Abstract
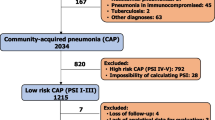
The objective was to compare three score systems, pneumonia severity index (PSI), the Confusion-Urea-Respiratory Rate-Blood pressure-65 (CURB-65), and severe community-acquired pneumonia (SCAP), for prediction of the outcomes in a cohort of patients with community-acquired (CAP) and healthcare-associated pneumonia (HCAP). Large multi-center, prospective, observational study was conducted in 55 hospitals. HCAP patients were included in the high classes of CURB-65, PSI and SCAP scores have a mortality rate higher than that of CAP patients. HCAP patients included in the low class of the three severity rules have a significantly higher incidence of adverse events, including development of septic shock, transfer into an ICU, and death (p < 0.01). At multivariate Cox regression analysis, inclusion in the severe classes of PSI, CURB-65, or SCAP scores and receipt of an empirical therapy not adherent to international guidelines prove to be risk factors independently associated with poor outcome. PSI, CURB-65, and SCAP score have a good performance in patients with CAP but are less useful in patients with HCAP, especially in patients classified in the low-risk classes.
Similar content being viewed by others
References
Venditti M, Falcone M, Corrao S et al (2009) Comparison of the outcomes of patients hospitalized with community-acquired, health care-associated, and hospital-acquired pneumonia. Ann Intern Med 150:19–26
Zilberberg MD, Shorr AF, Micek ST et al (2008) Antimicrobial therapy escalation and hospital mortality among patients with health-care-associated pneumonia: a single-center experience. Chest 134:963–968
Shorr AF, Zilberberg MD, Micek ST, Kollef MH (2008) Prediction of infection due to antibiotic-resistant bacteria by select risk factors for health care-associated pneumonia. Arch Intern Med 168:2205–2210
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336:243–250
Lim WS, van der Eerden MM, Laing R et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58:377–382
Espana PP, Capelastegui A, Gorordo I et al (2006) Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med 174:1249–1256
Shindo Y, Sato S, Maruyama E et al (2008) Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia. Respirology 13:731–735
Mandell LA, Wunderink RG, Anzueto A et al (2007) Infectious Diseases Society of America. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72
American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Micek ST, Kollef KE, Reichley RM et al (2007) Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother 51:3568–3573
Shindo Y, Sato S, Maruyama E et al (2009) Health-care-associated pneumonia among hospitalized patients in a Japanese community hospital. Chest 135:633–640
Falcone M, Venditti M, Corrao S, Serra P for the SIMI (2011) Role of multidrug-resistant pathogens in health care-associated pneumonia. Lancet Infect Dis 11:12–13
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Italian Society of Internal Medicine (SIMI).
An erratum to this article can be found at http://dx.doi.org/10.1007/s11739-011-0734-0
Appendix: Participating Members of the Italian Society of Internal Medicine
Appendix: Participating Members of the Italian Society of Internal Medicine
Medicina Interna, Policlinico San Donato Milanese: Francesco Salerno.
Policlinico Umberto I—Università di Roma “La Sapienza”: Sebastiano Filetti, Emilio D’Erasmo, Filippo Rossi Fanelli. Geriatria, Ospedale Civile, Montefiascone: Alessandra Fiorentini, Luigi Cricco.
Medicina Interna 5, Azienda Ospedaliera San Camillo-Forlanini, Roma: Laura Gasbarrone, Cecilia Serafini.
Clinica Medicina Interna 3, Azienda Ospedaliera Universitaria San Martino, Genova: Riccardo Ghio, Gabriele Zoppoli.
Medicina Generale III, Ospedale Luigi Sacco, Milano: Michele Cortellaro, Marina Magenta.
Medicina Generale I, Azienda Ospedaliera Universita degli Studi di Siena: Ranuccio Nuti, Roberto Valenti.
Presidio Ospedaliero C. Ondoli, Angera: Vincenzo Milano.
Medicina Interna, Azienda Ospedaliera San Giovanni Addolorata, Roma: Camillo Brandimarte, Paolo Carfagna.
Divisione Medicina Interna e Specialistica, Policlinico Universitario, Palermo: Riccardo Di Sciacca, Antonino Tuttolomondo.
Unità Operativa Medicina, Azienda Ospedaliera Card. G. Panico, Tricase: Maria Grazia Serra.
Semeiotica Medica, Policlinico S. Orsola Malpighi, Bologna: Mauro Bernardi, Silvia Li Bassi.
Dipartimento Medicina Interna e Gastroenterologia, Policlinico S. Orsola Malpighi, Bologna: Vincenzo Stanghellini, Elena Boschi.
Medicina Interna Universitaria “Cesare Frugoni”, Policlinico, Bari: Salvatore Antonaci, Francesco Vella.
Dipartimento di Medicina Interna—Policlinico Universitario “G. Martino” di Messina: Antonino Catalano.
Divisione Medicina, Azienda Ospedaliera Universitaria, Modena: Maria Luisa Zeneroli, Elisabetta Ascari, Alberto Veggetti.
Ospedale Del Delta, Lagosanto: Roberto Manfredini, Susanna Gamberoni.
Istituto di Clinica Medica Generale, Ospedale di Cattinara, Trieste: Gianfranco Guarnieri, Angela Fioretto.
