Abstract
Background
A worrying increase of gastroesophageal reflux disease (GERD) and Barrett esophagus has been reported after sleeve gastrectomy (SG). Recent reports on combined fundoplication and SG seem to accomplish initial favorable results. However, no study included manometry or pH monitoring to evaluate the impact of fundoplication in SG on esophageal physiology.
Method
In this study, 32 consecutive bariatric patients with GERD and/or esophagitis had high-resolution impedance manometry (HRiM) and combined 24-h pH and multichannel intraluminal impedance (MII-pH) before and after laparoscopic sleeve gastrectomy associated to anterior fundoplication (D-SLEEVE). The following parameters were calculated at HRiM: lower esophageal sphincter pressure and relaxation, peristalsis, and mean total bolus transit time. The acid and non-acid GER episodes were assessed by MII-pH, symptom index association (SI), and symptom-association probability (SAP) were also analyzed.
Results
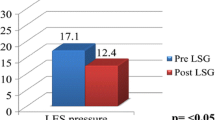
At a median follow-up of 14 months, HRiM showed an increased LES function, and MII-pH showed an excellent control of both acid exposure of the esophagus and number of reflux events. Bariatric outcomes (BMI and EWL%) were also comparable to regular SG (p = NS).
Conclusion
D-SLEEVE is an effective restrictive procedure, which recreates a functional LES pressure able to control and/or prevent mild GERD at 1-year follow-up.








Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
04 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11695-021-05244-w
References
Angrisani L, Santonicola A, Hasani A, et al. Five-year results of laparoscopic sleeve gastrectomy: effects on gastroesophageal reflux disease symptoms and co-morbidities. Surg Obes Relat Dis. 2016;12(5):960–8. https://doi.org/10.1016/j.soard.2015.09.014.
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Helvetius M. Observation sur le estomac de la Homme. Historie de l'Accademie Royale des Sciences. 1719; p. 337–45.
Soricelli E, Casella G, Baglio G, et al. Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy. Surg Obes Relat Dis. 2018;14(6):751–6.
Braghetto I, Korn O. Late esophagogastric anatomic and functional changes after sleeve gastrectomy and its clinical consequences with regards to gastroesophageal reflux disease. Dis Esophagus. 2019;32(6). https://doi.org/10.1093/dote/doz020.
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019;29:1462–9.
Doulami G, Triantafyllou S, Natoudi M, et al. 24-h multichannel intraluminal impedance pHmetry 1 year after laparoscopic sleeve gastrectomy: an objective assessment of gastroesophageal reflux disease. Obes Surg. 2017;27:749–53.
Sharma A, Aggarwal S, Ahuja V, et al. Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy. Surg Obes Relat Dis. 2014;10:600–5.
Braghetto I, Gonzalez P, Lovera C, et al. Duodenogastric biliary reflux assessed by scintigraphic scan in patients with reflux symptoms after sleeve gastrectomy: preliminary results. Surg Obes Relat Dis. 2019;S1550-7289(19):30100–5. https://doi.org/10.1016/j.soard.2019.03.034.
Del Genio G, Tolone S, Limongelli P, et al. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24(1):71–7. https://doi.org/10.1007/s11695-013-1046-4.
Foschi D, De Luca M, Sarro G, Bernante P, Zappa MA, Moroni R, Navarra G, Foletto M, Ceriani V, Piazza L, Di Lorenzo N. Linee Guida di Chirurgia dell’Obesità. Ed. Società Italiana di Chirurgia dell’Obesità e delle Malattie Metaboliche (S.I.C.OB.), 2016.
Del Genio G, Tolone S, Del Genio F, et al. Impact of total fundoplication on esophageal transit: analysis by combined multichannel intraluminal impedance and manometry. J Clin Gastroenterol. 2012;46(1):e1–5.
Pizza F, Rossetti G, Limongelli P, et al. Influence of age on outcome of total laparoscopic fundoplication for gastroesophageal reflux disease. World J Gastroenterol. 2007;13(5):740.
Shikora SA, Kim JJ, Tarnoff ME, et al. Laparoscopic Roux-en-Y gastric bypass: results and learning curve of a high-volume academic program. Arch Surg. 2005;140(4):362–7.
Genta RM, Spechler SJ, Kielhorn AF. The Los Angeles and Savary-Miller systems for grading esophagitis: utilization and correlation with histology. Dis Esophagus. 2011;24:10–7.
Amato G, Limongelli P, Pascariello A, et al. Association between persistent symptoms and long-term quality of life after laparoscopic total fundoplication. Am J Surg. 2008;196(4):582–6.
Del Genio G, Limongelli P, Del Genio F, et al. Sleeve gastrectomy improves obstructive sleep apnea syndrome (OSAS): 5 year longitudinal study. Surg Obes Relat Dis. 2016;12(1):70–4. https://doi.org/10.1016/j.soard.2015.02.020.
Tolone S, Limongelli P, del Genio G, et al. Gastroesophageal reflux disease and obesity: do we need to perform reflux testing in all candidates to bariatric surgery? Int J Surg. 2014;12:173–7.
del Genio G, Tolone S, Rossetti G, et al. Objective assessment of gastroesophageal reflux after extended Heller myotomy and total fundoplication for achalasia with the use of 24-hour combined multichannel intraluminal impedance and pH monitoring (MII-pH). Dis Esophagus. 2008;21(7):664–7. https://doi.org/10.1111/j.1442-2050.2008.00847.x.
