Abstract
Background
The purpose of this study was to demonstrate the relationship between the surgical approach employed for adults undergoing bariatric surgery for obesity in New York State and in-hospital postoperative complications. Understanding the differences among surgical approaches in terms of the type, extent, and likelihood of postoperative complications and the patient characteristics associated with them, particularly as the annual volume of bariatric surgery increases, can inform decisions about the appropriate bariatric surgical approach for patients with particular characteristics.
Methods
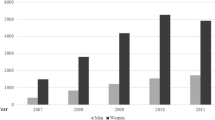
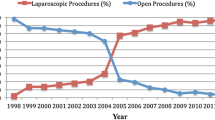
Using New York’s inpatient hospital discharge database, we identified 8,413 adults who underwent a bariatric surgical procedure during calendar year 2006. The three most common bariatric surgical approaches were identified, postoperative complication rates and descriptive statistics for the demographic characteristics and comorbidities for patients of each surgical approach were generated, and a logistic regression model was constructed to predict the likelihood of postoperative complications.
Results
Of all bariatric surgical patients, 8.1% experienced a postoperative complication, but complication rates varied dramatically across the surgical approaches, with open bypass patients having the highest complication rate and laparoscopic banding patients having the lowest rate. Different complications were associated with the three surgical approaches, as were the various patient demographic characteristics and comorbidities. The multivariate logistic regression indicated that open bypass patients were 5.4 times and laparoscopic bypass patients were 3.2 times more likely to experience a complication compared to laparoscopic banding patients.
Conclusion
Analyses of bariatric postoperative surgical complications must take into account the surgical approach employed.
Similar content being viewed by others
References
Ogden CL, Carroll MD, Curtin LL. Prevalence of overweight and obesity in the US, 1999–2004. JAMA 2006;295:1549–55.
Ezzati M, Martin H, Skjold S. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. Jr Soc Med 2006;99:250–7.
Christon NV, Sampalis JS, Liberman M. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240:416–24.
MacDonald KG, Long SD, Swanson MS. The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg 1997;1:213–20.
Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg 2004;199:543–51.
Sowemimo OA, Yood SM, Courtney J. Natural history of morbid obesity without surgical intervention. Surg Obes Relat Dis 2007;3:73–7.
Peeters A, O’Brien P, Laurie C. Does weight loss improve survival? Comparison of a bariatric surgical cohort with a community based control group. Obes Rev 2006;7 Suppl 2:95. (Abstract OP0193).
Busetto L, Mazza M, Mirabellie D. Total mortality in morbid obese patients treated with laparoscopic adjustable banding: a case–control study. Obese Rev 2006;7 Suppl 2:95. (Abstract OP0194).
Mottin CC, Padoin AV, Schroer CE. Behavior of type 2 diabetes mellitus in morbid obese patients submitted to gastric bypass. Obes Surg 2008;18:179–81.
Sjostrom L, Lindroos AK, Petonen M. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Eng J Med 2004;351:2683–93.
Anderson T, Backer OG, Stokholm KH. Randomized trial of diet and gastroplasty compared with diet alone in morbid obesity. N Eng J Med 1984;310:352–6.
Anderson T, Stokholm KH, Backer OG. Long-term (5 year) results after either horizontal gastroplasty or very-low-calorie diet for morbid obesity. Int J Obes 1988;12:277–84.
Sjostrom CD, Peltonen M, Sjostrom L. Blood pressure and pulse pressure during long-term weight loss in the obese: the Swedish Obese Subjects (SOS) Intervention Study. Obes Res 2001;9:188–95.
Liu JH, Zingmond D, Etzioni DA. Characterizing the performance and outcomes of obesity surgery in California. Am Surg 2003;69:823–8.
Livingston EH. Procedure incidence and in-hospital complication rates of bariatric surgery in the United States. Am J Surg 2004;188:105–10.
Trus TL, Pope GD, Finlayson RG. National trends in utilization and outcomes of bariatric surgery. Surg Endosc 2005;19:616–20.
Pope GD, Birkmeyer JD, Finlayson RG. National trends in utilization and in-hospital outcomes of bariatric surgery. J Gastrointest Surg 2002;6:855–61.
Courcoulas A, Schuchert M, Gatti G. The relationship of surgeon and hospital volume to outcome after gastric bypass surgery in Pennsylvania: a 3-year summary. Surgery 2003;134:613–23.
Mason EE, Renquist KE, Jiang D. Perioperative risks and safety of surgery for severe obesity. Am J Clin Nutr 1992;55:5735–65.
Livingston EH, Huerta S, Arthur D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg 2002;236:576–82.
Livingston EH, Langert J. The impact of age and Medicare status on bariatric surgical outcomes. Arch Surg 2006;141:1115–20.
Weller WE, Rosati C, Hannan EL. Predictors of in-hospital postoperative complications among adults undergoing bariatric procedures in New York State, 2003. Obes Surg 2006;16:702–8.
Mehrotra C, Serdula M, Naimi TS. Population based study of trends, costs, and complications of weight loss surgeries from 1990 to 2002. Obesity Res 2005;13:2029–34.
Saunders J, Ballantyne G. 30 day readmission rates at a high volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass and vertical banded gastroplasty Roux-en-Y gastric bypass. Obes Surg 2007;17:1171–7.
Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA 2005;294:1918–24.
Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg 2007;204:383–91.
Shekelle PG, Morton SC, Maglione MA, et al. Pharmacological and surgical treatment of obesity. Evidence Report/Technology Assessment No. 103 (prepared by the Southern-California-Rand Evidence-Based Practice Center, Santa Monica, CA, under contract number 290-02-0003.) AHRQ Publication No. 04-E028-2. Rockville, MD: Agency for Healthcare Research and Quality. July 2004.
Buchwald H, Avidor Y, Braunwald E. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–37.
Maggard MA, Shugarman LR, Suttorp M. Meta-analysis: surgical treatment of obesity. Ann Intern Med 2005;142:547–59.
Fernandez A, Demaria E, Tichansky D. Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesity. Ann Surg 2004;239:698–703.
Angrisani L, Lorenzo M, Borrelli V. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 5 year results of a prospective randomized trial. Surg Obes Relat Dis 2007;3:127–32.
Buchwald H. Consensus conference statement, bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis 2005;1:371–81.
Parikl MS, Laker J, Weiner M. Objective comparison of complications resulting from laparoscopic bariatric procedures. J Am Coll Surg 2006;202:252–61.
Elixhauser A, Syeiner C, Harris D. Co-morbidity measures for use with administrative data. Med Care 1998;36:8–27.
Puzziferri N, Austrheim-Smith BS, Wolfe BM. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg 2006;243:181–8.
Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci 2006;331:219–25.
Ren CJ, Cabrera I, Rajaram K. Factors influencing patient choice for bariatric operation. Obes Surg 2005;15:202–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author commercial interest: The authors have no financial interests or interest of any kind in the surgical approaches described in this paper.
Rights and permissions
About this article
Cite this article
Lindsey, M.L., Patterson, W.L., Gesten, F.C. et al. Bariatric Surgery for Obesity: Surgical Approach and Variation in In-Hospital Complications in New York State. OBES SURG 19, 688–700 (2009). https://doi.org/10.1007/s11695-009-9812-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-9812-z