Abstract
Background
Since 2014, the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) has produced an annual report of all bariatric surgery submitted to the Global Registry. We describe baseline demographics of international practice from the 4th report.
Methods
The IFSO Global Registry amalgamated data from 51 different countries, 14 of which provided data from their national registries. Data were available from 394,431 individual records, of which 190,177 were primary operations performed since 2014.
Results
Data were submitted on 72,645 Roux en Y gastric bypass operations (38.2%), 87,467 sleeve gastrectomy operations (46.0%), 14,516 one anastomosis gastric bypass procedures (7.6%) and 9534 gastric banding operations (5.0%) as the primary operation since 2014. The median patient body mass index (BMI) pre-surgery was 41.7 kg m2 (inter-quartile range: 38.3–46.1 kg m2). Following gastric bypass, 84.1% of patients were discharged within 2 days of surgery; and 84.5% of sleeve gastrectomy patients were discharged within 3 days. Assessing operations performed between 2012 and 2016, at one year after surgery, the mean recorded percentage weight loss was 28.9% and 66.1% of those taking medication for type 2 diabetes were recorded as not using them. The proportion of patients no longer receiving treatment for diabetes was highly dependent on weight loss achieved. There was marked variation in access and practice.
Conclusions
A global description of patients undergoing bariatric surgery is emerging. Future iterations of the registry have the potential to describe the operated patients comprehensively.
Similar content being viewed by others
Introduction
With international prevalence increasing year on year, and corresponding increases in the burden of related disease, it is clear that obesity is a problem that has to be addressed [1, 2]. Although bariatric surgery has been demonstrated to be a safe, effective and sustainable method of weight loss with associated reduction of obesity-related disease [3, 4], it is only performed on a very small percentage of patients who could benefit from it [5].
Bariatric surgery has the potential to improve health, in a cost-effective manner, to a large number of patients. However, accessibility to surgery varies within and between countries. Some information has been gleaned by worldwide surveys of practice of bariatric surgeons, but overall, little is still known about the demographics and trends of patients being operated on around the world [6,7,8,9,10,11]. Thus, although the surveys demonstrate the different kinds of operations and changes in practice over time in different regions, data on patient-related factors such as age, gender, body mass index (BMI) and obesity-related disease, for example type 2 diabetes and hypertension, are lacking. In addition, there is limited information on variation in surgical outcomes including length-of-stay or reduction in BMI or effect on obesity-related diseases on a national or international basis.
In an effort to answer some of these questions, the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) developed a Global Registry, in association with a software and analysis provider, Dendrite Clinical Systems Ltd., aiming to create a global estimate of bariatric surgery practice. The Global Registry has reported on its findings for the last 4 years [12,13,14,15]. In this 4th report, the number of individual patient records has doubled the information available compared to the third report, together with a near doubling in the number of national registries submitting data [14, 15]. In this paper, we summarise the findings of the 4th international analysis of outcomes from bariatric and metabolic surgery.
Methods
National societies were invited by the IFSO President Dr. Jacques Himpens to participate in the Global Registry as previously detailed [16] and a 4th report was commissioned for distribution at the IFSO World Congress in Dubai 2018 [15]. The Dendrite Intellect Web database technology platform, an Upload-My-Data web portal and a Direct Data Entry system were used to upload and merge the data. Data were submitted from over 550 hospitals in 51 countries spanning 5 continents, including data from 14 national registries.
Descriptive statistics were used for the analysis of the data. The contributors were reassured that no statistical comparison would be attempted between different units or countries. Data presented in graphs define the number of “valid” records, indicating the number of records where obesity-related disease could be ascertained and cases with “no data”, the number of cases unavailable for subgroup analysis.
The dataset, defined by a committee for the 1st report, has since been extended slightly, for instance to include explicitly one anastomosis gastric bypass as a procedure distinct from Roux en Y bypass. The dataset for the current version 4.1 is shown (Table 1) [16]. All operations entered up until 4th July 2018 were included in the analysis. All data presented are in relation to primary procedures. Operative data are presented from 2014 to 2018; follow-up data are presented from 2012 to 2016 to account for the inevitable lag in data capture.
