Abstract
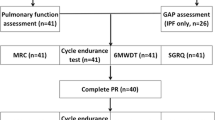
The role of pulmonary rehabilitation (PR) in COPD patients with lung hyperinflation has not yet been fully investigated. We retrospectively evaluated the effect of a standard PR course on exercise tolerance and symptoms according to the presence or absence of associated lung hyperinflation, as defined by lung function parameters in three Italian rehabilitation centres. In a cohort of 823 COPD patients (age 71 ± 8 years, FEV1 56 ± 18% pred.) we have systematically recorded: changes (∆) in 6-minute walking test (6MWD) as the primary outcome; dyspnoea (D); muscle fatigue (F); SO2nadir during effort; perceived breathlessness score (MRC); and specific health-related quality of life (SGRQ). Outcomes were compared between patients with lung hyperinflation (n = 283, LH) or without (n = 540 No-LH). Groups were comparable for age, body mass index, baseline exercise tolerance, and breathlessness. ∆-6MWD (+72 ± 47 vs. +62 ± 42 m, p < 0.05); ∆-D (−2.3 ± 1.7 vs. −1.9 ± 1.3 point, p < 0.05) and ∆-SO2nadir (+1.4 ± 3.0 and +0.5 ± 3.3 point, p < 0.05) were greater in LH than in No-LH. Using a multivariate linear regression model, ∆-6MWD in the LH group significantly correlated with lower functional residual capacity (p = 0.021) and baseline 6MWD (p = 0.004). Tolerance, gas exchange and perceived symptoms during effort are the parameters that gain a significant benefit from standard rehabilitation in COPD patients with a lung hyperinflation condition.


Similar content being viewed by others
Abbreviations
- Δ:
-
Pre-to-post changes in rehabilitation outcomes
- 6MWD:
-
6-Minute walking distance
- BMI:
-
Body mass index
- BODE:
-
Global functional index obtained by measure of BMI, FEV1, MRC and 6MWD
- COPD:
-
Chronic obstructive pulmonary disease
- D:
-
Borg dyspnoea
- SD:
-
Standard deviation
- LH:
-
COPD patients with associated lung hyperinflation
- F:
-
Borg muscle fatigue
- FEV1/FVC:
-
Forced expiratory volume in the first second on forced vital capacity ratio
- FEV1 :
-
Forced expiratory volume in the first second
- FiO2 :
-
Inspiratory fraction of oxygen
- FRC:
-
Functional residual capacity
- FVC:
-
Forced vital capacity
- GOLD:
-
Global initiative for chronic obstructive lung disease
- HRQL:
-
Health-related quality of life
- LTOT:
-
Long-term oxygen therapy
- LVRS:
-
Lung volume reduction surgery
- MCID:
-
Minimal clinically important difference
- MRC:
-
Medical Research Council dyspnoea scale
- NETT:
-
National Emphysema Treatment Trial
- No-LH:
-
Patients without a lung hyperinflation
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PaO2/FiO2 :
-
Arterial pressure on specific oxygen flow
- PaO2 :
-
Arterial partial pressure of oxygen
- PR:
-
Pulmonary rehabilitation
- RV/TLC:
-
Residue volume on total lung capacity ratio
- RV:
-
Residual volume
- SGRQ:
-
St. George’s respiratory questionnaire on perceived quality of life
- SO2nadir:
-
Minimum value of pulse oxygen saturation recorded during 6MWD
- TLC:
-
Total lung capacity
References
Global Initiative for Chronic Obstructive Pulmonary Disease (2006) Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: NHLBI/WHO workshop report, NIH Publication 2701. http://www.goldcopd.com (last accessed March 2011)
Burrows B, Fletcher CM, Heard BE, Jones NL, Wootliff JS (1966) The emphysematous and bronchial types of chronic airways obstruction. A clinicopathological study of patients in London and Chicago. Lancet 1:830–835
Pistolesi M, Camiciottoli G, Paoletti M, Marmai C, Lavorini F, Meoni E, Marchesi C, Giuntini C (2008) Identification of a predominant COPD phenotype in clinical practice. Respir Med 102:367–376
Cerveri I, Dore R, Corsico A, Zoia MC, Pellegrino R, Brusasco V, Pozzi E (2004) Assessment of emphysema in COPD: a functional and radiologic study. Chest 125:1714–1718
Casaburi R, ZuWallack R (2009) Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med 360:1329–1335
Pitta F, Troosters T, Probst VS, Langer D, Decramer M, Gosselink R (2008) Are patients with COPD more active after pulmonary rehabilitation? Chest 134:273–280