Medicina Interna, Ospedale “G. Mazzini” ASL Teramo: Dario Di Michele, Domenico Parisi.
Divisione di Medicina Interna, Ospedale Civile, Casorate Primo: Nicola Lucio Liberato, Esio Ronchi.
Medicina Interna, Ospedale Civile, Senigallia: Simonetta Sturbini, Paolo Canafoglia.
Medicina Interna Ospedaliera, Azienda Ospedaliera Universitaria Sant’Anna, Ferrara: Massimo Gallerani, Benedetta Boari.
Medicina ad Alta Rotazione, Azienda Ospedaliera Universitaria Sant’Anna, Ferrara: Ingrid Nielsen.
Geriatria, Azienda Ospedaliera San Gerardo, Monza: Giorgio Annoni, Anna Rossetti.
Azienda Ospedaliera Ospedale di Circolo Fondazione Macchi, Varese: Matteo Bernasconi.
Medicina Interna, Azienda Ospedaliera Policlinico Bari: Carmela Giannatempo.
Medicina I, Azienda Ospedaliera G. Salvini, Garbagnate Milanese: Roberta Turconi, Maurizio Colombo.
Medicina Interna 2, Policlinico Ospedale Maggiore, Milano: Alberto Tedeschi, Raffaella Rossi.
Medicina Interna II, Policlinico S. Maria alle Scotte, Siena: Roberto Cappelli, Valentina Guidi.
Medicina 1 A.S.L. 2 Savonese Ospedale San Paolo Savona: Rodolfo Tassara, D. De Melis.
Medicina Interna, Fondazione IRCCS Ospedale Maggiore Policlinico, Mangiagalli e Regina Elena, Milano: Roberto Cosentini, Margherita Arioli, Francesco Salerno, Giulia Gobbo.
Medicina Generale, A.S.L. 17, Ospedale di Este: Fabio Presotto, Sergio Gallana.
Clinica Medica III, Fondazione IRCCS Policlinico San Matteo-Università di Pavia: Carlo Balduini, Giampiero Bertolino.
Medicina Interna, Presidio Ospedaliero—A.S.L. BA/5, Monopoli-Conversano: Giacomo Fera.
Clinica Medica I, Policlinico San Matteo, Pavia: Gino Roberto Corazza, Ida Capriglione.
Medicina, Presidio Sanitario Gradenigo, Torino: Giulia Pilerio.
Dipartimento di Medicina Interna—Fondazione IRCCS Ospedale Maggiore Policlinico, Mangiagalli e Regina Elena & Università degli studi di Milano: Maria Domenica Cappellini, Giovanna Fabio, Maria Carrabba.
Medicina Generale, Ospedale E. Bassini, Cinisello Balsamo, Azienda Ospedaliera S.Gerardo–Monza: Sheng Chin Wu, Maria Beatrice Secchi.
Medicina, Casa di Cura La Madonnina, Bari: Michele Leone.
Medicina Interna, Presidio Ospedaliero, Pescara: Lucrezia De Feudis.
Medicina Interna Ospedale San Salvatore Pesaro: Massimo Gunelli, Orazio Ferri.
Medicina Interna 2, Presidio Ospedaliero Cà Fondello, Treviso: Carlo Doroldi, Roberta Pistis.
Università Vita-Salute San Raffaele–Milano: Maria Grazia Sabbadini, Moreno Tresoldi.
Medicina Interna 5, Ospedale Unico della Versilia, Lido di Camaiore: Paola Lambelet, Stefano Fascetti.
Struttura Complessa di Medicina Interna, A.O. Ospedale di Lecco, P.O. di Merate: Massimo Vanoli, Gianluca Casella.
Clinica Medica Generale, Azienda Ospedali Civili, Brescia: Enrico Agabiti Rosei, Andrea Salvi.
Medicina Interna, Ospedale Civile dell’Annunziata, Cosenza: Alfonso Noto.
Medicina Interna, Ospedale San Giovanni Decollato-Andosilla, Civita Castellana: Antonio Perciaccante.
Medicina Interna, Ospedale Madre G. Vannini, Roma: Claudio Santini, Maurizia Galiè.
Istituto di Medicina Interna e Geriatria, Università Cattolica del Sacro Cuore, Policlinico A. Gemelli, Roma: Giovanni Gasbarrini, Antonio Grieco.
Medicina 1, Azienda Ospedaliera di Busto Arsizio (VA) Ospedale di Circolo di Busto Arsizio: Barbara Nardi.
Clinica Medica 1, Azienda Ospedaliera, Padova: Aldo Gaetano Baritussio, Roberto Vannuccini.
Medicina Generale, Alessandria: Mauro Cappelletti.
Medicina d’Urgenza e Pronto Soccorso, Università Cattolica del Sacro Cuore, Policlinico A. Gemelli, Roma: Nicolò Gentiloni-Silveri.
Medicina Interna C, Policlinico G.B. Rossi, Verona: Alessandro Lechi, Germana Montesi.
Rights and permissions
About this article
Cite this article
Falcone, M., Corrao, S., Venditti, M. et al. Performance of PSI, CURB-65, and SCAP scores in predicting the outcome of patients with community-acquired and healthcare-associated pneumonia. Intern Emerg Med 6, 431–436 (2011). https://doi.org/10.1007/s11739-011-0521-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0521-y