Results
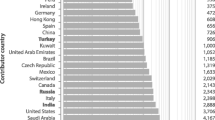
The registry contained 394,431 individual operation records at the time of last data submission. Numbers of participating countries, national registries, individual centres and submitted cases have steadily increased year on year (Table 2). The number of records submitted ranged greatly from 10 from a single centre to over 80,000 submitted by the Italian national registry (Table 3). We do not have complete country-data on case ascertainment.
The majority of the database records fell in the period 2009–2018 (88.5% of the total) although some countries have submitted data from procedures prior to 2000; 190,177 of primary operations were dated in the calendar years 2014–2018. Forty-six percent of the baseline records were > 80% complete in data submitted in the calendar years 2014–2018. Variation in data completion for the whole registry is presented (Table 4).
Patient Demographics
The following baseline analyses relate to primary operations in the calendar years 2014–2018. The overall proportion of female patients was 73.7% (95% CI: 73.5–73.9%). Although operations were more common in females in all countries, there was also a wide variation in the gender ratios, ranging from 50.9% female in Georgia (55/108) to 93.4% female in Guadeloupe (183/196). For the 16 countries with ≥ 1000 submitted patients, the gender ratios were 57.7% female (India; n = 11,088) to 79.4% female (Netherlands; n = 37,818).
The median BMI pre-surgery was 41.7 kg m2 (inter-quartile range: 38.3–46.1 kg m2); there was a wide variation between different contributor countries, with medians ranging from 34.2 kg m2 in South Korea to 49.1 kg m2 in Germany (Fig. 1a). The median age at time of operation was 42 years (inter-quartile range: 33–51 years; Fig. 1b) There was variation between countries with a trend to Middle Eastern and Asian countries having a younger, or adolescent practice, with those in the West more commonly operating at an older age. For the 16 countries with ≥ 1000 submitted patients, the BMI range was 37.3 (China; n = 1939) to 44.5 (Saudi Arabia; n = 2119).
Obesity-Related Disease Prior to Surgery
As expected, a large proportion of patients had obesity-related disease. There was large variation in the reported rates of these conditions between countries. Overall, those on medication for type 2 diabetes made up 19.8% of patients (inter-country variation: 4.5–97.7%); 30.6% were treated for hypertension (10.9–92.6%) and 12.4% of patients were on medication for depression (0.0–54.4%). Also, 24.3% of patients reported requiring treatment for musculoskeletal pain (0.0–65.1%); 18.6% of patients had diagnosed sleep apnea (0.0–74.3%); and 17.0% of patients had gastro-esophageal reflux disease (0.0–54.8%). Amongst those countries with ≥ 1000 submitted patients, the respective figures were 19.5% (9.8–43.5%) for type 2 diabetes, 30.2% (15.5–46.3%) for hypertension, 12.5% (0.6–29.1%) for depression, 24.6% (0.0–50.4%) for musculoskeletal pain, 18.4% (0.0–36.8%) for sleep apnea and 17.0% (6.4–40.7%) for GERD. The variation in disease prevalence between regions is shown (Fig. 2a, b).
Stratification for Operative Risk
An estimate of operative risk as determined by the Obesity Surgery Mortality Risk Score (OSMRS) varied widely by country (Fig. 3) [17]. Georgia, Bulgaria and Hong Kong had the highest risk patient populations (OSMRS groups B and C: 78.7%, 72.2% and 66.7%, respectively); South Korea, Bolivia and Kuwait show the least risk (OSMRS groups B and C: 12.5%, 20.5% and 22.2%).
Operation Type
Almost all, 99.3%, operations were performed laparoscopically. In the time period of this analysis, there were 72,645 Roux en Y gastric bypass operations (38.2%), 87,467 sleeve gastrectomy operations (46.0%), 14,516 one anastomosis gastric bypass procedures (7.6%) and 9534 gastric banding operations (5.0%). Although in the whole registry Roux en Y gastric bypass is the most recorded operation, in the last 2years, the number of sleeve gastrectomies recorded is greater than the number of Roux en Y gastric bypasses.