Crisafulli E, Gorgone P, Vagaggini B, Pagani M, Rossi G, Costa F, Guarriello V, Paggiaro P, Chetta A, de Blasio F, Olivieri D, Fabbri LM, Clini EM (2010) Efficacy of standard rehabilitation in COPD outpatients with comorbidities. Eur Respir J36:1042–1048
Clini EM, Crisafulli E, Costi S, Rossi G, Lorenzi C, Fabbri LM, Ambrosino N (2009) Effects of early inpatient rehabilitation after acute exacerbation of COPD. Respir Med 103:1526–1531
Ries AL, Make BJ, Lee SM, Krasna MJ, Bartels M, Crouch R, Fishman AP, National Emphysema Treatment Trial Research Group (2005) The effects of pulmonary rehabilitation in the national emphysema treatment trial. Chest 128:3799–3809
(2006) American Thoracic Society/European Respiratory Society Statement On Pulmonary Rehabilitation. Am J Respir Crit Care Med 173:1390–1413
Clini E, Costi S, Romagnoli M, Florini F (2004) Rehabilitation of COPD patients: which training modality. Monaldi Arch Chest Dis 61:167–173
Charlson M, Szatrowski TP, Peterson J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Quanjer PH (1983) Working party on “Standardization of lung function test”. Bull Eur Physiopathol Respir 19(Suppl 5):7–10
American Thoracic Society (2002) American Thoracic Society statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117
Borg G (1982) Psychophysical basis of perceived exertion. Med Sci Sports Exerc 14:31–37
Fletcher CM (1960) Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the aetiology of chronic bronchitis (MRC breathlessness score). Br Med J 2:1665
Carone M, Bertolotti G, Anchisi F, Zotti AM (1999) The St George’s respiratory questionnaire (SGRQ): Italian version. Rassegnadi Patologiadell’ Apparato Respiratorio 14:31–37
Make B, Casaburi R, Kline Leidy N (2005) Interpreting results from clinical trials: understanding minimal clinically important differences in COPD outcome. COPD 2:1–5
Redelmeier DA, Bayoumi AM, Goldstein RS, Guyatt GH (1997) Interpreting small differences in functional status: the six-minute walk test in chronic lung disease patients. Am J Respir Crit Care Med 155:1278–1282
DeTorres JP, Pinto-Plata V, Ingenito E, Bagley P, Gray A, Berger R, Celli B (2002) Power of outcome measurements to detect clinically significant changes in pulmonary rehabilitation of patients with COPD. Chest 121:1092–1098
Giustino G, Webb KA, Sutherland KB, O’Donnell DE (1999) Severe exertional dyspnea in a patient with localized emphysema. Can Respir J 6:535–539
Boschetto P, Miniati M, Miotto D, Braccioni F, De Rosa E, Bononi I, Papi A, Saetta M, Fabbri LM, Mapp CE (2003) Predominant emphysema phenotype in chronic obstructive pulmonary disease patients. Eur Respir J 21:450–454
Burrows B, Bloom JW, Traver GA, Cline MG (1987) The course and prognosis of different forms of chronic airways obstruction in a sample from the general population. N Engl J Med 317:1309–1314
Burrows B, Earle RH (1969) Prediction of survival in patients with chronic airways obstruction. Am Rev Respir Dis 99:865–871
Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR (2004) The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J 23:28–33
Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto-Plata V, Cabral HJ (2004) The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 350:1005–1012
Martinez FJ, Foster G, Curtis JL, Criner G, Weinmann G, Fishman A, DeCamp MM, Benditt J, Sciurba F, Make B, Mohsenifar Z, Diaz P, Hoffman E, Wise R, Research Group NETT (2006) Predictors of mortality in patients with emphysema and severe airflow obstruction. Am J Respir Crit Care Med 173:1326–1334
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, Fabbri LM, Goldin JG, Jones PW, Macnee W, Make BJ, Rabe KF, Rennard SI, Sciurba FC, Silverman EK, Vestbo J, Washko GR, Wouters EF, Martinez FJ (2010) Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med 182:598–604
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crisafulli, E., Venturelli, E., Biscione, G. et al. Exercise performance after standard rehabilitation in COPD patients with lung hyperinflation. Intern Emerg Med 9, 23–31 (2014). https://doi.org/10.1007/s11739-011-0727-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0727-z