Tutuian R, Vela MF, Balaji NS, et al. Esophageal function testing with combined multichannel intraluminal impedance and manometry: multicenter study in healthy volunteers. Clin Gastroenterol Hepatol. 2003;1(3):174–82.
Tolone S, Savarino E, Zaninotto G, et al. High-resolution manometry is superior to endoscopy and radiology in assessing and grading sliding hiatal hernia: a comparison with surgical in vivo evaluation. United European Gastroenterol J. 2018;6(7):981–9. https://doi.org/10.1177/2050640618769160.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(10):160–74.
del Genio G, Tolone S, Rossetti G, et al. Total fundoplication does not obstruct the esophageal secondary peristalsis: investigation with pre- and postoperative 24-hour pH-multichannel intraluminal impedance. Eur Surg Res. 2008;40(2):230–4.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett's esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74. https://doi.org/10.1016/j.soard.2016.11.029.
Chiu S, Birch DW, Shi X, et al. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7(4):510–5.
Deitel M, Gagner M, Erickson AL, et al. Third international summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;7(6):749–59.
Kleidi E, Theodorou D, Albanopoulos K, et al. The effect of laparoscopic sleeve gastrectomy on the antireflux mechanism: can it be minimized? Surg Endosc. 2013;27(12):4625–30. https://doi.org/10.1007/s00464-013-3083-4.
Himpens J, Dapri G, Cadière GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16(11):1450–6.
Nocca D, Skalli EM, Boulay E, et al. Nissen sleeve (N-sleeve) operation: preliminary results of a pilot study. Surg Obes Relat Dis. 2016;12(10):1832–7. https://doi.org/10.1016/j.soard.2016.02.010.
Sánchez-Pernaute A, Talavera P, Pérez-Aguirre E, et al. Technique of Hill’s gastropexy combined with sleeve gastrectomy for patients with morbid obesity and gastroesophageal reflux disease or hiatal hernia. Obes Surg. 2016;26(4):910–2. https://doi.org/10.1007/s11695-016-2076-5.
Olmi S, David G, Cesana G, et al. Modified sleeve gastrectomy combined with laparoscopic Rossetti fundoplication and vascularization assessment with Indocyanine green. Obes Surg. 2019;29:3086–8. https://doi.org/10.1007/s11695-019-03970-w.
Moon RC, Teixeira AF, Jawad MA. Safety and effectiveness of anterior fundoplication sleeve gastrectomy in patients with severe reflux. Surg Obes Relat Dis. 2017;13(4):547–52. https://doi.org/10.1016/j.soard.2016.10.008.
Olmi S, Caruso F, Uccelli M, et al. Laparoscopic sleeve gastrectomy combined with Rossetti fundoplication (R-sleeve) for treatment of morbid obesity and gastroesophageal reflux. Surg Obes Relat Dis. 2017;13(12):1945–50.
Rossetti G, del Genio G, Maffettone V, et al. Laparoscopic reoperation with total fundoplication for failed Heller myotomy: is it a possible option? Personal experience and review of literature. Int Surg. 2009;94(4):330–4.
Gagner M, Kemmeter P. Comparison of laparoscopic sleeve gastrectomy leak rates in five staple-line reinforcement options: a systematic review. Surg Endosc. 2019;34:396–407. https://doi.org/10.1007/s00464-019-06782-2.
Demeusy A, Sill A, Averbach A. Current role of staple line reinforcement in 30-day outcomes of primary laparoscopic sleeve gastrectomy: an analysis of MBSAQIP data, 2015-2016 PUF. Surg Obes Relat Dis. 2018;14(10):1454–61. https://doi.org/10.1016/j.soard.2018.06.024.
Del Genio GM, Collard JM. Acute complications of antireflux surgery. In: Ferguson MK, Fennerty MB, editors. Managing failed anti-reflux therapy. London: Springer Verlag; 2006. p. 67–77.
Karamanakos SN, Vagenas K, Kalfaretzos F. Weight loss, appetite suppression and changes in fasting and postprandial ghrelin and peptide-YY levels after roux-en-Y gastric bypass and sleeve gastrectomy a prospective, double blind study. Ann Surg. 2008;247:401–7.
Dimitriades E, Daskalakis M, Kampa M, et al. Alterations in gut hormones following laparoscopic sleeve gastrectomy [published online ahead of print October 26, 2012]. Ann Surg. https://doi.org/10.1097/SLA.0b013e31826e1846.
Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy-a “food limiting” operation. Obes Surg. 2008;18(10):1251–6.
Oor JE, Roks DJ, Ünlü Ç, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethics Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
del Genio, G., Tolone, S., Gambardella, C. et al. Sleeve Gastrectomy and Anterior Fundoplication (D-SLEEVE) Prevents Gastroesophageal Reflux in Symptomatic GERD. OBES SURG 30, 1642–1652 (2020). https://doi.org/10.1007/s11695-020-04427-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04427-1