Mexico (205/253, 81.0%), Colombia (282/356, 79.2%) and Brazil (595/808, 73.6%) reported the highest proportions of gastric bypass surgery; Australia (284/284, 100.0%), Saudi Arabia (2122/2122, 100.0%) and Guadeloupe (196/197, 99.5%) reported the highest rates of sleeve gastrectomy operations. Those figures may represent local, rather than national practice since, of these countries, only Brazil submitted data from a national registry. Region variation in operation type is displayed in Fig. 4 and Table 5.
Length of Stay
The vast majority of patients who had a gastric band inserted were discharged within 1 day of their operation (88.5%); gastric bypass patients within 2 days of surgery (84.1%); and sleeve gastrectomy patients within 3 days (84.5%). This variation in trends was marked between different regions with the shortest lengths of stay being in North America (single-centre data; Fig. 5).
One-Year Follow Up
For the 184,871 primary operations recorded between 2012 and 2016, 116,431 had follow-up records (63.0%). One-year follow-up was more complete in those patients having Roux en Y gastric bypass than sleeve gastrectomy (57.4% vs 29.4%). Variation in attainment of follow-up data for the Roux en Y gastric bypass group is shown (Table 6).
Over all types of surgery, the average recorded percentage weight loss was 28.9% a year after surgery: 30.0% for Roux en Y; 29.1% for gastric sleeve; 16.1% for gastric band; and 32.9% for one anastomosis gastric bypass. As would be expected, the percentage weight loss at 1 year was greater in those with a higher initial BMI (Fig. 6a).
One year after primary surgery, 66.1% of those taking medication for type 2 diabetes beforehand were no longer on medication; the proportion of patients no longer treated for diabetes was highly dependent on weight loss achieved, with the rate of improvement increasing with higher percentage weight loss (Fig. 6b).
Discussion
This dataset derived from the continuing IFSO Global Registry gives an extensive and unique overview of practice in bariatric surgery, demonstrating variations in patient and operation selection in different countries. If the datasets submitted by national registries have accurate case ascertainment, then it is likely that they represent accurately the practice in each country. However, the IFSO Global Registry has no mechanism to check case ascertainment, submission of incomplete or erroneous data, and it is assumed that each submitting society provides this validation. The same assumption is made for all individual hospital submissions. Future iterations of the dataset could include a question about whether the data have been validated before submission. However, even in small datasets, the data submitted appear consistent with known parameters in that country: the number of patients submitted from Germany in this report is only 22 but their median BMI is similar to that of the known caseload in that country [18].
To enable high levels of participation and compliance with the Global Registry, the dataset has purposefully been kept short and minimal, predominantly in the form of ‘Yes/No’ questions. However, the simplicity of the data collected may miss important outcomes, and it is not in line with recommendations on standardised bariatric surgery outcomes reporting [19]. There is a fine balance between the two approaches to achieve a comprehensive, detailed database with true case attainment: there is more work to be done to achieve the perfect equilibrium.
We noted that the overall completion of the baseline dataset was 63%. Differences in how registries are set up, for instance the lack of ‘Yes/No’ answers to identify the absence of surgical complications, may account for some apparent incompleteness. Recently, the Swedish and Norwegian SOReg and the Dutch registry DATO have demonstrated that sharing data elements between registries can allow accurate cross-comparison of surgical complications, an important initiative towards quality assurance between different countries [20]. Qualitative assurance and improvement projects might be a future goal of the IFSO Global Registry. However, thus far, the project has been limited to a description of baseline demographics and 1-year outcomes so as to encourage continuing data submission and recognising the inherent challenges of data validation as described above. In the future, standardising a minimum bariatric dataset could be a goal for national registries and local databases worldwide.
