Abstract
Background
Transient hyperglycemia is commonly observed in non-diabetic subjects during surgery. We undertook this study to investigate (1) insulin secretion pattern and glucose levels during elective surgery, and (2) the role of pre-operative fasting in the development of surgery-induced hyperglycemia.
Methods
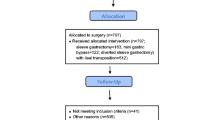
We examined 21 severely obese normal glucose tolerant patients, who underwent bariatric surgery. From the 21 operated subjects, 14 remained fasted while seven patients received 75 g glucose the preoperative night. They sampled at baseline and from the onset of operation frequently for 9 h thereafter, for measuring serum insulin and glucose.
Results
Hyperglycemia developed within 1 h from the onset of operation and lasted 9 h. The administration of 75 g glucose the preoperative night prevented surgery-induced hyperglycemia. Insulin profile analyzed by deconvolution analysis was similar between fasted patients and those who received 75 g glucose. Serum insulin was suppressed at the beginning of the surgery and reached baseline values 4 h thereafter.
Conclusion
Hyperglycemia occurred within 1 h from the beginning of surgery and sustained for at least 9 h while insulin levels are suppressed or unaltered compared to baseline values in euglycemia. The administration of 75 g glucose the preoperative night prevents surgery-induced hyperglycemia without altering the profile of insulin secretion.




Similar content being viewed by others
References
Van den Berghe G, Zegher F, Bouilion R. Acute and prolonged critical illness as different neuroendocrine paradigms. J Clin Endocrinol Metab. 1998;83:1827–34.
Langouche L, Van den Berghe G. The dynamic neuroendocrine response to critical illness. Endocrinol Metab Clin N Am. 2006;35:777–91.
Wartofsky L, Burman KD. Alterations in thyroid function in patients with systemic illness: the “euthyroid sick syndrome”. Endocr Rev. 1982;3:164–217.
Fliers E, Alkemade A, Wiersinga WM. The hypothalamic–pituitary–thyroid axis in critical illness. Best Pract Res Clin Endocrinol Metab. 2001;15:453–64.
Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care. 1999;2:69–78.
Ljungqvist O, Nygren J, Thorell A. Insulin resistance and elective surgery. Surgery. 2000;128:757–60.
Mizock BA. Alterations in fuel metabolism in critical illness: hyperglycaemia. Best Pract Res Clin Endocrinol Metab. 2001;15:533–51.
Pei D, Chen TW, Kuo YL, Hung YJ, Hsieh CH, Wu LY, et al. The effect of surgical stress on insulin sensitivity, glucose effectiveness and acute insulin response to glucose load. J Endocrinol Invest. 2003;26:397–402.
Halter JB, Pflug AE. Relationship of impaired insulin secretion during surgical stress to anesthesia and catecholamine release. J Clin Endocrinol Metab. 1980;51:1093–8.
Rizza RA, Mandarino LJ, Gerich JE. Cortisol-induced insulin resistance in man: impaired suppression of glucose production and stimulation of glucose utilization due to a postreceptor defect in insulin action. J Clin Endocrinol Metab. 1982;54:131–8.
Shamon H, Hendler R, Sherwin RS. Synergistic interactions among antiinsulin hormones in the pathogenesis of stress hyperglycemia in humans. J Clin Endocrinol Metab. 1981;52:1235–41.
Grimble RF. Inflammatory status and insulin resistance. Curr Opin Clin Nutr Metab Care. 2002;5:551–9.
Lang CH, Dobrescu C, Bagby GL. Tumor necrosis factor impairs insulin action on peripheral glucose disposal and hepatic glucose output. Endocrinology. 1992;130:43–52.
Mehta VK, Hao W, Brooks-Worell BM, Palmer JP. Low dose interleukin I and tumor necrosis factor individually stimulate insulin release but in combination cause suppression. Eur J Endocrinol. 1994;130:208–14.
Van den Berghe G. How does blood glucose control with insulin save lives in intensive care? J Clin Invest. 2004;114:1187–95.
Clarke RS. The hyperglycaemic response to different types of surgery and anaesthesia. Br J Anaesth. 1970;42:45–53.
Goschke H, Bar E, Girard J, Leutenegger A, Niederer W, Oberholzer M, et al. Glucagon, insulin, cortisol, and growth hormone levels following major surgery: their relationship to glucose and free fatty acid elevations. Horm Metab Res. 1978;10:465–70.
Allison SP, Prowse K, Chamberlain MJ. Failure of insulin response to glucose load during operation and after myocardial infarction. Lancet. 1967;1:478–81.
Giddings AE, Mangnall D, Rowlands BJ, Clark RG. Plasma insulin and surgery. I. Early changes due to operation in the insulin response to glucose. Ann Surg. 1977;186:681–6.
Aarimaa M, Syvalahti E, Viikari J, Ovaska J. Insulin, growth hormone and catecholamines as regulators of energy metabolism in the course of surgery. Acta Chir Scand. 1978;144:411–22.
Ljungqvist O, Thorell A, Gutniak M, Haggmark T, Efendic S. Glucose infusion instead of preoperative fasting reduces postoperative insulin resistance. J Am Coll Surg. 1994;178:329–36.
Thorell A, Alston-Smith J, Ljungqvist O. The effect of preoperative carbohydrate loading on hormonal changes, hepatic glycogen, and glucoregulatory enzymes during abdominal surgery. Nutrition. 1996;12:690–5.
