.1007/s11606-011-1885-4
Acknowledgments
Dr. Horwitz is supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. Dr. Horwitz is also a Pepper Scholar with support from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG021342 NIH/NIA).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fogerty, R.L., Rizzo, T.M. & Horwitz, L.I. Assessment of internal medicine trainee sign-out quality and utilization habits. Intern Emerg Med 9, 529–535 (2014). https://doi.org/10.1007/s11739-013-0971-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-013-0971-5