Although this year, the number of national registries submitting data has increased to 14, there are still large areas of the world whose data are unknown. Other countries have large comprehensive registries: in the USA, the MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) is a large collaboration between the American College of Surgeon and the ASMBS (American Society for Metabolic and Bariatric Surgery) and the resulting Participant Use Data File (PUF) is released periodically for independent analysis by participating centres. Recent reports from the 2015 PUF provide baseline demographic descriptions that are complementary to the data presented here [21,22,23]. Many countries have data submitted from only a single centre, which means that this may only reflect local practice rather than national trends. Continued efforts to recruit new centres and obtaining data from existing, and developing, national registries will strengthen the description of baseline demographics in patients operated worldwide.
The data collected via the Global Registry mirror the operative trends of the 2016 international survey of practice [11]. The international survey obtains a wider coverage of complete countries than is obtained by the Global Registry; however, where no national registry is available, these numbers may be estimated. In addition, the Global Registry collects a greater depth of data, with patient variables and outcome data within the limitation of the dataset. The estimated international number of operations performed in 2016 was 634,897. This suggests at this time around 7.5% of all international operations are being logged on the global registry, an increase from previous years [16].
Even though the overall attainment of 1-year follow-up data has increased, weight loss and diabetes status are the only variables retrieved with sufficient frequency to allow meaningful comparison, with 32.5% and 23.3% of cases with follow-up, respectively. [16] We note the differences in captured follow-up for patients with diabetes having gastric bypass (41.1%) and sleeve gastrectomy (11.9%). The reasons for this are unknown, but might be due to different follow-up data submitted by the geographically separate centres doing these operations. Also, the data presented in the full 4th report show some promising trends in improvement of hypertension, sleep apnea, depression, and musculoskeletal pain, but with follow-up records available for fewer than 10% of cases, no conclusions can be drawn from these findings [15]. A challenge for this and all registries is how to achieve better follow-up data.
One of the benefits of such a registry enables us in real time to appreciate the changes in practice, initially with the rise in popularity of the sleeve gastrectomy, and now with an emerging increase in the number of one anastomosis gastric bypass operations being performed. Such understanding can help us focus our research questions to make them relevant, as demonstrated by the By-Band study which evolved to become the By-Band-Sleeve randomised controlled trial in the UK, as the number of sleeve gastrectomies performed increased. [24]
Limitations of the paper include lack of generalizability due to incomplete case ascertainment, and inability to assess incomplete or erroneous data submission, as well as incomplete follow-up data. In addition to the limitations of the Yes/No questions, there is unknown selection bias for those patients with recorded follow-up. Swedish, Norwegian and Dutch surgeons have shown that it is possible to amalgamate large datasets with the aim of demonstrating differences in mortality and complication rates between different countries. [20] Over time, future iterations of the IFSO Global Registry might be able to achieve this on a much wider scale. If this became possible, the bariatric community would be able to demonstrate further the safety of bariatric/metabolic surgery on a generalizable basis.
In summary, there is a wide variation in bariatric practice internationally with sleeve gastrectomy now the most commonly performed bariatric procedure. The burden of obesity-related disease in the operated populations is high but varies greatly between regions. Worldwide, bariatric surgery provides marked weight loss and remission of diabetes at 1 year. Further data are needed to show the effect on other obesity-related diseases.
References
Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. 2015;66(Suppl 2):7–12.
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–81.
Colquitt JL, Pickett K, Loveman E. Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014:CD003641.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Welbourn R, Hopkins J, Dixon JB, et al. Commissioning guidance for weight assessment and management in adults and children with severe complex obesity. Obes Rev. 2018;19:14–27.
Scopinaro N. The IFSO and obesity surgery throughout the world. International Federation for the Surgery of obesity. Obes Surg. 1998;8:3–8.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64.
Angrisani L, Santonicola A, Iovino P, et al. Primary, Endoluminal, and Revisional procedures. Obes Surg. 2016;2018
Welbourn R, Gagner M, Naslund I, Ottosson J, Kinsman R, Walton P. First IFSO Global Registry Report 2014. Dendrite clinical systems ltd, Henley-on-Thames, RG9 1AY, UK 2014.
