Abstract
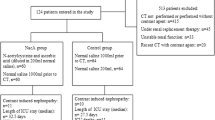
Contrast-induced nephropathy (CIN) is most commonly defined as acute renal failure occurring within 48–72 h of exposure to an intravascular radiographic contrast medium that is not attributable to other causes. In the international literature, a 25% increase in serum creatinine levels or an increase in absolute values of 0.5 mg/dl from baseline has been suggested to define CIN. The reported incidence of CIN varies widely, ranging from 2 to 50%. This variability results from differences in the presence or absence of risk factors. With a retrospective analysis we evaluated the use of saline hydration plus N-acetyl cysteine (NAC) to prevent CIN in a low-risk population of patients undergoing coronary artery angiography compared with an historic low risk group not treated. From January 2009 to December 2009, 152 consecutive patients who underwent coronary artery angiography with a low osmolarity contrast agent were enrolled in our study, and compared with an historic control group consisting of 172 low-risk patients. Nephrotoxic drugs such as diuretics, ACE-I and ARBs were stopped at least 24 h before the procedure. Inclusion criteria to define low-risk population were the absence of: diabetes, age >65 years, or baseline creatinine >1.4 mg/dl. We have treated group A (152 patients, 47.3%) with a saline hydration (1 ml/kg/h) plus N-acetyl cysteine 600 mg 12 h before and 12 h after the procedure; group B (group control of 170 patients, 52.7%) were not treated. The overall incidence of CIN was 7.1% (23 patients). In particular, the incidence of CIN was 2.6% (4 patients) in the group A and 11.2% (19 patients) in the group B (p = 0.002). In the multivariate analysis, including risk factor such as age, hypertension, hypercholesterolemia, current smoking habit baseline creatinine level, contrast index and hydration, the last variable was the only one inversely correlated independently with the incidence of CIN (p = 0.001). In conclusion, intravenous hydration with saline and NAC is an effective and low cost tool in preventing CIN in patients undergoing coronary artery angiography, and, according to the current guidelines, should be used in all high-risk patients for CIN. Our results show that even in patients at low risk, hydration with saline 0.9% plus NAC is useful and significantly reduces the incidence of CIN.



Similar content being viewed by others
References
Levy EM, Viscoli CM, Horwitz RI (1996) The effect of acute renal failure on mortality: a cohort analysis. JAMA 275(19):1489–1494
Dangas G, Iakovou I, Nikolsky E et al (2005) Contrastinduced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol 95(1):13–19
Mehran R, Aymong ED, Nikolsky E et al (2004) A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 44(7):1393–1399
McCullough PA (2008) Contrast-induced acute kidney injury. J Am Coll Cardiol 51(15):1419–1428
Gutierrez N, Diaz A, Timmis GC (2002) Determinants of serum creatinine trajectory in acute contrast nephropathy. J Intervent Cardiol 15:349–354
Rihal CS, Textor SC, Grill DE et al (2002) Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation 105:2259–2264
Iakovou I, Dangas G, Mehran R et al (2003) Impact of gender on the incidence and outcome of contrast-induced nephropathy after percutaneous coronary intervention. J Invasive Cardiol 15:18–22
Sanaei-Ardekani M, Movahed MR, Movafagh S, Ghahramani N (2005) Contrast-induced nephropathy: a review. Cardiovasc Revasc Med 6:82–88
Weisbord SD, Mor MK, Resnick AL et al (2008) Prevention, incidence, and outcomes of contrast-induced acute kidney injury. Arch Intern Med 168:1325–1332
Briguori C, Airoldi F, D’Andrea D et al (2007) Renal insufficiency following contrast media administration trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation 115:1211–1217