Soop M, Nygren J, Myrenfors P, Thorell A, Ljungqvist O. Preoperative oral carbohydrate treatment attenuates immediate postoperative insulin resistance. Am J Physiol Endocrinol Metab. 2001;280:576–83.
Soop M, Nygren J, Thorell A, Weidenhielm L, Lundberg M, Hammarqvist F, et al. Preoperative oral carbohydrate treatment attenuates endogenous glucose release 3 days after surgery. Clin Nutr. Aug 2004;23(4):733–41.
Nygren J, Soop M, Thorell A, Efendic S, Nair KS, Ljungqvist O. Preoperative oral carbohydrate administration reduces postoperative insulin resistance. Clin Nutr. 1998;17:65–71.
Cahill GF Jr. Starvation in man. N Engl J Med. 1970;282:668–75.
Association AD. Screening for diabetes. Diabetes Care. 2002;25:S21–4.
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10.
Veldhuis JD, Carlson ML, Johnson ML. The pituitary gland secretes in bursts: appraising the nature of glandular secretory impulses by simultaneous multiple-parameter deconvolution of plasma hormone concentrations. Proc Natl Acad Sci U S A. 1987;84:7686–90.
Porksen N, Nyholm B, Veldhuis JD, Butler PC, Schmitz O. In humans at least 75% of insulin secretion arises from punctuated insulin secretory bursts. Am J Physiol. 1997;273:E908–14.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci U S A. 1991;88:2297–301.
Veldhuis JD, Straume M, Iranmanesh A, Mulligan T, Jaffe C, Barkan A, et al. Secretory process regularity monitors neuroendocrine feedback and feedforward signaling strength in humans. Am J Physiol Regul Integr Comp Physiol. 2001;280:R721–9.
Black PR, Brooks DC, Bessey PQ, Wolfe RR, Wilmore DW. Mechanisms of insulin resistance following injury. Ann Surg. 1982;196:420–35.
Thorell A, Nygren J, Hirshman MF, Hayashi T, Nair KS, Horton ES, et al. Surgery-induced insulin resistance in human patients: relation to glucose transport and utilization. Am J Physiol. 1999;276:E754–61.
Nygren J, Thorell A, Efendic S, Nair KS, Ljungqvist O. Site of insulin resistance after surgery: the contribution of hypocaloric nutrition and bed rest. Clin Sci (Lond). 1997;93:137–46.
Fellander G, Nordenstrom J, Tjader I, Bolinder J, Arner P. Lipolysis during abdominal surgery. J Clin Endocrinol Metab. 1994;78:150–5.
Nakao K, Miyata M. The influence of phentolamine, an adrenergic blocking agent, on insulin secretion during surgery. Eur J Clin Invest. 1977;7:41–5.
Lattermann R, Schricker T, Wachter U, Goertz A, Georgieff M. Intraoperative epidural blockade prevents the increase in protein breakdown after abdominal surgery. Acta Anaesthesiol Scand. 2001;45:1140–6.
Brodner G, Van Aken H, Hertle L, Fobker M, Von Eckardstein A, Goeters C, et al. Multimodal perioperative management-combining thoracic epidural analgesia, forced mobilization, and oral nutrition-reduces hormonal and metabolic stress and improves convalescence after major urologic surgery. Anesth Analg. 2001;92:1594–600.
Suttner S, Lang K, Piper SN, Schultz H, Rohm KD, Boldt J. Continuous intra- and postoperative thoracic epidural analgesia attenuates brain natriuretic peptide release after major abdominal surgery. Anesth Analg. 2005;101:896–903.
Michalaki M, Vagenakis AG, Makri M, Kalfarentzos F, Kyriazopoulou V. Dissociation of the early decline in serum T(3) concentration and serum IL-6 rise and TNFalpha in nonthyroidal illness syndrome induced by abdominal surgery. J Clin Endocrinol Metab. 2001;86:4198–205.
Stewart P. Glucocorticoid hormone action. In: Larsen P, Kroneberg H, Melmed S, Polonsky K, editors. Williams text book of endocrinology, 10 edn. ch. 14. Saunders, Philadelphia; 2003. p. 503–6.
Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67.
Burroughs V, Weinberger J. Diabetes and stroke: part two-treating diabetes and stress hyperglycemia in hospitalized stroke patients. Curr Cardiol Rep. 2006;8:29–32.
Gentile NT, Seftchick MW, Huynh T, Kruus LK, Gaughan J. Decreased mortality by normalizing blood glucose after acute ischemic stroke. Acad Emerg Med. 2006;13:174–80.
Cheung NW, Wong VW, McLean M. The hyperglycemia: intensive insulin infusion in infarction (HI-5) study: a randomized controlled trial of insulin infusion therapy for myocardial infarction. Diabetes Care. 2006;29:765–70.
Malmberg K, Ryden L, Efendic S, Herlitz J, Nicol P, Waldenstrom A, et al. Randomized trial of insulin–glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year. J Am Coll Cardiol. 1995;26:57–65.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
Brunkhorst F, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michalaki, M., Kyriazopoulou, V., Mylonas, P. et al. Glucose Levels and Insulin Secretion in Surgery-Induced Hyperglycemia in Normoglycemic Obese Patients. OBES SURG 18, 1460–1466 (2008). https://doi.org/10.1007/s11695-008-9501-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9501-3