Welbourn R, Dixon J, Higa K, Kinsman R, Ottosson J, Ramos A. Second IFSO Global Registry Report 2016. Dendrite Clinical Systems Ltd, Henley-on-Thames, RG9 1AY, UK ISBN 978–0–9929942-1-1 2016.
Higa K, Himpens J, Welbourn R, Dixon J, Kinsman R, Walton P. Third IFSO Global Registry Report 2017. Dendrite Clinical Systems Ltd, Henley-on-Thames, RG9 1AY, UK ISBN 978–0–9929942-4-2 2018.
Himpens J, Ramos A, Welbourn R, Kinsman R, Walton P. Fourth IFSO Global Registry Report 2018. Dendrite Clinical Systems Ltd, Henley-on-Thames, RG9 1AY, UKISBN 978–0–9929942-7-3 2018.
Welbourn R, Pournaras DJ, Dixon J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the second IFSO global registry report 2013-2015. Obes Surg. 2018;28:313–22.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3:134–40.
Stroh C, Weiner R, Wolff S, et al. Are there gender-specific aspects in obesity and metabolic surgery? Data analysis from the German bariatric surgery registry. Viszeralmedizin. 2014;30:125–32.
Brethauer SA, Kim J, El Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25:587–606.
Poelemeijer YQM, Liem RSL, Vage V, Mala T, Sundbom M, Ottosson J, et al. Perioperative outcomes of primary bariatric surgery in North-Western Europe: a pooled multinational registry analysis. Obes Surg. 2018;28(12):3916–22.
El Chaar, M, Lundberg P, Stoltzfus J. Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass: first report based on metabolic and bariatric surgery accreditation and quality improvement program database. Surg Obes Rel Dis. 2018;14:545–53.
Janik MR, Mustafa RR, Rogula TG, Alhaj Saleh A, Abbas M, Khaitan L. Safety of laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass in elderly patients - analysis of the MBSAQIP. Surg Obes Relat Dis. 2018;14(9):1276–82.
Kumar SB, Hamilton BC, Wood SG, et al. Is laparoscopic sleeve gastrectomy safer than laparoscopic gastric bypass? A comparison of 30-day complications using the MBSAQIP data registry. Surg Obes Relat Dis. 2018;14:264–9.
Rogers CA, Reeves BC, Byrne J, et al. Adaptation of the by-band randomized clinical trial to by-band-sleeve to include a new intervention and maintain relevance of the study to practice. Br J Surg. 2017;104:1207–14.
Funding
The IFSO Global Registry Fourth Report was funded by the International Federation for Surgery for Obesity and Metabolic Disorders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Conflict of Interest
Dr. Welbourn reports non-financial support for attending conferences from Ethicon Endo-Surgery, personal fees from consultancy fees from Novo Nordisk, outside the submitted work.
Dr. Cohen reports personal fees from GI Dynamics, grants from Johnson & Johnson Medical, Brazil, outside the submitted work.
Dr. Dixon reports personal fees from NHMRC, during the conduct of the study; personal fees from Apollo Endosurgery, personal fees from Bariatric Advantage, personal fees from Medrontic, personal fees from Nestle, personal fees from Johnson & Johnson, outside the submitted work.
Dr. Himpens reports personal fees from Ethicon, personal fees from Medtronic, outside the submitted work.
Dr. Walton and Dr. Kinsmen reports grants from IFSO, during the conduct of the study; grants from IFSO, outside the submitted work. Dr. Hollyman, Dr. Liem, Dr. Brown, Dr. Ottosson, Dr. Ramos, Dr. Alsabah, and Dr. Våge have nothing to disclose.
Additional information
Richard Welbourn and Marianne Hollyman are joint first authors
Rights and permissions
About this article
Cite this article
Welbourn, R., Hollyman, M., Kinsman, R. et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Fourth IFSO Global Registry Report 2018. OBES SURG 29, 782–795 (2019). https://doi.org/10.1007/s11695-018-3593-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3593-1