Recio-Mayoral A, Chaparro M, Prado B et al (2007) The reno-protective effect of hydration with sodium bicarbonate plus N-acetyl cysteine in patients undergoing emergency percutaneous coronary intervention. J Am Coll Cardiol 49(12):1283–1288
Solomon R, Deray G (2006) How to prevent contrast-induced nephropathy and manage risk patients: practical recommendations. Kidney Int 69:S51–S53
Calabrò P, Bianchi R, Caprile M et al (2010) Use of NaCl saline hydration and N-acetyl cysteine to prevent contrast induced nephropathy in different populations of patients at high and low risk undergoing coronary artery angiography. Minerva Cardioangiol 58(1):35–40
Mueller C, Buerkle G, Buettner HJ et al (2002) Prevention of contrast media-associated nephropathy: randomized comparison of 2 hydration regimens in 1620 patients undergoing coronary angioplasty. Arch Intern Med 162:329–336
Mehran R, Aymong ED, Nikolsky E et al (2004) A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention. J Am Coll Cardiol 44:1393–1399
Cigarroa RG, Lange RA, Williams RH, Hillis LD (1989) Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med 86:649–652
Levey AS, Coresh J, Balk E et al (2002) Clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(Suppl 1):S1–S246
McCullough A, Adam A, Becker CR et al (2006) Contrast-induced nephropathy: clinical insights and practical guidance. A report from the CIN consensus working panel. Am J Cardiol 98(Suppl):1K–77K
Mueller C, Burkle G, Buettner HS et al (2002) Prevention of contrast media associated nephropathy. Randomized comparison of 2 hydratation regimens in 1620 patients undergoing coronary angioplasty. Arch Interv Med 162:329–336
Detrenis S, Meschi M, Musini S, Savazzi G (2005) Lights and shadows on the pathogenesis of contrast-induced nephropathy: state of the art. Nephrol Dial Transpl 20:1542–1550
Romano G, Briguori C, Quintavalle C et al (2008) Contrast agents and renal cell apoptosis. Eur Heart J 29(20):2569–2576
Taylor AJ, Hotchkiss D, Morse RW, Mc Cabe J (1998) PREPARED: preparation for angioplasty in renal dysfunction—a randomized trial of inpatient vs outpatient hydratation protocols for cardiac catheterization in mild to moderate renal dysfunction. Chest 114:1570–1574
Solomon R, Werner C, Mann D et al (1994) Effects of saline, mannitol, and furosemide to prevent acute decreases in renal function induced by radiocontrast agents. N Engl J Med 331(21):1416–1420
Bagshaw SM, Ghali WA (2005) Theophylline for prevention of contrast-induced nephropathy: a systematic review and meta-analysis. Arch Intern Med 165(10):1087–1093
Stone GW, McCullough PA, Tumlin JA et al (2003) Fenoldopammesylate for the prevention of contrast-induced nephropathy: a randomized controlled trial. JAMA 290(17):2284–2291
Nallamothu BK, Shojania KG, Saint S et al (2004) Is acetylcysteine effective in preventing contrast-related nephropathy? A meta-analysis. Am J Med 117(12):938–947
Zagler A, Azadpour M, Mercado C, Hennekens CH (2006) N-Acetylcysteine and contrast-induced nephropathy: a meta-analysis of 13 randomized trials. Am Heart J 151(1):140–145
Maioli M, Toso A, Leoncini M et al (2008) Sodium bicarbonate versus saline for the prevention of contrast-induced nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. JACC 52:599–604
Acknowledgments
We express our gratitude to all the nurses of the Cardiac Catheterization Laboratory of the Division of Cardiology, Monaldi Hospital, for the technical support and cooperation, particularly Mrs Gabriella Lettieri, Mrs Annunziata Orefice, Mrs Marina Battista, Mrs Patrizia Sannino, Mrs Angela Auriemma and Mr Pasquale Canzanella.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calabrò, P., Bianchi, R., Crisci, M. et al. Use and efficacy of saline hydration and N-acetyl cysteine to prevent contrast-induced nephropathy in low-risk populations undergoing coronary artery angiography. Intern Emerg Med 6, 503–507 (2011). https://doi.org/10.1007/s11739-011-0513-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0513-y